The physical and social environment in which individuals with both mental health and substance use disorders live has often been overlooked as an area of study. Dually diagnosed patients pose a particular challenge to psychiatric treatment, since they tend to have a more chronic course of illness, higher rates of relapse and rehospitalization, lower rates of treatment completion, and more complicated service needs than those with substance use problems only
(1 –
7) . The environmental context in which dually diagnosed individuals live may be particularly important, since substance abuse in this population is especially influenced by socioenvironmental factors
(8) . When these patients relapse, it is often environmental triggers that precipitate an episode
(9,
10) .
Recently, there has been increased interest in the environmental factors affecting mental health and substance use
(11 –
16), but relatively little research relates environmental context to treatment engagement, compliance, or outcomes
(17 –
19) . The neighborhood context has been discussed and examined in relation to its effect on crime, delinquency, violence, stress, depression, and physical health
(1,
11 –
12,
20 –
28) . Although most practitioners implicitly recognize the importance of a patient’s neighborhood environment, only limited research has been devoted to examining empirically the importance of environment in psychiatric and substance abuse treatment outcomes
(17,
18) . Drake et al.
(29) concluded that the most important future direction for intervention research in this area “needs to emphasize the environmental context…and not just new medications.”
The present study was designed to investigate the role of neighborhood influences in treatment compliance and continuity of care as well as rehospitalization among dually diagnosed patients (with at least one mental disorder and a substance use disorder) following discharge from an acute intensive care hospital unit. An innovative feature of this investigation was the use of geographic information systems software
(30) and geographic variables that capture spatial relationships to investigate neighborhood effects on individual behavior. Specifically, we examined which individual patient characteristics and neighborhood environmental factors predicted 1) initial outpatient treatment attendance within 30 days of hospital discharge and 2) rehospitalization within 1 year of discharge. Identifying the key elements of a patient’s neighborhood environment that might influence relapse and recidivism may help clinicians provide better long-term treatment planning and reduce the likelihood of relapse and recidivism, particularly in dually diagnosed patients.
Method
The present study is a retrospective analysis that utilized data extracted from the medical records of 380 patients who were diagnosed with comorbid mental health and substance use disorders and treated in an acute inpatient unit at Temple University Hospital—Episcopal Campus. The sampled records were from patients admitted between September 30, 2002, and December 31, 2003. The admission length of patients ranged from 3 to 13 days (mean=11.4 days). Diagnosis was established after a comprehensive intake interview was conducted by a psychiatrist using DSM-IV-TR criteria. Since medical chart data were used, we relied on normal hospital procedure for generating psychiatric diagnoses, and therefore the reliability and validity of the diagnoses are unknown. All patients 1) were seen by an attending psychiatrist and psychiatric resident upon admission as well as daily, 2) received daily individual and group psychotherapy, and 3) participated in 12-step groups. Upon discharge, patients were referred for ongoing outpatient mental health and drug treatment as clinically indicated. All patients were given a referral for outpatient 12-step programs in the community, in addition to individual psychotherapy. The network of possible outpatient placements in Philadelphia consisted of more than 100 facilities located throughout the city.
Inclusion criteria were a diagnosis of co-occurring disorders (at least one mental disorder and a substance use disorder) and a positive urine drug screen for prototypical illicit drugs upon admission. All patients were enrolled in Community Behavioral Health, which is the behavioral health management organization for all Medicaid recipients in Philadelphia County.
All procedures for gathering information from medical records during chart extraction were done in compliance with Health Insurance Portability and Accountability Act guidelines
(31), and information collected and entered into the sampled patient database did not include any identifying items, such as a patient’s name, actual address, Social Security number, or birth date. Since patients’ residential location was of primary interest for the research, exact address information (i.e., street address number) was de-identified by adding or subtracting a random odd number between one and 10, which preserved approximate block location while not breaching confidentiality. Data were collected by a research assistant, with authorization by Temple University Hospital after the study was classified as exempt by the Temple University Institutional Review Board.
Variables
Outcome variables
The two primary outcome variables were 1) treatment continuity, as measured by whether the patient attended his or her first outpatient appointment within 30 days of discharge, and 2) whether the patient was readmitted to the inpatient unit within 1 year of discharge.
Predictor variables
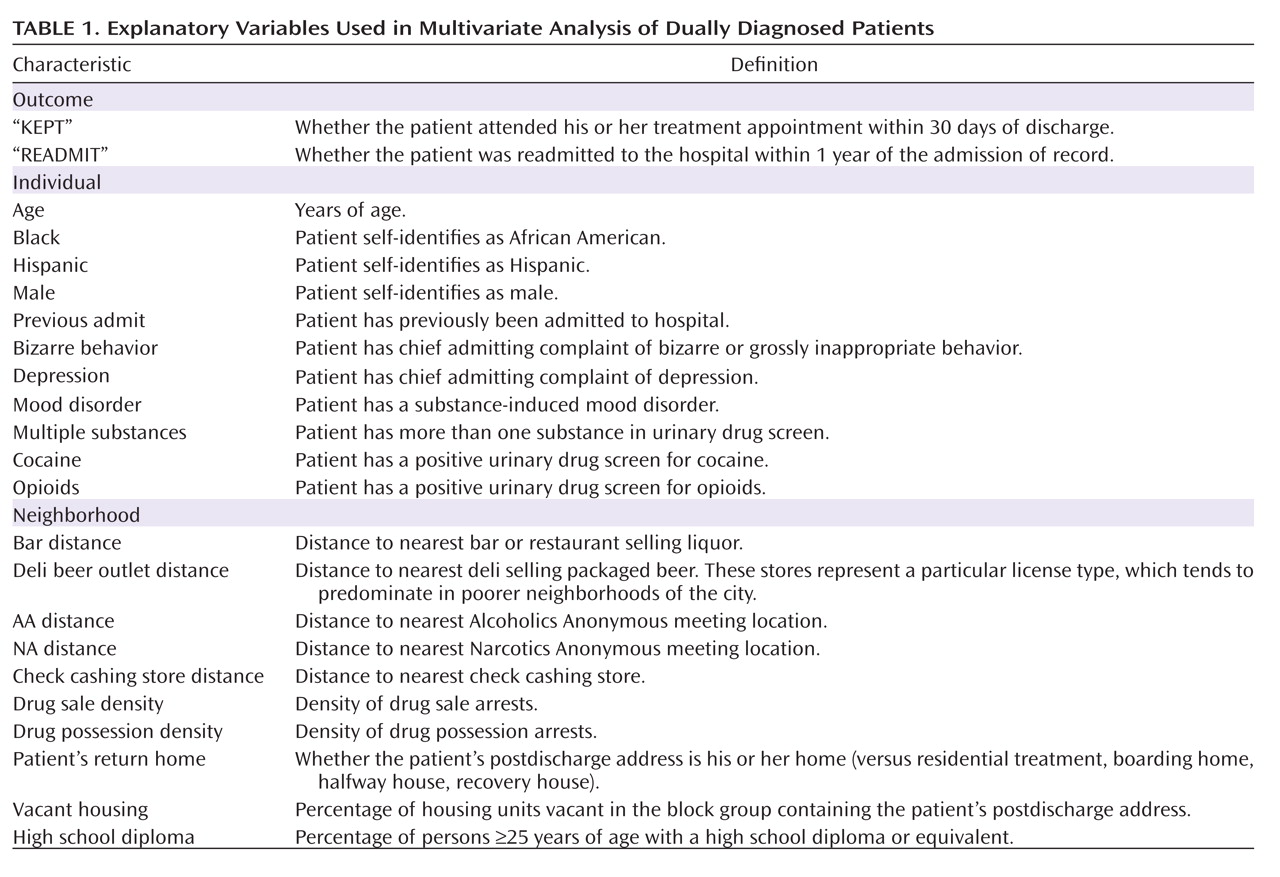
As seen in
Table 1, two categories of predictor variables were utilized in the analysis: 1) variables relating to individual patient characteristics and 2) variables associated with patients’ neighborhood environment. The individual-level patient variables were demographic characteristics, psychiatric assessment information, drug use data, housing status, criminal justice history, victimization data, and disability status. The selection of these variables was based on prior research relating to treatment outcomes for the study population
(3,
19) and information routinely available from medical records. Interrater reliability for data extraction was established in a previous study
(19) and found to have 95% agreement. Variables associated with neighborhood environment were collected from a variety of geographic characteristics in a patient’s home neighborhood. We expected these geographic characteristics to have some type of influence on patient outcomes. Our strategy for collecting geographic variables was derived from established theories of neighborhood social disorganization
(24,
28) and risky and protective factors relating to health and substance abuse
(32,
33) . Data on social disorganization, acquired from the 2000 U.S. Census at the block-group level, were 1) indicators of socioeconomic disadvantage (receiving public assistance, living below the poverty line, poor educational attainment, unemployment, female-headed households with children), 2) community isolation as a result of language barriers (Spanish speaking individuals, foreign-born population), and 3) social disorder as embodied by the presence of crime and dilapidation of housing infrastructure (vacant housing, drug sale offense arrests [data acquired from the 2000–2002 Philadelphia Police Department]). Geographic variables were appropriately normalized to condition on the underlying distribution from which they were drawn. For example, vacant housing refers to the total number of vacant houses normalized by the total number of houses.
Regarding risky and protective factors, it is pertinent to note that there has been very little empirical research on the influence of environmental factors in this specific context, particularly regarding the use of geographic characteristic-level data (as opposed to aggregated data, such as that from the U.S. Census). For this reason, rather than being restrictive, we investigated a variety of geographic characteristics that we theorized might influence treatment continuity and rehospitalization among the study population. Our strategy for data collection relied on our own previous research in this area
(19,
34) as well as other previous studies
(35,
36) that focused on geographic characteristic-level data in analyses of health and crime.
We collected data on indicators of alcohol and drug availability, since we presumed such features would have an obvious relationship with substance abuse. These indicators were 1) locations of drug possession arrests and 2) establishments licensed to sell beer and liquor under the Pennsylvania State Liquor Control Board (e.g., bars and restaurants, delis selling packaged beer, state-owned liquor stores). We also collected data on a variety of drug and alcohol treatment centers and programs, such as Narcotics Anonymous and Alcoholics Anonymous meeting locations. Additionally, we collected data on the locations of check cashing stores and pawn shops because these institutions often take the place of banks and other conventional financial institutions in many poorer neighborhoods and may serve as indicators of informal economies, including illegal activities such as gambling, drug selling, and prostitution.
Generating geographic variables
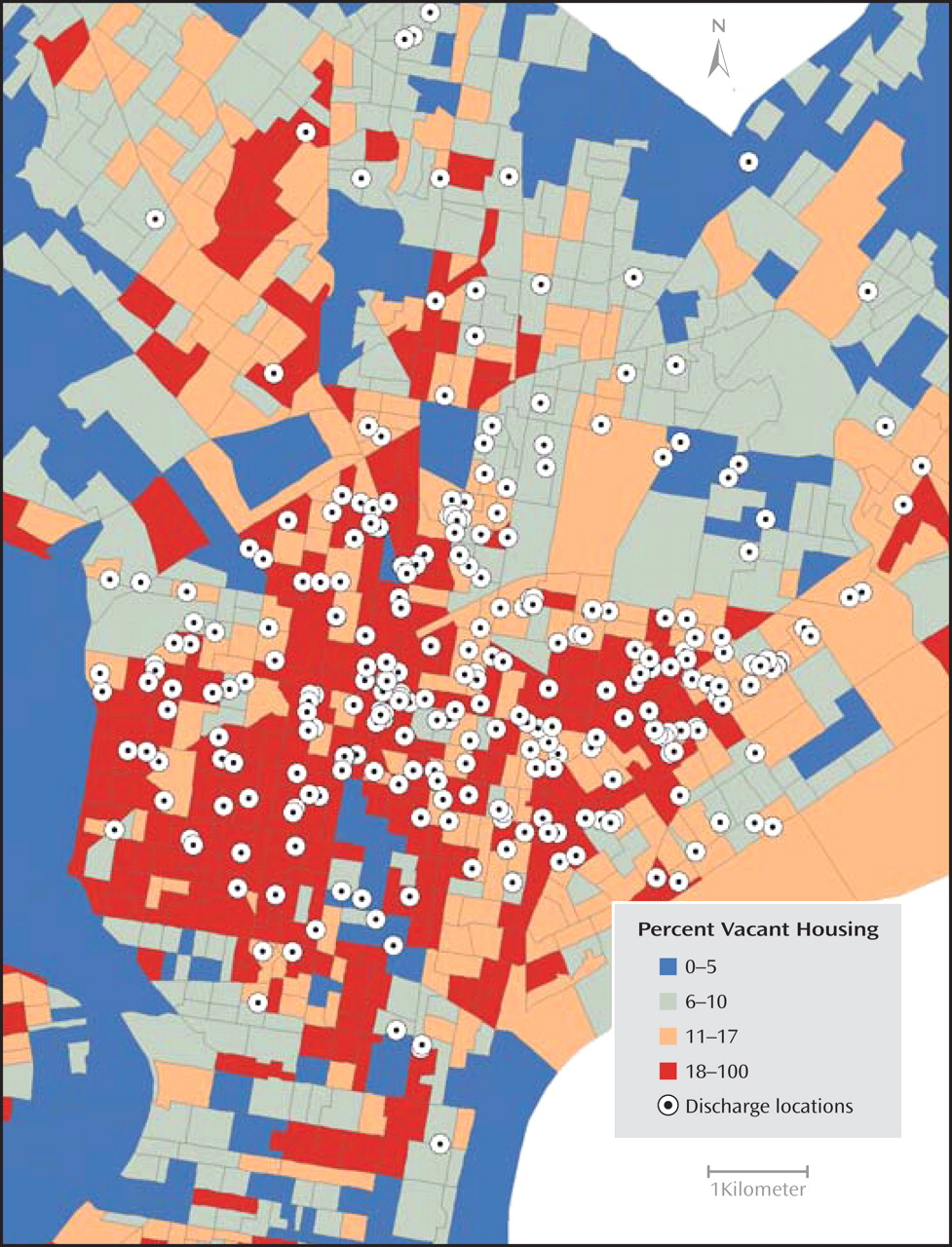
A geographic information system was utilized to convert the locations of subjects’ residence and neighborhood geographic features from text-based addresses to digital spatial data (
Figure 1 )
(37) . For certain types of geographic features, such as alcohol outlets, we theorized that access to the feature might influence the subject’s behavior. For each of these types of geographic features, we measured the distance between the location to which each subject was discharged after hospitalization and the nearest feature of interest. For other types of geographic features, we theorized that the influence of the feature on a subject’s behavior may not be a result of the subject’s direct access to the feature itself but rather of its influence on the overall character of the neighborhood. For these data, the density of geographic features near each subject’s postdischarge location was calculated based on the number of features (e.g., number of drug sale arrests) within a 500-meter radius circle of the postdischarge location. For U.S. Census data, which are available according to block-group spatial units, the value for each U.S. Census variable was joined with each subject according to the block group to which the subject was discharged after hospitalization.
Data Analysis Strategy
We were careful to develop parsimonious models of treatment compliance and hospital readmission and to mitigate issues of multicollinearity by conducting univariate statistical tests (Mann-Whitney U and chi-square tests) between each explanatory variable and either outcome variable (see the data supplement accompanying the online version of this article). We also identified pairs of explanatory variables that were highly correlated. This strategy allowed us to eliminate certain geographic explanatory variables (including several U.S. Census variables) that were 1) not related to either outcome (treatment continuity or hospital readmission) or 2) collinear with other geographic variables offering greater explanatory power.
Stepwise-forward logistic regression analysis was used to generate models for each outcome variable. Stepwise-forward regression is a common approach in selecting the most influential variables from a set of possible explanatory variables
(38) . It is an iterative approach that only adds predictor variables to the regression equation when predictor variables add explanatory power, after accounting for the influence of the other explanatory variables already present in the model. This method also assists in mitigating the presence of multicollinearity. For each outcome, stepwise-forward logistic regression was applied first only to individual explanatory variables (model 1), then only to geographic variables (model 2), and then to individual and geographic variables combined (model 3). We transformed the geographic variables by including the natural log of the raw value to better account for the nonlinear influence of geographic variables on the likelihood of treatment continuity or hospital readmission. The accuracy of each model was summarized according to 1) Nagelkerke’s R
2, 2) classification accurateness, 3) and area under the receiving operating characteristic curve. None of the geographic variables that appeared in the same regression equation had a Pearson correlation >0.20 or < –0.20. Our initial data set contained 504 patient records. Because 55 records did not geocode and an additional 69 records had incomplete data, our analyses were based on a total of 380 patient records with no missing data.
Results
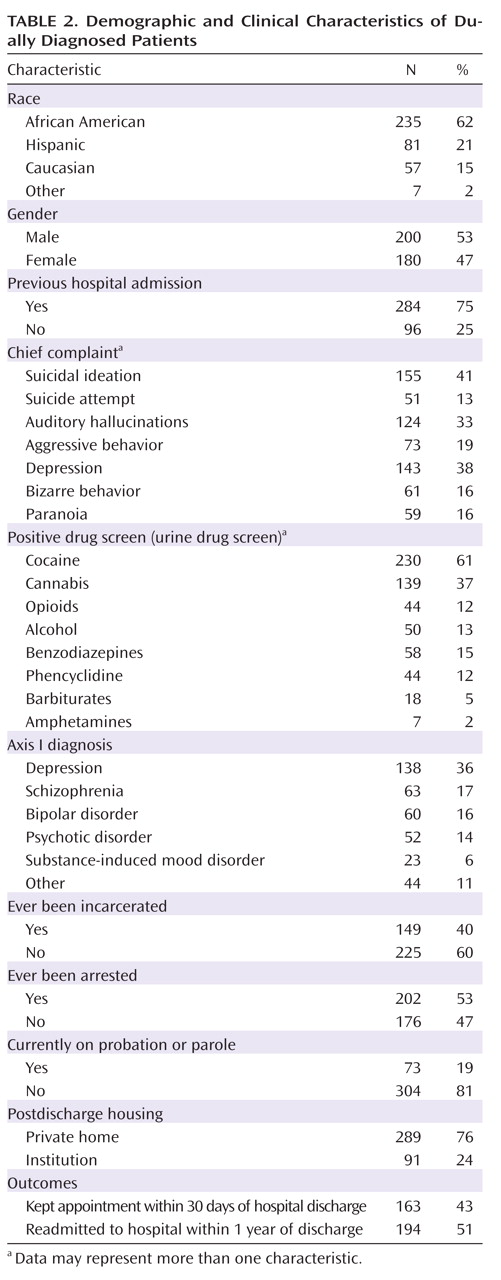
In general, the patients included in our sample represented a primarily poor, inner city, minority population, with the majority being active cocaine users (61%). Slightly less than one-half of the patients in the sample (43%) kept their initial outpatient appointment within 30 days of discharge from the acute inpatient unit, and approximately one-half (51%) were rehospitalized within 1 year.
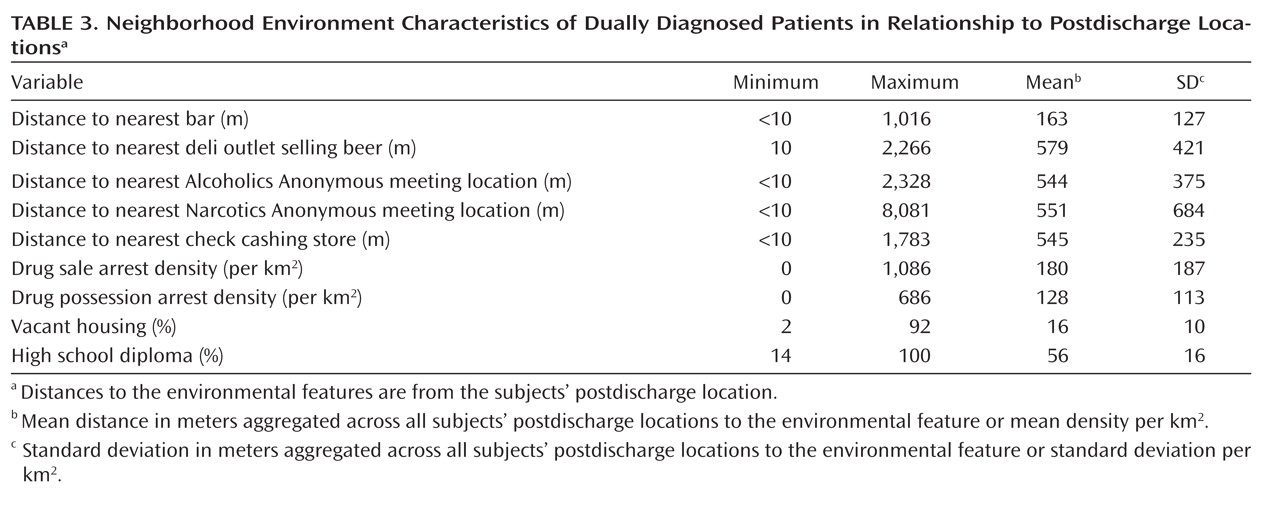
Table 2 details the demographic and clinical characteristics of the patients (mean age=38 years old; age range=18–67 years old), and descriptive data regarding neighborhood environment are reported in
Table 3 .
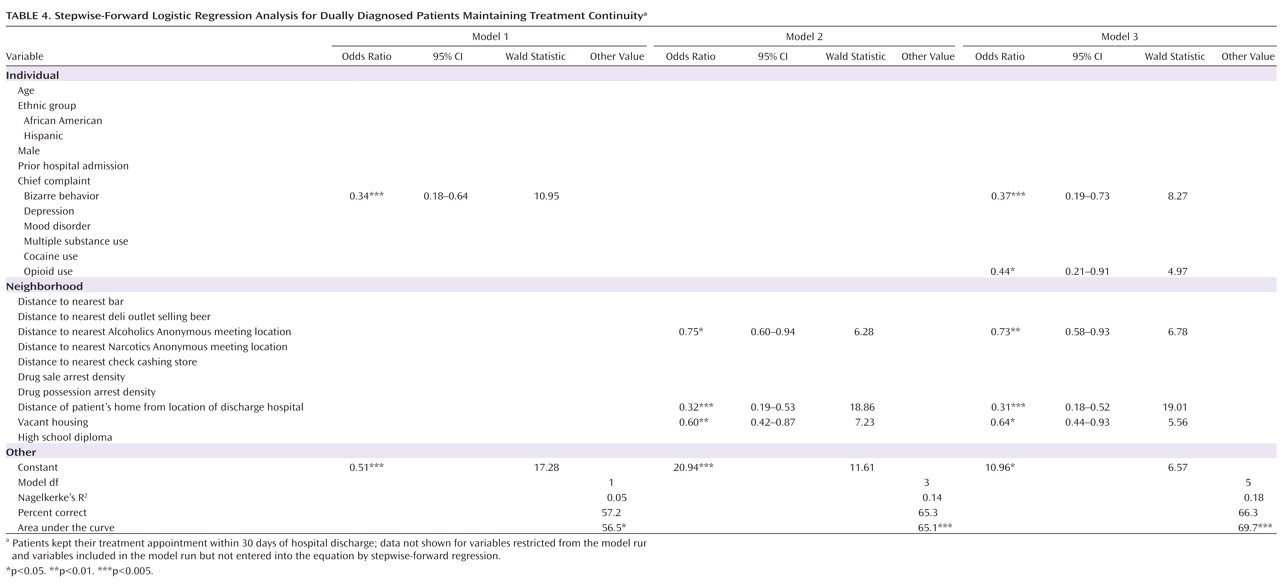
Results of the stepwise-forward regression analyses for outcome variables (whether a patient kept his or her appointment within 30 days of discharge [“KEPT”]; whether a patient was readmitted within 1 year following his or her index admission date [“READMIT”]) are reported in
Table 4 .
For the outcome variable pertaining to whether a patient kept his or her appointment within 1 year following his or her index admission date, model 1 contained the results of a stepwise-forward regression in which the geographic variables were excluded and only the individual-level variables were allowed to enter the regression equation. Results indicated that the chief complaint of “bizarre behavior” (i.e., grossly inappropriate behavior) was the only significant individual-level variable. None of the other individual-level variables explained a significant portion of the variance in the outcome to be included in the model once we accounted for the influence of bizarre behavior. Model 2 contained the results of a stepwise-forward regression in which the individual variables were excluded and only the geographic variables were allowed to enter the equation. Results revealed that patients were less likely to keep their appointments if they lived in areas with relatively high rates of vacant housing and areas relatively far from an Alcoholics Anonymous meeting location. Additionally, returning home following discharge (versus returning to residential treatment or a boarding home, halfway house, or recovery house) decreased the likelihood of treatment continuity. When both individual and geographic characteristics were allowed to enter the stepwise regression of the outcome variable pertaining to whether a patient kept his or her appointment within 1 year following his or her index admission date (model 3), all independent variables that were significant in models 1 and 2 remained significant, with approximately the same odds ratios and significance values. The following additional individual-level variable emerged as significant in this context: whether a patient had a positive urinary drug screen for opioids. Patients with this characteristic were less likely to attend their first treatment appointment within 30 days of discharge. It is pertinent to note that the classification accuracy of model 3 was higher than that for both models 1 and 2, although it exhibited only marginal improvement over model 2. The area under the curve was also higher for model 3 than for the other two models and was highly significant. The magnitude of the odds ratio for patients who kept their postdischarge treatment appointment is illustrated in
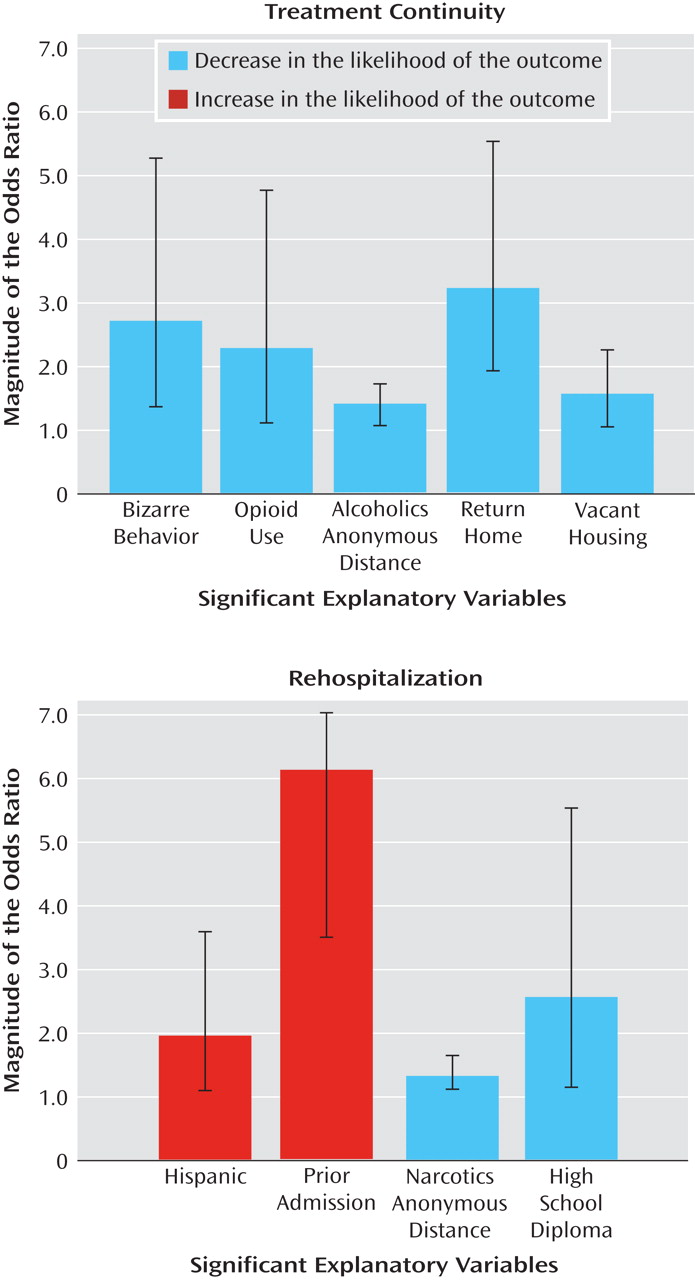
Figure 2 .
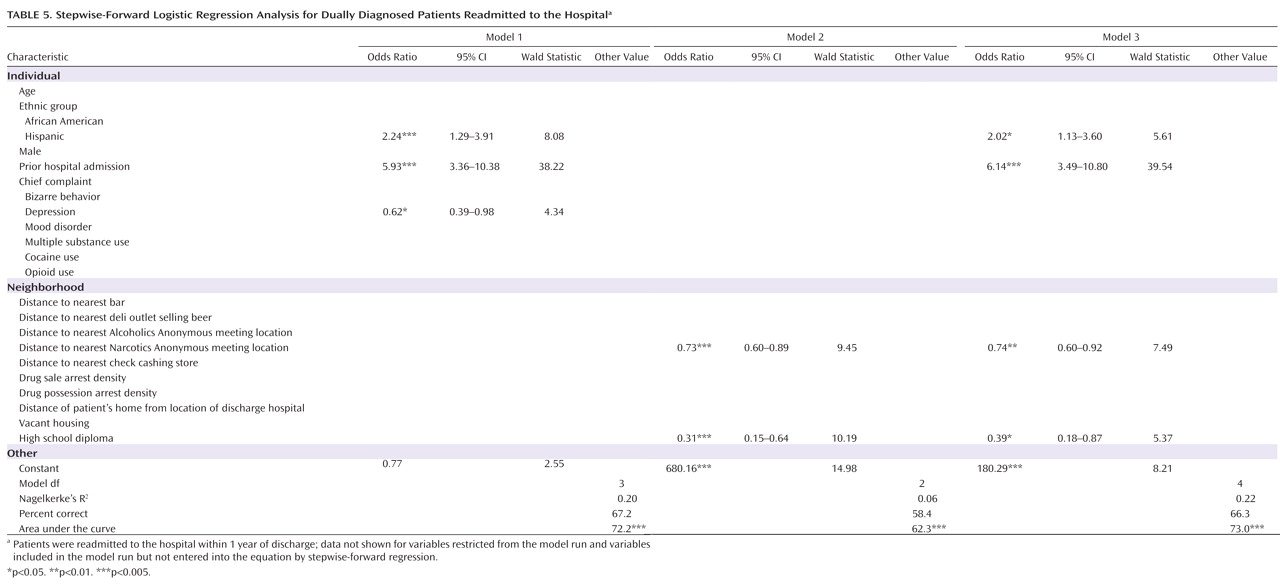
For the outcome variable pertaining to whether a patient was readmitted to the hospital within 1 year following his or her index admission date, models 1, 2, and 3 also show results for stepwise forward regression analyses of individual variables only, geographic variables only, and individual and geographic variables combined, respectively (
Table 5 ). Model 1 indicated that being Hispanic and having a previous admission to the psychiatric emergency room both increased the likelihood of being readmitted within 1 year, with the presence of a previous emergency room admission increasing the likelihood by nearly 600%. However, having a chief complaint of depression decreased the likelihood of being readmitted within 1 year (odds ratio=0.62, p<0.05). Two geographic variables emerged in model 2 as being significantly related to the outcome variable of being readmitted within 1 year: distance from a patient’s postdischarge location to the nearest Narcotics Anonymous meeting place and the percentage of people with a high school diploma residing in the block group of a patient’s postdischarge location. The likelihood of being readmitted within 1 year was increased if a patient was discharged after hospitalization to a location near a Narcotics Anonymous meeting place and in an area with low educational attainment. For model 3, in which all individual and geographic variables were combined, all independent variables present in models 1 and 2 remained in the model, with approximately the same odds ratios and significance values. The exception was the presence of the chief complaint of depression, which was present in model 1 but was not entered into the equation in model 3. Classification accuracy and the area under the curve showed that models 1 and 3 were largely equivalent in predictive power, being both highly significant and more accurate than model 2. Model 3 also included the outcome variable of treatment continuity and the geographic variable of the distance from a subject’s postdischarge location to the hospital in order to determine whether treatment continuity or proximity to the hospital influenced the likelihood of readmission within 1 year. However, neither variable contributed to the explanation of the variance in the outcome once we accounted for the influence of the other variables.
Discussion
The present study employed a geographic information system as a tool to determine the predictive value of various geographic factors in patients’ neighborhood environment, such as the proximity to bars, deli outlets selling beer, and Alcoholics Anonymous meeting places as well as crime, vacant housing, and various other features, that might influence an individual to adhere to their first outpatient psychiatric appointment within 30 days postdischarge or to experience rehospitalization within 1 year following discharge. The present research is consistent with that of Drake et al.
(29), who advocated for greater focus on environmental context in future intervention research to better address the long-term needs of dually diagnosed patients. Our results are also consistent with a small but newly emerging body of literature identifying various types of neighborhood factors associated with various negative mental health and substance abuse outcomes
(11,
15 –,
19,
22,
39) .
In the present study, the chief complaint of bizarre behavior (i.e., grossly inappropriate behavior) and a patient returning home following hospital discharge (versus returning to an institutional setting) were both found to reduce the likelihood of treatment continuity. As we suggested in previous research
(2), some individuals may seek initial hospitalization as a result of acute conflicts in their lives, for drug detoxification, or as a temporary respite from life on the streets. For these patients, continuing in outpatient treatment after discharge from the hospital may be of less importance than it is for those patients seeking relief from longer-term, chronic psychiatric illnesses. In the present study, patients who used heroin were less likely to attend outpatient treatment. This could be reflective of the nature of opioid addiction, in which outpatient treatment may be perceived as having less value than other types of modalities, such as residential and methadone maintenance therapy. Residing in an area with a high degree of vacant housing reduced the likelihood of a patient attending initial outpatient treatment. This variable most likely relates to the general quality of a neighborhood’s social disorganization. Indeed, a number of studies have identified neighborhood social disorganization as a factor associated with various negative mental health and substance abuse outcomes (e.g.,
15,
16,
22) . Patients who lived farther from an Alcoholics Anonymous meeting place were also less likely to attend their first postdischarge treatment appointment. This is, perhaps, because meeting locations appear to be predominantly located in nonminority, working or middle class neighborhoods or in center city/business districts, which are often not easily accessible for the patients assessed in our study.
In terms of rehospitalization, Hispanic patients had an increased likelihood of readmission within 1 year after discharge. Because our hospital is located in a Hispanic neighborhood, we theorized that proximity to the hospital would increase the likelihood of readmission. However, we examined whether the distance from a patient’s home to the hospital predicted rehospitalization and found that this variable was not significant. Close proximity to Narcotics Anonymous meeting places also increased the likelihood of readmission. An examination of the spatial distribution of Narcotics Anonymous meeting places in Philadelphia suggested that, in contrast to Alcoholics Anonymous meeting locations, Narcotics Anonymous meetings are located in areas where there are concentrations of drug users and are significantly correlated with drug sale density.
There are several limitations to the present study. The data were extracted from hospital charts and therefore may be less accurate than prospective, more highly controlled research studies. Additionally, the study was conducted in a single hospital in a limited geographic area. Further, it is possible for patients to have been readmitted to hospitals other than Temple University Hospital and therefore not be part of our data set. There are three other crisis response centers in Philadelphia, with Temple University Hospital receiving the greatest number of patients. The clinicians affiliated with the present study reported that most of their patients do tend to return to Temple University Hospital’s acute inpatient unit when rehospitalized, but this has not been verified empirically.
The present results, although preliminary, yield potentially important clinical implications for psychiatric populations. What is important is not so much the influence of the specific geographic variables that affected treatment continuity and rehospitalization, but rather that these findings should be viewed as evidence for the importance of further investigating the role of neighborhood context in psychiatric treatment and hospital aftercare planning. Currently, hospital discharge planning treatment staff rarely take into account the overall quality of a patient’s neighborhood or proximity to certain environmental features that might trigger relapse and rehospitalization. Patients are often influenced by the environment in which they live, and therefore we believe that the environmental contingencies, inherent in communities and neighborhoods, affecting individual behavior are robust concepts, which apply across the different geographic contexts of cities, nations, and cultures. A more explicit focus on an individual’s neighborhood and community context represents an important but understudied area in psychiatry, in terms of both research and clinical practice, which can potentially enhance long-term care and treatment planning for psychiatric patients. Additional collaborative work with experts in geographic information science is warranted to better understand the role of the neighborhood environment in predicting important clinical outcomes.