Obsessions and compulsions are the core features of obsessive-compulsive disorder (OCD) but have also been anecdotally described in other psychiatric disorders
(1,
2) as well as in individuals with no formal psychiatric diagnosis
(3) . However, the view that many individuals in the general population experience obsessions and compulsions, which is central to several theoretical models of OCD
(3,
4), is mainly based on small studies performed on convenience samples of undergraduate students
(5,
6) . Epidemiological data on obsessions and compulsions are scarce because epidemiological studies usually only report on categorical diagnoses. Prevalence estimates for obsessions and compulsions in the community have ranged between 1.5% (current)
(7) and 35% (past month)
(8), although these studies assessed a limited number of symptoms
(7) or did not take into account psychiatric disorders other than OCD
(8) .
If obsessions and compulsions were indeed frequent among individuals who do not meet criteria for OCD, it would be important to document the level of interference associated with these symptoms. In clinical OCD samples, obsessions are more strongly associated with decreased quality of life than compulsions
(9), but it is unknown whether this is true in the context of other psychiatric disorders or in the community in general. In a related vein, it is unknown how many people from the general population seek treatment due to obsessions/compulsions and what variables are associated with this help-seeking behavior.
In clinical samples, the content of OCD symptoms is heterogeneous. Factor and cluster analytical studies have consistently identified a few consistent symptom dimensions: contamination/cleaning, harm/checking, symmetry/ordering, and hoarding
(4) . These dimensions are temporally
(10) and cross-culturally
(11) stable, have distinct neural substrates
(12), and are associated with particular patterns of comorbidity
(13) . However, it is unclear whether the frequency of these particular symptom dimensions is similar in the community, whether they are temporally stable, and whether they are associated with particular comorbid disorders. Finally, little is known about the developmental stability of obsessions/compulsions and whether the presence of obsessions/compulsions in childhood is predictive of full-blown OCD later in life. If such an association existed, screening and prevention strategies might be warranted.
In the present report, we employ a prospective longitudinal design with an unselected birth cohort of individuals. Our research questions were: 1) What is the prevalence of obsessions and compulsions in the community and the associated level of interference? 2) How many people seek help for obsessions/compulsions and what predicts help-seeking behavior? 3) What is the prevalence and temporal stability of specific obsessive-compulsive symptom dimensions? 4) Are these symptom dimensions associated with particular patterns of comorbidity? 5) Is there an association between obsessive-compulsive symptoms in childhood and OCD in adulthood?
Method
Participants
Participants are members of the Dunedin Multidisciplinary Health and Development Study, a longitudinal investigation of the health and behavior of a complete cohort of children born during a one-year period in 1972–1973 in Dunedin, New Zealand. 1,037 individuals (52% male; 91% of eligible births) participated in the age 3 assessment, forming the base sample for the longitudinal study. Cohort members represent the full range of socioeconomic status in the general population of New Zealand’s South Island, and are primarily white. The Dunedin sample has been assessed at ages 3, 5, 7, 9, 11, 13, 15, 18, 21, 26, and most recently at age 32 when we saw 972 participants (96% of living cohort members). The research procedure involves bringing study members (including emigrants living overseas) to the research unit for individual interviews and tests. Written informed consent was obtained. In this article, we report about obsessions and compulsions collected at ages 11, 26 and 32.
Psychiatric Assessment at Age 11
The psychiatric assessment of Dunedin Study members has been described in detail
(14,
15) . At age 11, 792 of the 925 participants were administered the NIMH Diagnostic Interview Schedule for Children (DISC-C)
(16), based on DSM-III
(17) criteria, by a child psychiatrist
(18) . Due to scheduling constraints, one-quarter of the cohort did not see the psychiatrist. The age 11 sample represents the original birth cohort, as previously described
(18) . Obsessions and compulsions were assessed with the OCD section of the DISC-C, which asked the following questions: 1) “Do thoughts or pictures you don"t like ever come into your head?” 2) “Do you have rules about things that you have to do over and over (like not stepping on the lines in the sidewalk, or knocking on wood)?” 3) “Are there things that you always feel you have to do in exactly the same way?” 4) “Do you feel you have to count something and can"t stop even when you try to (like steps on a stairway)?” Children’s responses were probed by the psychiatrist, who then coded them as 0 (“no”), 1 (“probable”), or 2 (“yes”). We defined a group of individuals with obsessions or compulsions at age 11, which comprised all children coded “yes” to at least one of questions 1 through 4.
Psychiatric Assessment at Ages 26 and 32
At ages 26 and 32, psychiatric symptoms and disorders were assessed by means of the NIMH Diagnostic Interview Schedule (DIS-IV)
(19), which uses the DSM-IV
(20), with a reporting period of 12 months at each age. Interviewers were health professionals with tertiary qualifications and clinical experience in mental health (not lay interviewers). At ages 26 and 32, interviewers were different and blind to prior study data. Obsessions and compulsions were assessed with the OCD section of the DIS, which lists the most common types of obsessions and compulsions. We report on five types of obsessions (contamination, relatives being hurt/killed, hurting/killing someone beloved without wanting to, accidentally harming someone, and shameful thoughts) and five types of compulsions (washing, checking to prevent harm, ordering, repeating, and counting). If the study member endorsed a particular symptom, the interviewer inquired about interference using several questions about duration and distress (for obsessions: “Have these thoughts bothered you again and again over a period of at least two weeks?” “Have these thoughts often bothered you for more than one hour at a time?” “Have these thoughts caused you a lot of emotional upset or made it hard for you to do things you want to do?” For compulsions: “Did the feeling that you had to do these things last for at least two consecutive weeks?” “Did having to do these things often take you more than an hour a day?” “Have you been very upset with yourself for having to do these things?”). Help-seeking behavior in the past year due to obsessions/compulsions was also recorded.
In addition to examining individual symptoms, we also grouped symptoms at ages 26 and 32 according to four dimensions of obsessive-compulsive symptoms identified in past factor and cluster-analytical studies of clinical samples (e.g. references
4,
21 for recent reviews). Obsessive-compulsive symptom dimensions were ascertained on the basis of the endorsement of specific individual symptoms. Dimension 1 (contamination/washing) included contamination obsessions and/or washing compulsions. Dimension 2 (harm/checking) included obsessions about relatives being hurt/killed, hurting/killing someone beloved without wanting to, accidentally harming someone, and/or checking to prevent harm. Dimension 3 (symmetry/ordering) included ordering, repeating and counting compulsions. Dimension 4 (shameful thoughts) included a single item relating to “shameful” obsessions.
In addition to obsessions and compulsions, we also report about the relationship between these symptoms and other common DSM-IV mental disorders at ages 26 and 32: anxiety disorders (generalized anxiety disorder, post-traumatic stress disorder, panic disorder, agoraphobia, specific phobia, and social phobia), major depression, alcohol dependence, and drug dependence (cannabis, opiates, etc.). We defined a “no mental disorder” group at ages 26 and 32 as those who did not meet criteria for any DSM-IV disorder in the past year.
Statistical Analyses
We report prevalence rates for obsessions, compulsions, and the four symptom dimensions, as well as the percentage of individuals fulfilling interference criteria and seeking help at ages 26 and 32. We also report the association between obsessions/compulsions at age 11 and obsessive-compulsive symptom dimensions and OCD diagnosis in adulthood. Associations between variables were assessed using odds ratios with 95% confidence intervals (95% CI).
Results
Prevalence of Obsessions and Compulsions
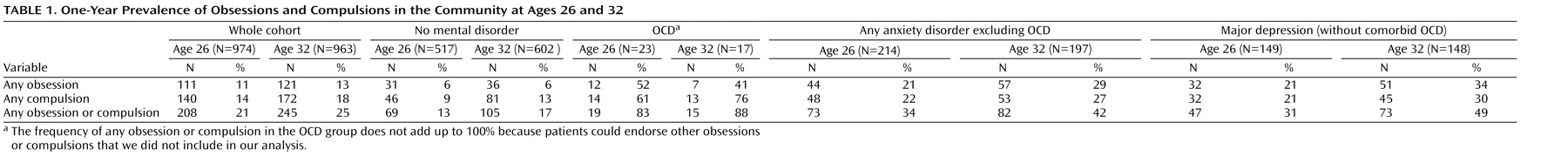
Table 1 presents the one-year prevalence rates of obsessions and compulsions (regardless of their content) for the whole cohort, for individuals with no mental disorder, for individuals who met diagnostic criteria for OCD and for individuals with the most common mental disorders (specifically, any anxiety disorder excluding OCD, and major depression without comorbid OCD) at ages 26 and 32. Obsessions and compulsions were relatively frequent among individuals with mental disorders other than OCD (31%–49%) as well as among individuals without mental disorders (13%–17%). These percentages contrast with the prevalence of categorically defined OCD according to DSM-IV criteria, which was 2.3% at age 26 and 1.8% at age 32.
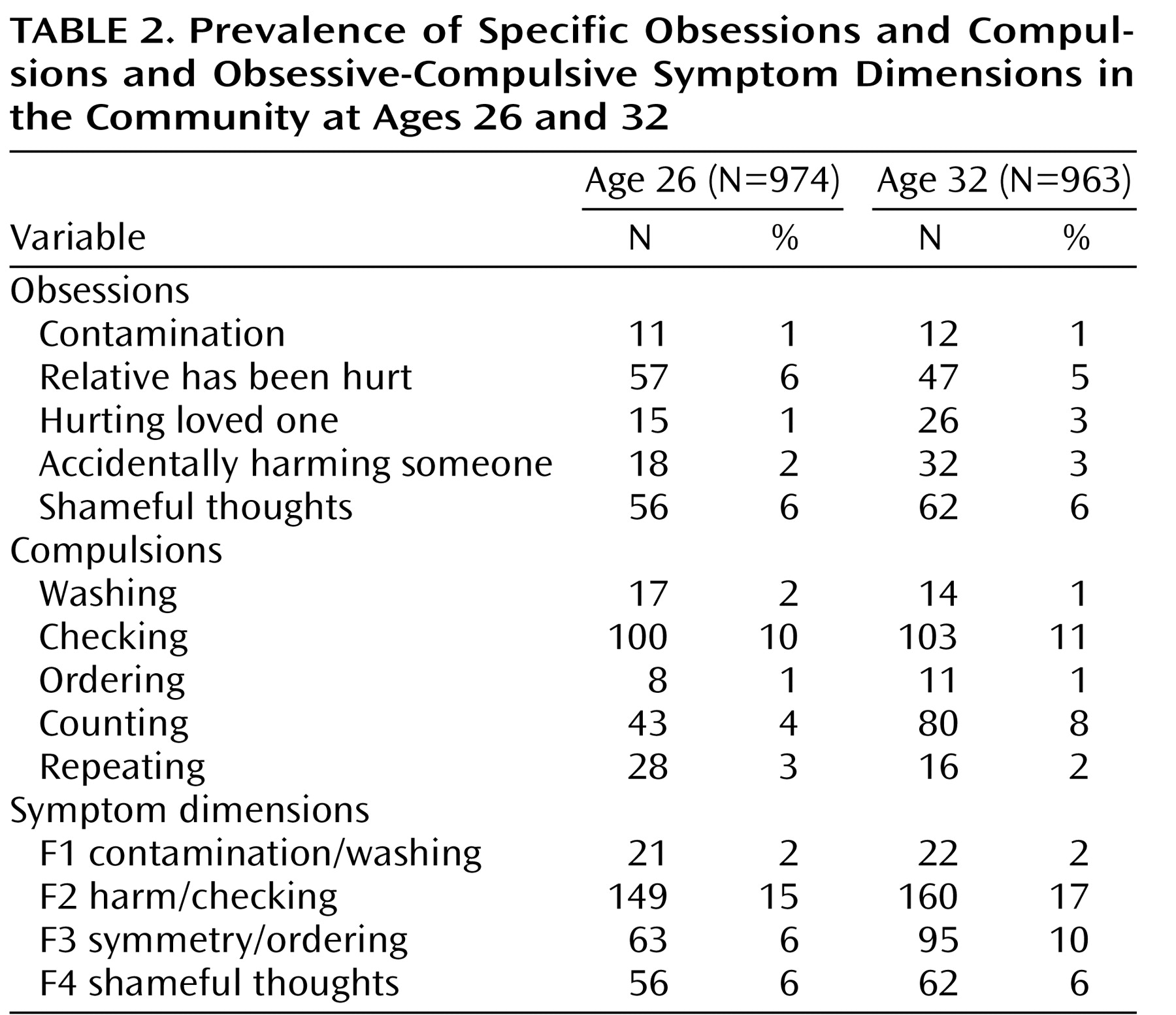
Table 2 presents the prevalence rates of specific obsessions and compulsions. Obsessions about a relative being hurt and shameful thoughts were the most frequent obsessions (5%–6% of the total sample). Checking to prevent harm was by far the most common compulsion, with 10% of the sample endorsing this symptom. Overall, the prevalence of the different obsessions and compulsions was similar at both ages 26 and 32.
Interference due to Obsessions and Compulsions
At both age periods (ages 26 and 32), and for all participant groups (no mental disorder, OCD, any anxiety disorder excluding OCD, and major depression without comorbid OCD), obsessions caused more interference than compulsions. For example, nearly 45% of study members who reported obsessions said that obsessions caused them emotional upset, whereas only 20% of study members who reported compulsions were upset by them. Of interest, 31%–42% of people with no mental disorder reported having been bothered by obsessions for periods of over 2 weeks, 25% reported experiencing obsessions for more than an hour a day, and approximately 15% reported being emotionally upset by them. Regarding compulsions, 33%–45% of the whole cohort reported performing them for periods of over 2 weeks; 11%–12% of healthy individuals reported being upset by having to perform such rituals but only one study member reported spending more than 1 hour a day performing rituals. (See data supplement at http:ajp.psychiatryonline.org.)
Help-Seeking Behavior
At age 26, 21 individuals (2% of the whole sample, 57% women) sought help for obsessions or compulsions in the previous year. Eight of these individuals (38%) had OCD; 11 (52%) had major depression, another anxiety disorder, or both; and 2 (10%) had no disorder. Five out of the eight study members meeting diagnostic criteria for OCD who sought help had comorbid major depression. Similarly, at age 32, 20 individuals (2% of the whole sample, 65% women) sought help for obsessions or compulsions. Three (15%) had OCD, 16 (80%) had major depression, another anxiety disorder or both, and 1 (5%) had no diagnosed disorder. In all, 67% of study members with OCD who sought help had comorbid major depression.
We further explored the variables that predicted help-seeking behavior for obsessions or compulsions in this cohort. At both ages, help-seeking was associated with having obsessions (age 26, odds ratio=9.46, 95% CI=3.92–22.88; age 32, odds ratio=7.75, 95% CI=2.51–23.95) but not with having compulsions (age 26, odds ratio=1.89, 95% CI=0.68–5.24; age 32, odds ratio=0.26, 95% CI=0.10–0.69). Three types of obsessions were associated with seeking help at both ages: hurting/killing someone beloved without wanting to (age 26, odds ratio=20.12, 95% CI=5.82–69.61; age 32, odds ratio=4.45, 95% CI=1.44–13.72), accidentally harming someone (age 26, odds ratio=11.16, 95% CI=2.94–42.27; age 32, odds ratio=3.73, 95% CI=1.23–11.33), and shameful thoughts (age 26, odds ratio=14.77, 95% CI=5.92–36.83; age 32, odds ratio=5.1, 95% CI=1.99–13.05).
Obsessive-Compulsive Symptom Dimensions: Prevalence, Stability, and Co-Occurring Mental Disorders
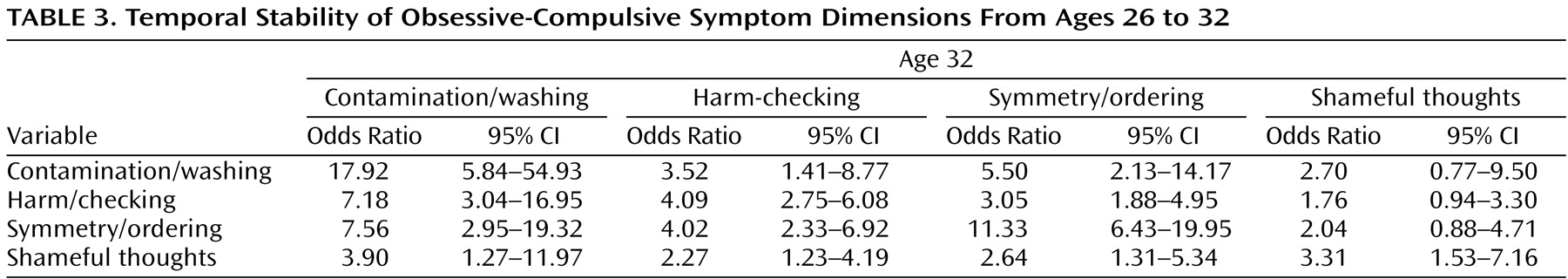
Table 2 presents the prevalence of obsessive compulsive symptom dimensions at ages 26 and 32. Prevalence rates were similar across the two ages, and the symptom dimensions were also longitudinally stable: endorsing a particular symptom dimension at age 26 significantly increased the risk of endorsing the same symptom dimension at age 32 (
Table 3 ).
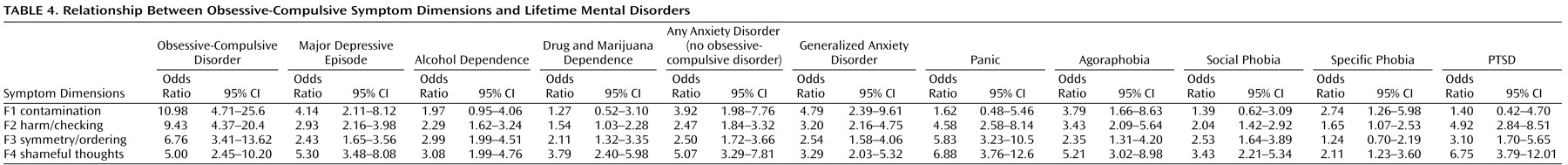
We next collapsed ages 26 and 32 for each symptom dimension and calculated associations between symptom dimensions and presence of other common mental disorders at age 26 or 32. The presence of all symptom dimensions was significantly associated with increased risk of other axis I disorders (
Table 4 ).
This association was particularly marked for the shameful thoughts dimension and weakest for the contamination/cleaning dimension.
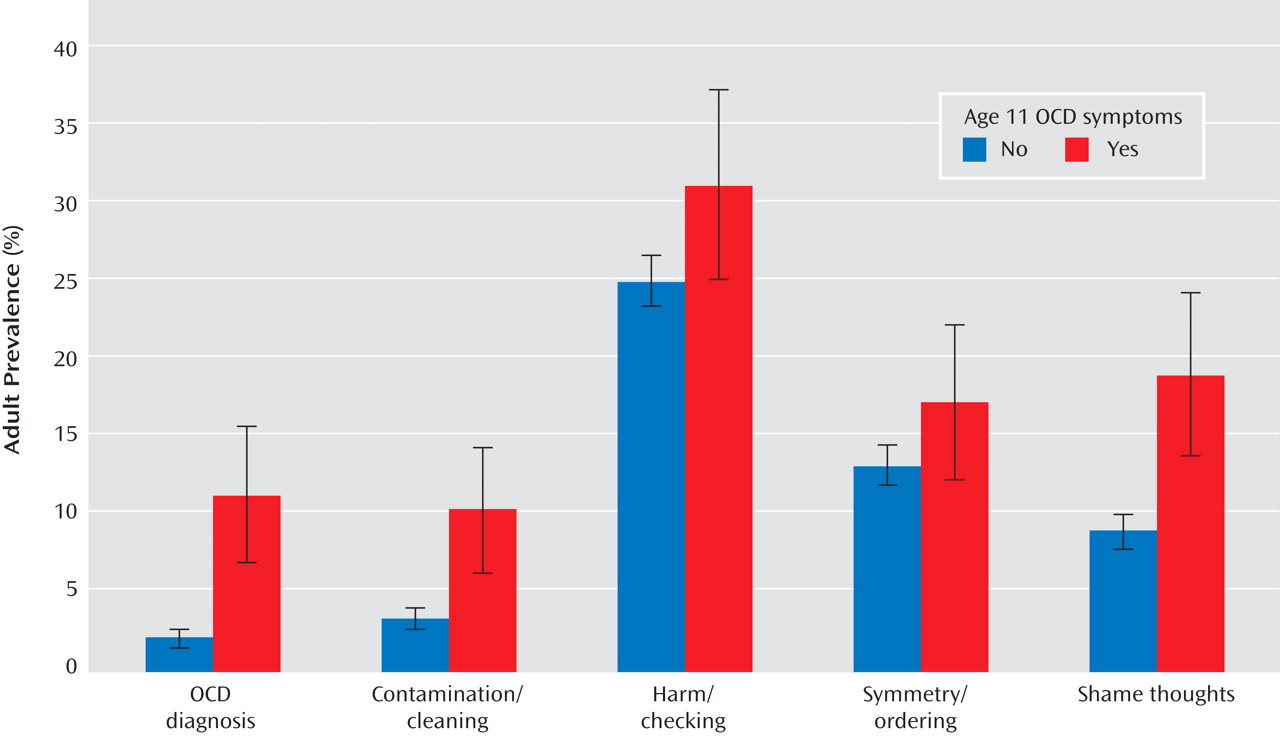
Developmental Stability
At age 11, 61 participants (8%) reported at least one obsession or compulsion. Children who reported obsessions or compulsions were significantly more likely to meet diagnostic criteria for OCD in adulthood (odds ratio=5.90, 95% CI=2.18–15.9). Furthermore, these children were significantly more likely to endorse adult symptom dimensions of contamination/cleaning (odds ratio=3.37, 95% CI=1.32–8.61) and shameful thoughts (odds ratio=2.38, 95% CI=1.17–4.81).
Figure 1 shows that although many more people experienced OCD symptoms than met diagnostic criteria for OCD in adulthood, both were developmentally linked to the same symptom precursors in childhood.
Discussion
To the best of our knowledge, this is the first study to examine the prevalence of specific obsessions and compulsions in a community sample using face-to-face structured clinical interviews. Unlike previous efforts, we were able to evaluate the prevalence of a wide range of obsessions and compulsions among individuals with different psychiatric disorders and in individuals without a psychiatric diagnosis. Due to the longitudinal nature of the study, we were also able to document that the pattern of findings regarding prevalence, interference, and help-seeking was replicated across assessments held 6 years apart, and that there are stable individual differences across adulthood in the susceptibility to experience obsessive-compulsive symptoms. Our findings also provide new evidence for continuity of obsessive-compulsive symptoms from childhood to adulthood. Seven conclusions can be drawn from the data.
First, the current results suggest that obsessions and compulsions extend beyond the traditional nosological boundaries of OCD. We estimate that 21%–25% of individuals from the general population endorse obsessions and/or compulsions, as defined in the DSM-IV, although only 2%–3% meet full diagnostic criteria for the disorder. These figures are comparable to those of some epidemiological studies in adult
(8) and adolescent
(22) samples. Confirming anecdotal reports and a handful of clinical studies
(1,
2), more than one-third of people with anxiety disorders other than OCD or with depression (without comorbid OCD) endorsed obsessions and/or compulsions. Obsessions and compulsions were also relatively frequent (13%–17%) among individuals without mental disorders.
Second, the results suggest that obsessions and compulsions may cause interference even in people without OCD. The degree of distress/interference was highest for people with OCD, followed by people with other psychiatric disorders, and was lowest for people with no psychiatric diagnosis. But even in the latter group, about a quarter said they experienced and were bothered by the obsessions for more than 1 hour a day and periods of over 2 weeks, and 15% reported being emotionally upset by them. Obsessions were associated with higher distress/interference than compulsions, mirroring previous findings in OCD samples
(9) .
Third, it appears that only a minority of individuals who experience obsessions and/or compulsions seek help for these symptoms. Remarkably, most study members who sought help did not have OCD but other diagnoses such as depression, an anxiety disorder, or both. Some people (10%) who sought help for obsessive-compulsive symptoms in the past year did not even meet criteria for any psychiatric disorder in the past year. Replicating previous epidemiological data on OCD, people endorsing obsessions were more likely to seek help than people endorsing compulsions
(23,
24) regardless of whether they had a psychiatric disorder. However, only fears of harming others and shameful obsessions were predictive of help-seeking behavior. To our knowledge, this has not been reported previously. These types of intrusive thoughts may be perceived by people as pathological or “morally wrong,” and this may be a strong drive for seeking help. This would be consistent with the cognitive theories of OCD, which postulate that a central feature of the disorder is an exaggerated sense of personal responsibility for the prevention of harm to oneself or others
(25) .
Fourth, the frequency of specific types of obsessions and compulsions endorsed by the community does not necessarily correspond with that reported in large clinical samples. Harm obsessions and checking to prevent harm were the most frequent symptoms in this cohort. Checking rituals have been consistently identified as the most common compulsion in both epidemiological
(8) and large clinical samples of OCD patients
(26,
27) . Aggressive (harm) obsessions are also among the most commonly reported obsessions in clinical samples, together with contamination obsessions. Surprisingly, in this study, the proportion of individuals with contamination fears and washing rituals was much lower than expected from clinical studies. The reasons for this are unclear, but it is possible that individuals with these symptoms may be more likely to fit a stereotype of OCD and, therefore, to receive a diagnosis, resulting in an overrepresentation in clinical samples. Alternatively, this might occur because excessive washing can result in severe skin conditions requiring medical intervention. Once in the health system, these individuals may then be more likely to be referred to mental health services.
Fifth, obsessive-compulsive symptom dimensions tend to be temporally stable. The temporal stability of symptom dimensions is consistent with previous studies in clinical samples
(10 –
32) . Of interest, in our study temporal stability was strongest for the contamination/cleaning and symmetry/ordering dimensions and slightly weaker for the harm/checking and shameful thoughts dimensions. Past research shows that the major symptom dimensions of OCD may have different genetic, neural and neuropsychological correlates
(4,
21), implying partially different etiologies. It is therefore possible that the harm/checking and shameful thoughts dimensions are more closely tied to situational stressors than the other two dimensions investigated.
Sixth, the four symptom dimensions were associated with an increased risk of most mental disorders, and this was particularly marked for the shameful thoughts dimension. The specificity of the relationship with particular psychiatric disorders was, however, less clear than in previous clinical studies
(13) .
Seventh, children reporting obsessions/compulsions at age 11 were significantly more likely to endorse obsessive-compulsive symptoms and meet diagnostic criteria for OCD in adulthood, 20 years later. To our knowledge, this longitudinal link has not been previously reported and has important implications for early detection and prevention strategies, discussed below.
Limitations
Several limitations need to be acknowledged. First, hoarding symptoms are not assessed by the DIS-IV. Hoarding symptoms are relatively prevalent in clinical
(33) and in community samples
(34) and are associated with substantial levels of disability. Second, we assumed that the shameful thoughts item of the DIS-IV includes obsessions that people perceive as unacceptable or embarrassing, such as sexual and religious obsessions, but we were not able to probe the exact content of these thoughts. Third, some participants may have been reluctant to report embarrassing symptoms, resulting in an undercount of such symptoms. However, longitudinal study members who have been interviewed many times are probably more forthcoming about socially undesirable psychiatric symptoms than are research-naïve participants interviewed for the first time, because they have had the opportunity to build trust in the study’s confidentiality guarantee. Fourth, we were not able to study the continuity of specific symptom dimensions from childhood to adulthood, as few different types of symptoms were ascertained at age 11. Fifth, the results of this study are limited to a single birth cohort of young adults in one part of the world, and future research will need to establish whether the findings generalize to other cultures and age groups.
Wider Implications
Our results have several implications for future research, clinical practice, and nosology. Since obsessions and compulsions are relatively frequent in the community and cause a substantial degree of distress and interference, it will be important to understand the factors that may predict the development of full-blown OCD in some individuals but not others. From a clinical perspective, our results suggest that early recognition and treatment of obsessions and compulsions in the community may potentially reduce distress and interference from these symptoms and perhaps reduce risk for developing full-blown OCD and other mental health problems. The use of existing quick screening tools
(35) is feasible and would greatly increase the detection of potentially distressing obsessions and compulsions in the community. A recent study
(36) suggests that brief cognitive-behavioral work with individuals with subclinical OCD symptoms may reduce such symptoms in the long run, but this area of research is still in its infancy. Cost-effectiveness analyses will be required to decide whether these cases should be treated, but such calculations should take into account that treatment of mild cases might prevent a substantial proportion of future serious cases
(37) . Clinicians also need to be aware that many people who suffer from obsessions and compulsions may seek help for other reasons, such anxiety and depression.
Finally, the results support current dimensional views of psychopathology in general
(28 –
30) and OCD in particular
(4,
21) and have implications for DSM-V. First, the diagnostic boundaries of OCD could be broadened to include subsyndromal cases, which as we have shown are associated with substantial disability and increased risk of developing OCD and other mental disorders. Second, the specification of the major symptom dimensions of OCD in DSM-V would better capture the heterogeneity of the disorder and encourage further research in the field
(38) .