Sample
A total of 9,515 depressed patients entered the study. The final sample for analysis consisted of 8,229 patients (86.48%). Subjects were excluded if the Hospital Anxiety and Depression Scale score was below 8 for depression or anxiety (644 patients) or data characterizing the patient were not correctly or completely saved. The subsample of subjects excluded 1) had fewer DSM-IV symptoms of depression (t=4.25, df=9512, p<0.0001); 2) had a shorter length of the present episode (t=2.15, df=6798, p=0.0159); 3) were more frequently men (χ 2 =172.9, df=8, p<0.0001); and 4) had better final Hospital Anxiety and Depression Scale scores for depression (t=3.974, df=9512, p<0.0001) and anxiety (t=5.212, df=9512, p<0.0001), and thus they were more frequently responders (χ 2 =3.71, df=1, p=0.0124).
Women comprised 70.37% of the final sample, and the average age of the sample was 48.02 years (SD=14.09). In this population, 1,115 patients were 65 years old or older, and 407 patients were over 75 years old. Civil status among these patients was as follows: married, 48.37%; single, 15.41%; divorced, 15.57%; and widowed, 7.31%. Education levels (middle=high school graduate) were as follows: low, 49.10%; middle, 30.06%; and high, 20.84%. Employment status was as follows: active employment, 57.86%; unemployed, 12.43%; retired, 19.07%; student, 0.11%; and another type of professional activity, 10.53%.
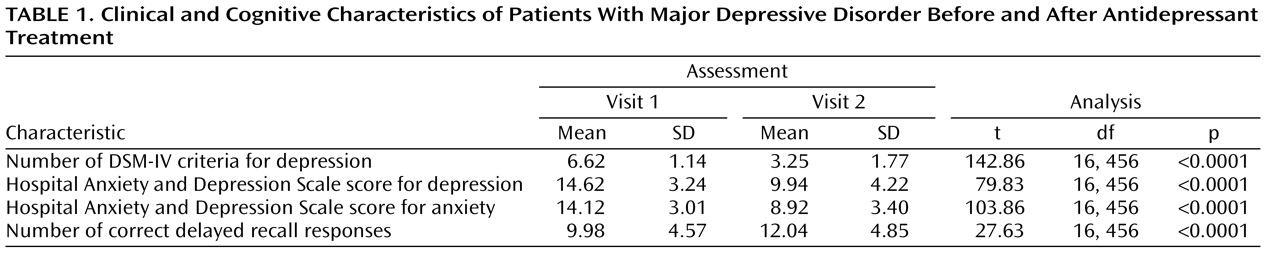
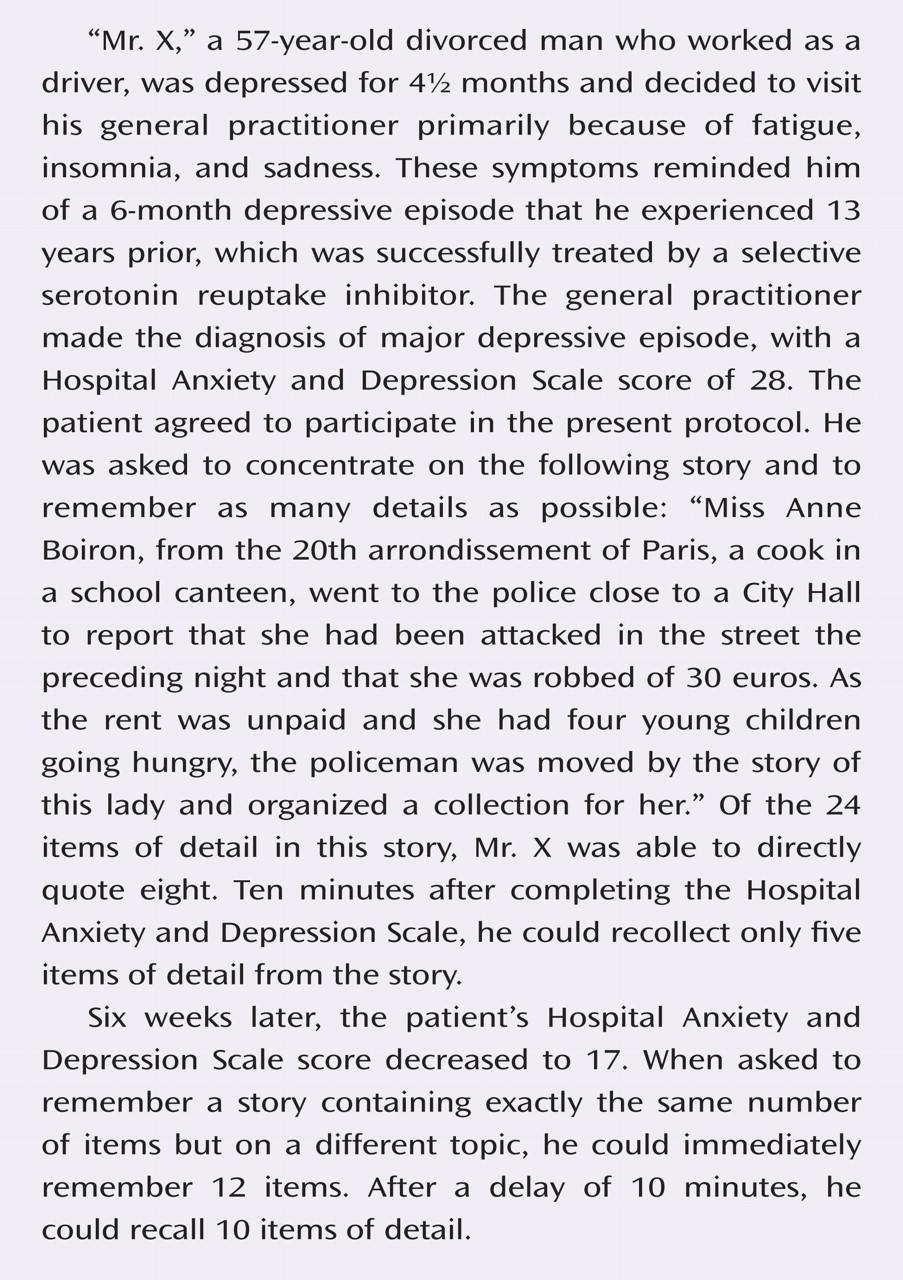
The Hospital Anxiety and Depression Scale score for depression was below 11 in only 10.48% of patients. The duration of current major depressive episode was on average 8.37 weeks (SD=10.84). Among the patients, 18.38% fulfilled five DSM-IV criteria for depression, 31.82% fulfilled six criteria, 27.76% fulfilled seven criteria, 15.44% fulfilled eight criteria, and 6.60% fulfilled nine criteria (
Table 1 ). This was the first episode of depression for 49.64% of patients, the second episode for 25.30%, the third episode for 6.05%, and between the fourth and 13th episode for the remaining patients (4.67%). The length of unipolar depression, except the present episode, was on average 12.55 weeks (SD=34.91), and the lifetime duration (or number of weeks depressed) was 21.23 weeks (SD=33.91).
The second visit was on average 42 days (SD=8.93) after the first visit (between 3 and 20 weeks). At the second visit, the number of depressive symptoms from the list of DSM-IV criteria decreased (
Table 1 ). According to these criteria, 76.39% of patients no longer fulfilled the diagnosis of major depressive episode (i.e., fulfilled less than five criteria). According to Hospital Anxiety and Depression Scale self-rating, 76.44% of patients were responders (i.e., patients who had at least a 50% decrease of the depression score between the two visits).
The number of correct answers for immediate recall of the Weschler paragraph recall index tested at the first visit was between one and 24, with an average of 11.75 appropriate answers (SD=4.72) (see the table in the data supplement accompanying the online version of this article). The delay between immediate and delayed recall was on average 14.15 minutes (SD=7.73; range=5–56). Accordingly, the delay between immediate and delayed recall was introduced into multivariate analyses, as was the delay between the first and second visits. The patients recalled approximately 10 correct details of the paragraph (i.e., 85.89% of the initial immediate recall) (
Table 1 ).
During the second visit, a global improvement of immediate recall was observed (13.24 correct answers; [SD=4.79; range=1–24]) (see the table in the data supplement accompanying the online version of this article). On average, 13.58 minutes later (SD=7.32; range=5–65), delayed recall was correct for approximately 12 items (
Table 1 ).
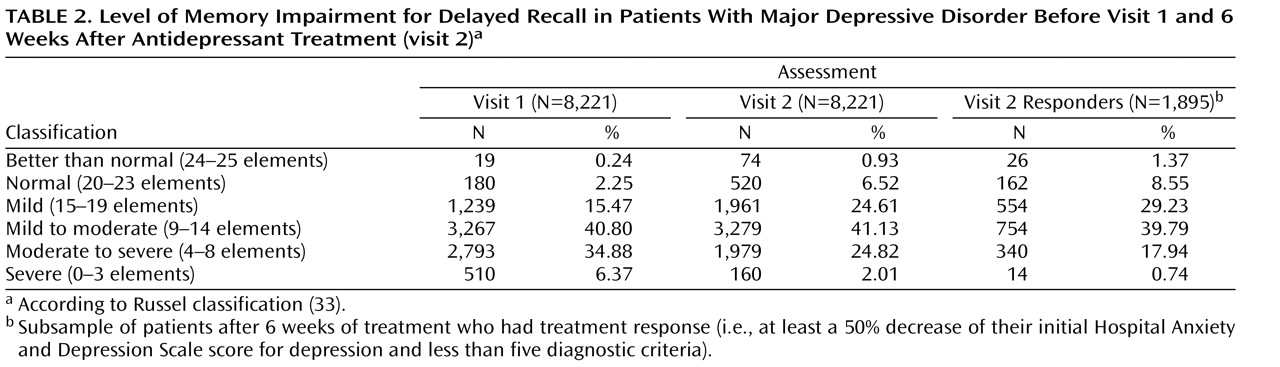
The level of memory impairment at both visits as well as in the sample of patients with treatment response at the second visit is detailed in
Table 2 .
Benzodiazepines were prescribed for 52.51% of patients, but treatment was unchanged during the entire observation period for 90.73% of patients (reflecting the short delay between the first and second visits), and the dosage was fixed for the vast majority of patients (93.30%). Nevertheless, coprescription of benzodiazepines was included in the analyses as a potential confound.
At the initial visit, the 8,229 patients who had a Hospital Anxiety and Depression Scale score above 8 for both depression and anxiety and who fulfilled DSM-IV criteria for major depressive disorder according to the clinician were tested for paragraph delayed recall.
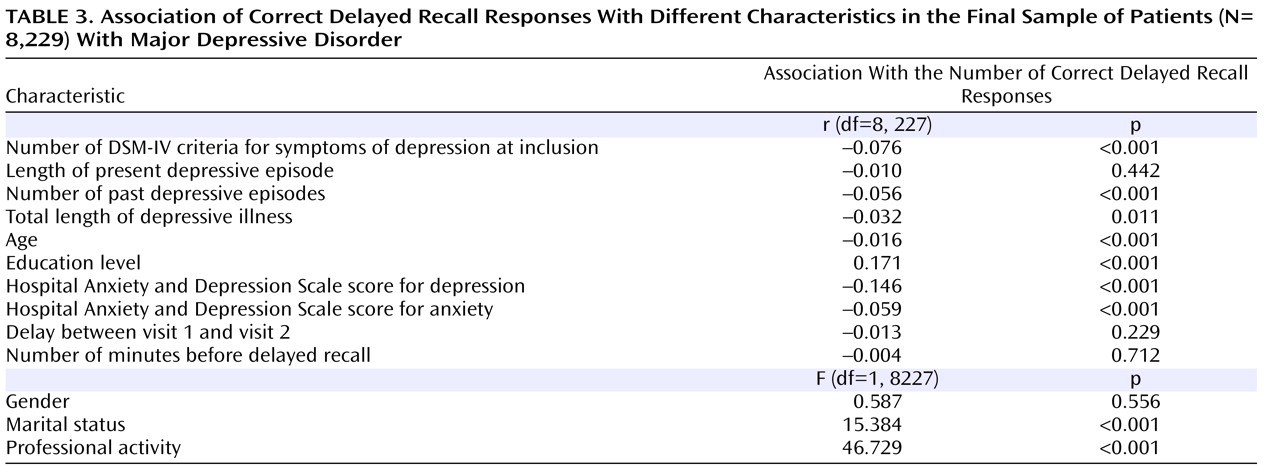
The relationship between the main variables at the first visit is presented as uncorrected correlations to aid in understanding of the data structure. The number of correct responses was significantly correlated with the following (
Table 3 ): younger age, higher education level, presence of professional activity, marital status (positive correlation), number of DSM-IV symptoms of depression, Hospital Anxiety and Depression Scale scores for depression and anxiety, and number of past episodes (negative correlation) (p<0.001). A significant but weaker negative correlation was shown for the total length of depressive episodes (p<0.012). Gender, delay between the first and second visits, and the time between immediate and delayed recall were not predictive of the number of correct delayed recall responses. When the role of depression and anxiety scores of the Hospital Anxiety and Depression Scale were analyzed separately, depression was significantly correlated with the number of correct delayed recall responses (r=–0.125, p<0.001), whereas anxiety was not (r=–0.016, p=0.579).
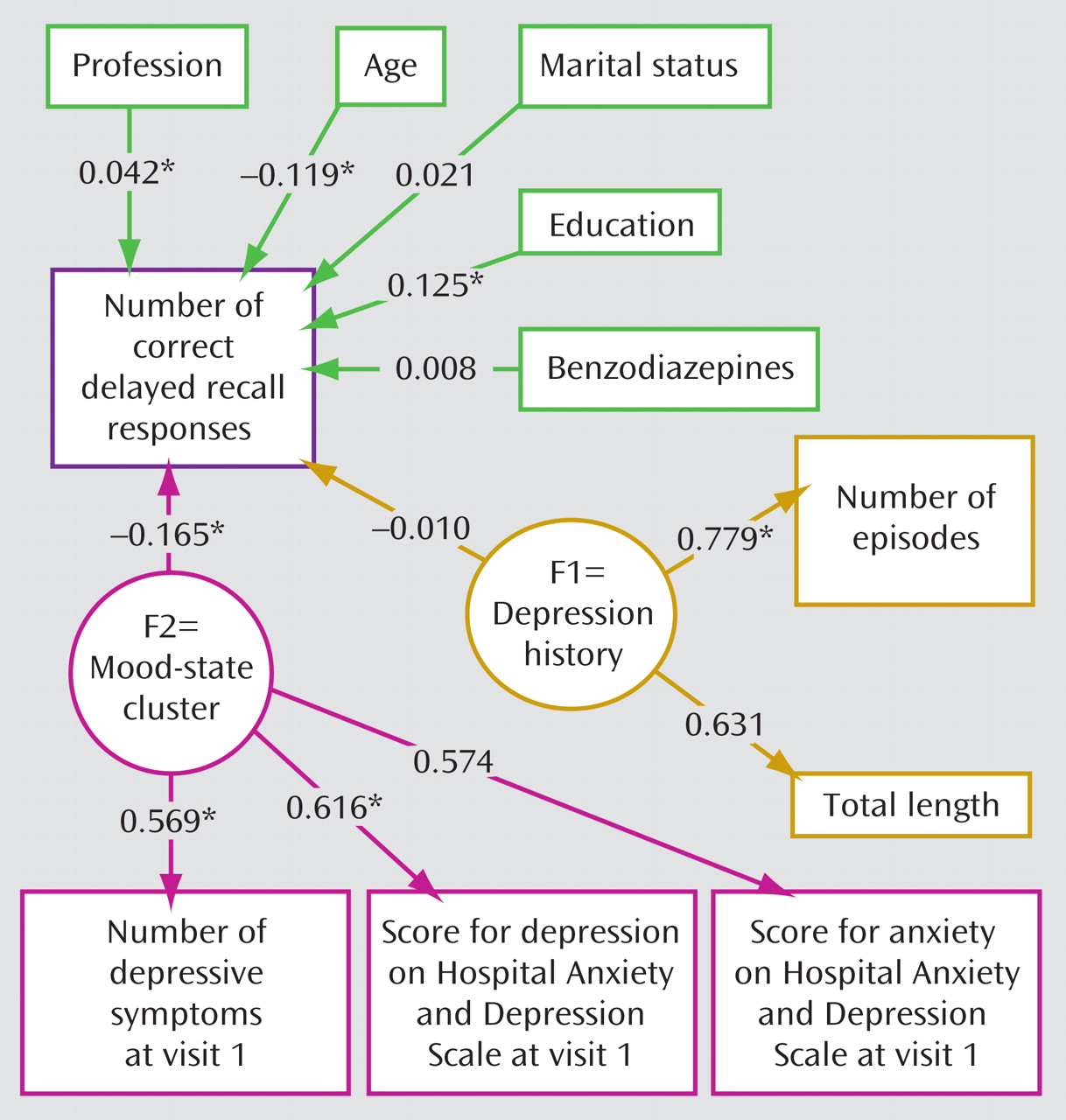
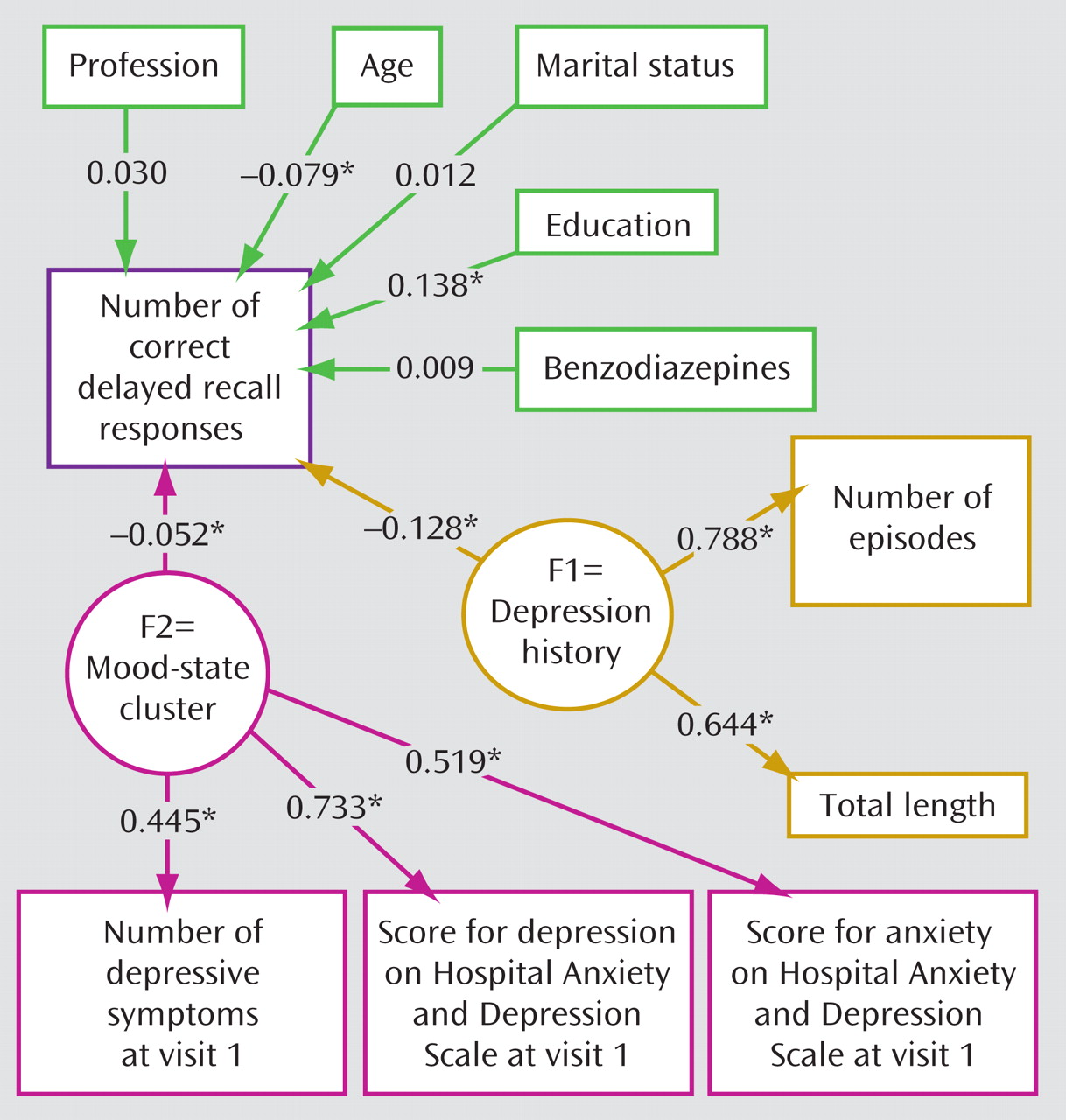
To account for the existence of different clusters of variables influencing the number of correct responses for paragraph delayed recall, structural equation modeling was performed. At the first visit, mood-state dependent variables had the largest effect on the number of correct delayed recall responses, together with smaller effects of age and level of education (
Figure 1 ). In contrast, the length and number of past episodes of major depression were noncontributory (
Figure 1 ).
The model fit was good, since the upper portion of the 95% confidence interval of the root mean square error of approximation was smaller than 0.05 (0.0436) and the Bentler and Bonnet normed fit index was higher than 0.95 (0.974).
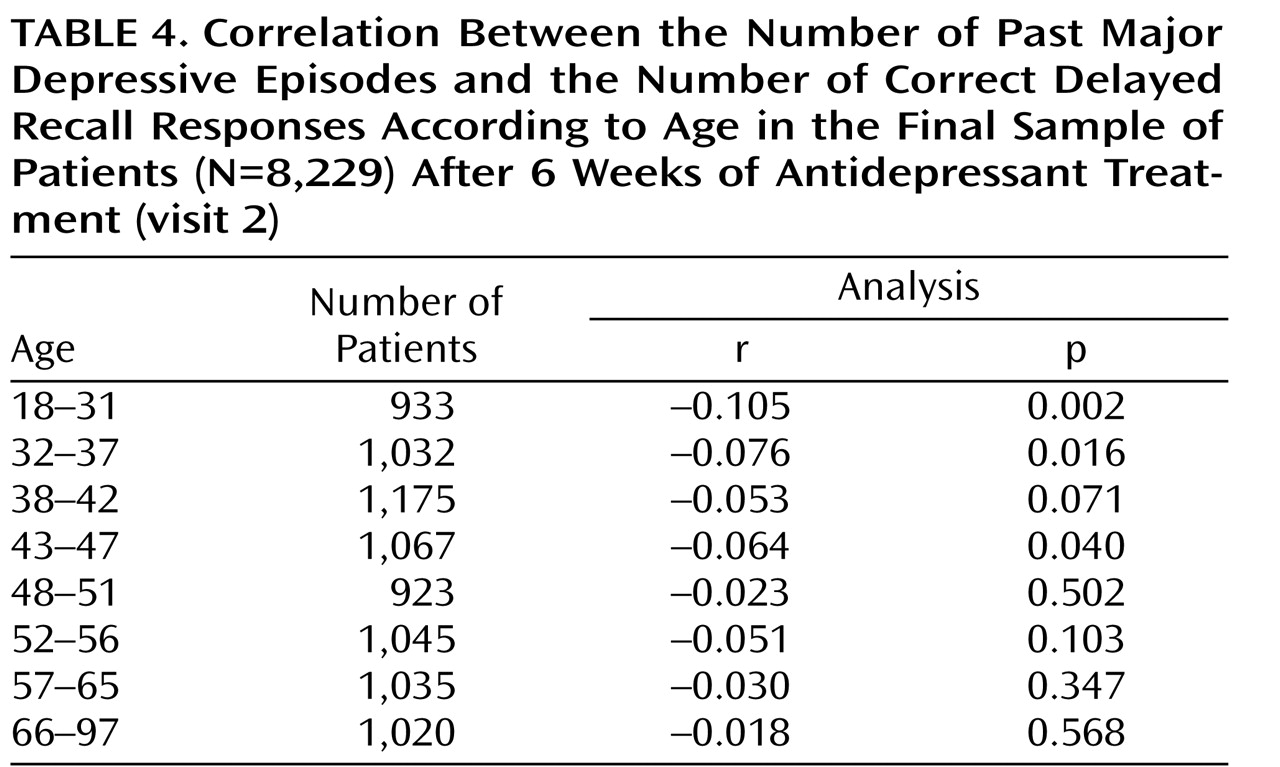
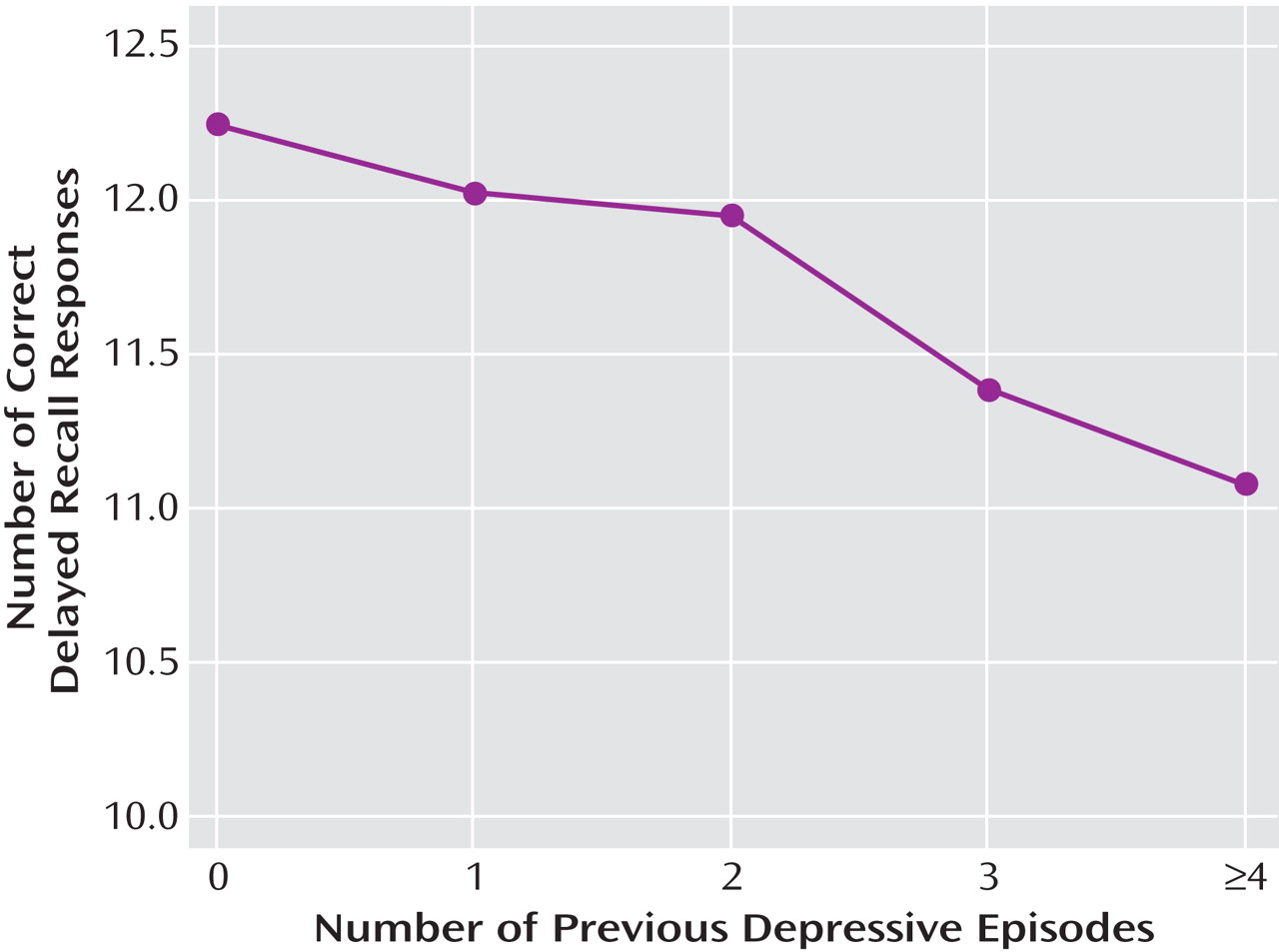
Given the changes in mood and cognitive performance at the second visit, we predicted that the role of past episodes in the second analysis would be strengthened in the subsample of patients who most fully responded. A correlation between the number of past episodes and the number of correct delayed recall responses for the final sample of analysis (N=8,229) was observed (r=–0.063, p<0.001) and was more notable in younger patients (
Table 4 ). More precisely, among those 1,895 patients whose Hospital Anxiety and Depression Scale depression score decreased by 50% at the second visit and who had less than five diagnostic criteria, the structural equation modeling showed that the number of past episodes and total length of major depressive disorder constituted a cluster that was significantly correlated with the number of correct delayed recall responses (
Figure 2 ). Thus, there was a significant relationship between past depression and memory performance as proposed in our hypothesis. Moreover, the path coefficient for the past depression cluster was substantially higher than the path coefficient observed between mood-dependent parameters (constituting the other cluster) (
Figure 2 ). None of the Hospital Anxiety and Depression Scale scores for depression and anxiety (omitting the mood-state cluster) were significantly correlated with the number of correct delayed recall responses (r=–0.052, p=0.067; r=–0.016, p=0.579, respectively).
Again, the model fit was good, with the upper portion of the 95% confidence interval of the root mean square error of approximation equal to 0.0301 and the Bentler and Bonnet normed fit index equal to 0.977. As expected, age and education remained contributory.
We then used a linear regression analysis to examine whether the correlation between the number of correct delayed recall responses and the number of past major depressive episodes was greater at the second visit relative to the first visit. The three most important variables that were significantly correlated with the number of correct delayed recall responses were 1) the visit number (visit 1 versus visit 2; F=10,400, df=15, 286, p<0.001), 2) the number of past depressive episodes (F=34.71, df=15, 286, p<0.001), and 3) the interaction between the former and latter variables (F=32.28, df=15, 286, p<0.001). Age, gender, education, and Hospital Anxiety and Depression Scale score for depression were also significantly correlated (F>6.91, df=15, 286, p<0.009).
Finally, at the first visit we examined the sample of patients who were in remission at the time of the second visit. This allowed us to analyze whether the significant role of the total length of mood disorder and number of past episodes detected in the 1,895 patients who were in remission at the second visit was obscured by current depression at the first visit. The structural equation modeling showed that the number of past episodes and total length of major depressive disorder constituted a cluster that was no longer significantly correlated with the number of correct delayed recall responses (r=–0.019, p=0.59), whereas the mood-state dependent variable was significantly predictive (r=–0.249, p<0.001). Age (r=–0.121, p<0.001) and education level (r=0.118, p<0.001) were also contributory, and the model fit was satisfying, with the upper portion of the 95% confidence interval of the root mean square error of approximation equal to 0.023 and the Bentler and Bonnet normed fit index equal to 0.972.
Omitting 510 patients at the first visit and 160 patients at the second visit (
Table 2 ) who were classified as having “severe” impairment did not significantly change the results (the state cluster was correlated [r=–128, p<0.001] with the number of correct delayed recall responses at the first visit, but the trait cluster was not [r=–0.016, p=0.185], whereas the state cluster was not correlated [r=–0.035, p=0.163] with the number of correct delayed recall responses at the second visit, but the trait cluster was correlated [r=–0.123, p<0.001]). Therefore, the initial results shown in
Figure 1 and
Figure 2 reflect a general effect and were not unduly influenced by the “severe” impairment group.