Residents in a psychiatric training program were unsure about whether and how they would like to interact with the pharmaceutical industry. They had been cautioned by some faculty members about the potential for industry influence to bias their thinking and behavior, while other faculty had suggested that associations with industry are inevitable and, frequently, desirable. The majority of residents in the program began to interact with the pharmaceutical industry via attendance at industry-funded activities, acceptance of industry-sponsored gifts, awards, and medication samples, and reading of industry-financed journals and research studies. A smaller group of residents, finding it difficult to disentangle the tendentious elements of industry influence from useful ones, eschewed contact with the pharmaceutical industry whenever possible.
Those residents who were considering research careers found themselves facing a particular challenge. They valued the intellectual independence of academia but, in an era of increasing competition for limited research funds, regarded collaboration with the pharmaceutical industry as an opportunity to gain access to valuable resources: therapeutic compounds, data, expertise, and funding. They wished to make informed and deliberate choices about how to engage responsibly with industry but were sometimes uncertain about how to proceed.
Over the past decade, it has become increasingly apparent that interactions among physicians, academic medical centers, and the pharmaceutical industry are fraught with conflicts of interest that threaten the reputations of industry and academia as well as the ability of doctors to interpret data and treat patients without undue bias (
1–
3). For example, a growing body of evidence shows that gifts from drug companies—ranging from food and pens to substantial stipends and honoraria—influence the choices that physicians make in treating their patients (
1,
4–
6).
In 2006, a joint task force of the American Board of Internal Medicine Foundation and the Institute on Medicine as a Profession published policy recommendations on conflicts of interest (
7), and the Association of American Medical Colleges followed suit in 2008 (
8). Both recommended strict guidelines, including a zero-dollar limit on all gifts (including food), restriction of interactions between industry representatives and physicians, centralized distribution of industry funds for continuing medical education, and discouragement of ghostwriting and speakers bureaus (
1). Although there are no clear mechanisms for enforcing these recommendations, the institutions that have implemented them have generally found the transition to be smooth and rapid, with "top-down" modeling of proper conduct particularly effective (
1). The current generation of residents and medical students may thus develop in a milieu where restraint and reflection in interactions with drug companies are the norm rather than the exception.
In the area of medical research, however, appropriate boundaries on interactions between academia and industry are less clear-cut, perhaps in part because this is a realm in which collaborations are more evidently mutually advantageous. Drug companies rely on medical centers to conduct trials and recruit patients, as well as for thought leaders to design studies and for academic scientists to identify new drug targets and test promising compounds. Complementarily, in an era of limited government funding, industry money is a much-needed boon to research activities in academic departments. In this context, industry-academia research collaborations have themselves become increasingly vulnerable to conflicts of interest. Whereas 20 years ago most academic investigators assumed complete responsibility for industry-sponsored studies, more recently the converse is true, with drug companies frequently exerting control over all aspects of the process, from designing experiments to analyzing data to writing papers to dictating final decisions on which data to publish and where (
2,
9). Studies are frequently designed and reported in ways that suit the interests of sponsoring companies, including over- or underdosing comparator compounds, choosing placebo-controlled trials over comparison with active competitor drugs, designating primary endpoints that are likely to favor the sponsor's product rather than the most clinically relevant outcomes, publishing partial data sets, and neglecting to publish negative results (
2). An illustrative example involves recent revelations about studies by Merck on the cyclo-oxygenase-2 inhibitor rofecoxib that were ghostwritten by company employees despite attribution to academic investigators (
10) or manipulated to underreport mortality caused by the drug (
11). Similarly, a review of 74 clinical trials of antidepressant medications found that all but one of 38 positive studies were published, but only three of 36 negative studies were accurately represented (
12).
It has been argued that major policy overhaul and increased oversight are needed in funding and publication processes for industry-sponsored research (
13). Equally important may be a culture and policy shift within academic departments to prioritize ethical and transparent interactions with industry, much as is currently happening with drug company contributions to individual clinicians and educational programs (
1,
3). A crucial point of intervention may be in the education of residents, who are in the process of learning to navigate relationships with industry.
Professor Jeffrey Lieberman, chair of the department in which the above-mentioned residents were training, informed the residents that he had been approached by representatives of a pharmaceutical company who wished to collaborate on a research project. The company was interested in conducting a post hoc analysis of two large prospective trials to determine how its medication (aripiprazole) compared with a reference compound (haloperidol) in a subpopulation of patients with early-stage schizophrenia (
14). Dr. Lieberman, with the company's agreement, invited residents to become involved and offered to mentor them through the collaboration process.
Several residents volunteered to attend meetings in which Dr. Lieberman modeled collegiality and professional independence in his dealings with the pharmaceutical representatives. There was limited interaction between the residents and the representatives when the chairman was not present (e.g., in the waiting room outside the conference room where the group met). After each meeting, Dr. Lieberman conferred with the residents and instructed them on responsible engagement with industry researchers. He emphasized the importance of careful review of the original trials (
14) and subsequent analyses of these trials (
15–
17) to determine what meaningful information might be obtained from a post hoc analysis; thoughtful selection of research hypotheses; and critical appraisal of results. Together, Dr. Lieberman and the residents framed several hypotheses of scientific and clinical interest and identified methods to test them using the company's data. They then submitted their hypotheses and proposed analysis plan to the industry representatives for statistical analysis.
The nature of interactions between psychiatric trainees and the pharmaceutical industry is complex. Residents experience significant exposure to industry in a variety of contexts (
18–
21), and many do not appreciate the potential consequences of resident-industry contacts (
18,
22). For example, in many, but not all (
23), studies, only a minority of residents reported believing that interactions with industry influence their prescribing practices (
18,
21,
24–
26), despite substantial evidence that information provided by drug companies to caregivers affects prescribing patterns (
18). In fact, psychiatric residents may feel more immune to industry influence than do residents in other medical specialties (
25).
Curiously, psychiatric training programs have placed little emphasis on educating residents about their contacts with industry. Until recently, most programs allowed unsupervised interactions between residents and industry representatives, and few had formal policies regulating these interactions (
20,
21,
27,
28). While the majority of programs provide some instruction on resident-industry relationships, teaching in this area is generally informal (
28) and tends to focus on the acceptance of gifts that may affect prescribing practices, to the neglect of other important relationships with industry (
18), such as research collaborations. The lack of guidance and training on research collaborations with industry is regrettable, given the importance of exposing residents to research early in their training (
29) and the considerable role that pharmaceutical companies play in research, particularly in the field of pharmacotherapy (
30).
One explanation for the dearth of policy and education on interactions between residents and industry may be the lack of clarity regarding the efficacy of such interventions. A variety of educational and policy strategies targeting residents have been investigated, including in a psychiatric training program (
25), with mixed results (
22,
31–
35). In one study, policies restricting contact between residents and drug companies were found to decrease the perceived benefit of these interactions (
34). Some educational interventions have been shown to improve residents' understanding of the complexity of relationships with the pharmaceutical industry (
22) or to lead residents to report greater caution when considering their future interactions with industry (
31). One intervention, in contrast, succeeded only in educating residents about the negative effects that interactions with industry may have on other physicians and did not persuade residents to reassess their own vulnerability to influence (
32). Another strategy showed little impact on residents' opinions of industry (
35). An educational intervention specifically targeting psychiatric residents resulted in decreased acceptance of gifts and supplies but did not appreciably alter attitudes about resident-industry interactions (
25). In light of these conflicting data, further development and assessment of strategies for teaching residents how to understand and negotiate interactions with the pharmaceutical industry are merited (
18,
20,
21,
24,
26,
27). Fortunately, there is substantial enthusiasm in the field of psychiatry, and among residents in particular, for more education in this area (
25,
28).
Dr. Lieberman and the residents met with the industry representatives to review the results of the statistical analyses. The representatives' report included some of the analyses proposed by the departmental group and an outline for a manuscript that concluded that aripiprazole outperformed haloperidol in patients with early-stage schizophrenia. After careful inspection of the report, Dr. Lieberman and the residents found that the results did not, in fact, unequivocally support the conclusions of the draft manuscript. They noted that the mean dose of haloperidol used in the study was 8.6 mg/day, higher than that used in the most recent first-episode schizophrenia trials (
36–
38). Aware that early-stage schizophrenia patients are more sensitive to drug side effects and require lower doses of medications for therapeutic response (by 50% or more) than chronic patients (
39–
41) and that haloperidol in first-episode psychosis causes more extrapyramidal symptoms than do second-generation antipsychotics (
36–
38,
40,
1–
44), the departmental group was prompted to consider whether the apparent superiority of aripiprazole may have been due predominantly to excessive dosing, and hence intolerable side effects, of haloperidol.
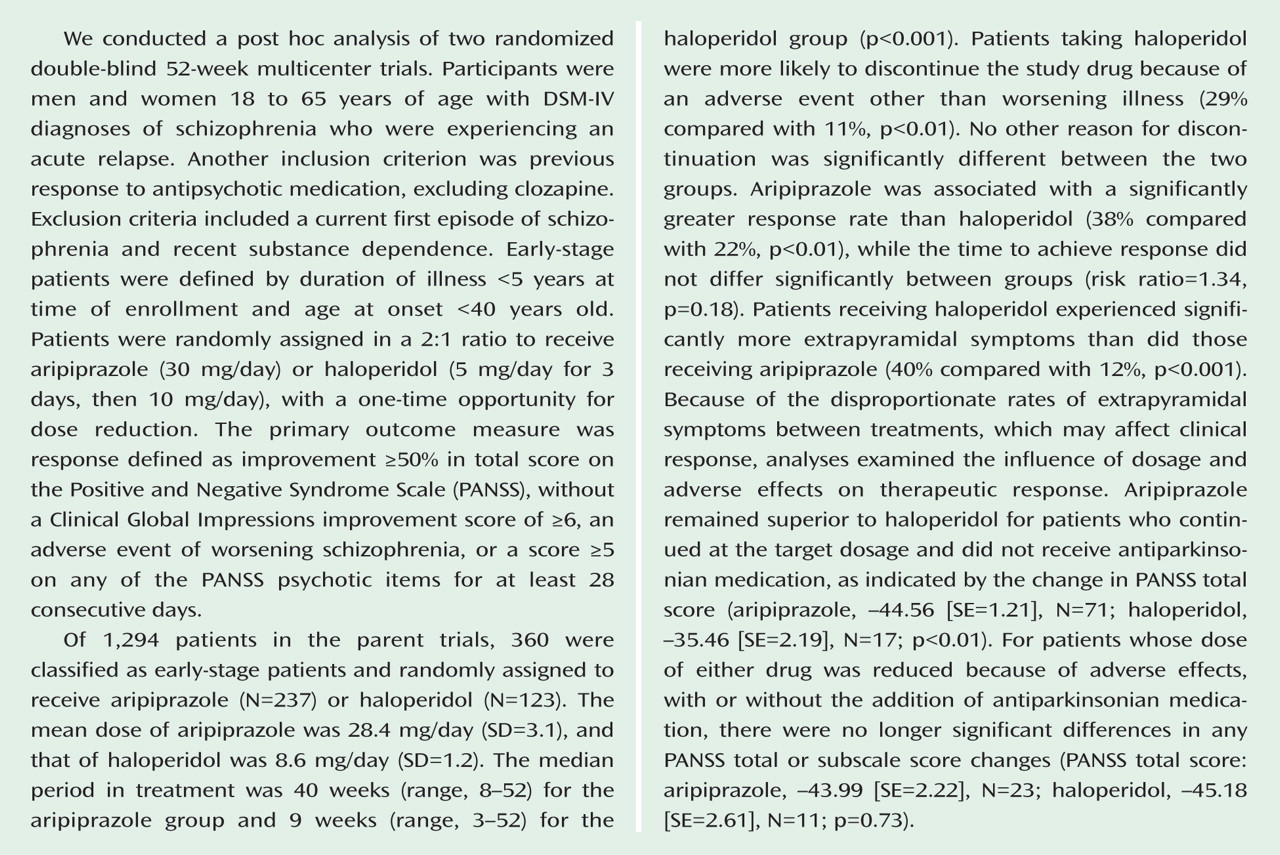
Dr. Lieberman and the residents worked with the industry representatives to obtain the complete results of the statistical analyses previously designated by the group (see
Figure 1). These analyses revealed high rates of extrapyramidal symptoms and increased and more rapid dropout from the study among patients treated with haloperidol. Discontinuation due to an adverse event other than worsening illness was the only significant difference in reason for treatment discontinuation between treatments. In addition, the efficacy differences on the Positive and Negative Syndrome Scale (PANSS) favoring aripiprazole were seen in measures that could be confounded with extrapyramidal symptoms (
45). Finally, when patients whose extrapyramidal symptoms were managed by dose reduction or the addition of antiparkinsonian medication were examined separately, all PANSS efficacy differences disappeared.
Under the supervision of Dr. Lieberman, the trainees drafted a manuscript that reflected their interpretation of these results, including their impression that the difference in drug efficacy may have been due to the differential dropout rate and greater side effects caused by the high dosage of haloperidol used in the study. These conclusions differed from publications of previous analyses of the parent trials, which found aripiprazole to be superior to haloperidol in durability of symptom response (
14), adverse effects (
14), remission rate (
15), new-onset tardive dyskinesia rate (
16), and utility (a function of PANSS scores and adverse effects) (
14–
17).
While developing the manuscript, the residents continued to meet, with Dr. Lieberman and separately, to discuss the challenges of the project. These challenges included the selection of appropriate statistical methods for a post hoc analysis with multiple hypotheses; the difficulty and importance of prioritizing the group's interpretations, even when they differed from those of the pharmaceutical company; and the lack of transparency regarding the original data, to which the company retained exclusive access.
By the end of the project, the departmental group believed that they had identified findings of interest to clinical and research communities and that their presentation of these findings was objective and accurate. They had also learned about post hoc hypothesis formation, several statistical techniques, and the importance of access to original study data.
Academic psychiatrists may benefit from research collaborations with industry (
46), and the enterprise of industry-sponsored research may itself be improved by the involvement of experienced academic investigators, as compared to exclusive reliance on researchers employed by the pharmaceutical industry. Few psychiatric training programs, however, provide instruction on how to negotiate these collaborations responsibly. We propose that the mentoring of trainees by a senior academic psychiatrist through a research project with industry representatives may be a useful means of teaching appropriate modes of working cooperatively with the pharmaceutical industry. Role modeling by senior psychiatrists has been reported to have a significant effect on the shaping of resident perceptions about industry in general (
21,
35), and our experience suggests that the same may be true of research collaborations in particular.
In the proposed arrangement, the academician-trainee-industry relationship is analogous to the supervisor-resident-patient triad that forms the backbone of psychiatric education in many training programs. Such an approach benefits from the reciprocal advantages of allowing trainees to learn fruitful and principled modes of engaging industry researchers and motivating senior psychiatrists to model critical thinking, independence, and integrity in their dealings with the pharmaceutical industry. Notably, this approach also suffers from the same limitations as other supervisory relationships, especially those imposed by the mentor's own biases.
Despite recent consternation over academia-industry research collaborations, we believe that these cooperative efforts will remain appropriate and valuable opportunities for academic psychiatrists, if conducted responsibly. Given the limited government resources currently available for research and teaching and the increasing costs of large long-term clinical trials, psychiatric training programs may wish to embrace the expanding role of research collaborations with pharmaceutical companies and teach ethical and productive engagement with industry investigators. We suggest that the mentoring of trainees by a senior academic psychiatrist may be one effective way of doing this.
Acknowledgments
The authors thank Dr. Itai Danovitch, whose thoughtful comments about industry-academia interactions informed this paper.