Completed suicide is almost always associated with psychiatric disorder, but the vast majority of those with psychiatric disorder neither attempt nor commit suicide. What is it that differentiates those depressed individuals who kill themselves from the rest of depressed patients? The answer to that question could improve our assessment and treatment of patients at risk for suicide.
Convergent work from postmortem studies, in vivo biological studies of suicide attempters, and family genetic studies has shown that among depressed individuals, those who have engaged in suicidal behavior show a distinct biological and clinical profile of interrelated characteristics, i.e., decreased central serotonin activity in the ventromedial prefrontal cortex, higher levels of impulsive aggression, and familial aggregation of suicidal behavior that is not explained by the transmission of psychiatric disorders like depression
(1) . Moreover, both changes in serotonin function and greater familial loading for suicidal behavior are related to high levels of impulsive aggression. However, it has not been clear which intermediate phenotypes of suicidal behavior best explain its distinct pattern of familial transmission. In this issue of the
Journal, the elegant family study conducted by McGirr and colleagues
(2), from the McGill Group for Suicide Studies, was designed to address this question.
Gottesman and Gould
(3) reintroduced the concept of an “endophenotype” to psychiatric genetics. Psychiatric conditions are complex, heterogeneous, and multigenetic. Complex disorders can be deconstructed into sets of simpler traits that are intermediate along the genetic pathway that links gene and disease. In order for a trait to be considered an endophenotype, it must be 1) associated with the condition, 2) heritable, 3) state independent, 4) a tract that cosegregates with the condition, and 5) found in the unaffected relatives of those with the condition at a higher than expected rate. The identification of a simpler trait that bridges the gap between genes and a more complex condition should, in theory, improve the chances of finding a relationship between disease and genotype.
One candidate endophenotype for suicidal behavior is the trait of “impulsive aggression,” which may be defined as the tendency to respond to provocation or frustration with hostility or aggression. Most often, this construct is assessed using measures of impulsivity, aggression, hostility, or fulfillment of criteria for one of the cluster B personality disorders. The McGirr and colleagues study is the most explicit and comprehensive examination of impulsive aggression as a putative endophenotype for suicidal behavior yet reported.
In this family study, depressed probands who committed suicide, nonsuicidal depressed probands, healthy comparison probands, and relatives of each proband group were compared with respect to frequency of suicidal behavior, cluster B personality disorders, impulsivity, lifetime aggression, and impulsive aggression. A single factor that correlated with all of these measures was constructed. Cluster B traits were more pronounced in depressed probands who committed suicide relative to healthy comparison probands, but were only higher at a “trend level” when compared with nonsuicidal depressed probands. Cluster B traits were familial and related to family history of suicidal behavior, and these two conditions appeared to cosegregate together. A similar pattern was found in the relatives of the three groups.
State independence and the level of cluster B traits in unaffected relatives were not specifically reported.
These results are consistent with other findings in the literature that show an association with cluster B traits and suicidal behavior, a higher rate or level of cluster B traits as a function of family loading for suicidal behavior, heritability of cluster B traits, and mediation of familial transmission of suicidal behavior via the transmission of the trait of impulsive aggression
(1,
4,
5) . Nevertheless, there are at least three questions that can be raised about impulsive aggression as an endophenotype for suicidal behavior.
First, cluster B traits are themselves complex and can likely be deconstructed into simpler and more homogeneous traits that can be more directly assessed through performance-based tests. Symptom-based assessments may not capture deficits in information processing and emotion regulation that are likely to contribute to cluster B traits. Laboratory measures of decision making, risk assessment, and emotion regulation that have been shown to have distinct neurobiological and genetic correlates may help to refine the impulsive-aggressive endophenotype
(6) .
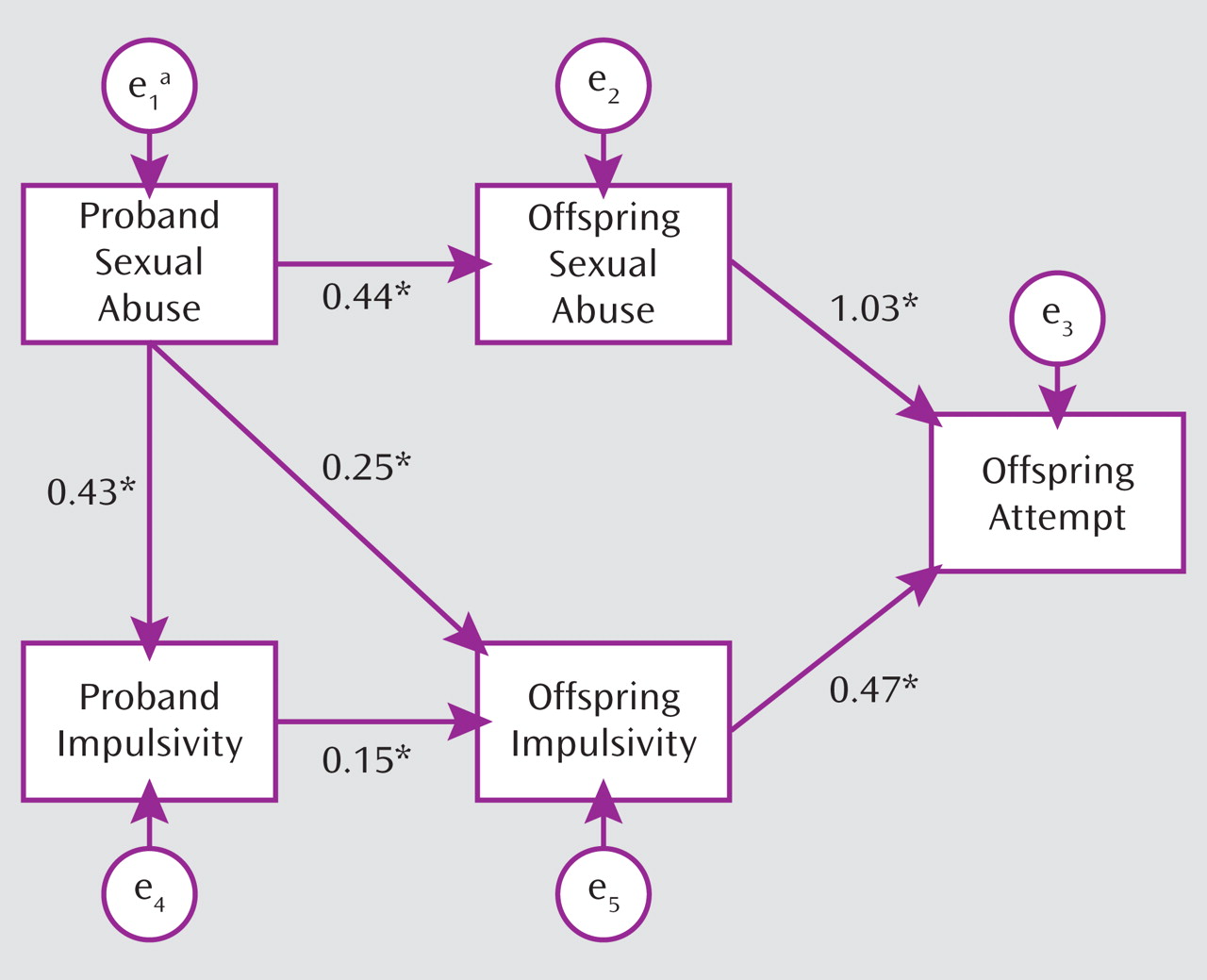
Second, while cluster B traits are heritable, the majority of the variance in familial concordance (60%–70%) seems to be explained by environment or measurement error
(5) . Moreover, the familial transmission of impulsive aggression may be cotransmitted with that of child maltreatment, which in part explains the familial transmission of suicidal behavior
(7) (
Figure 1 ). Thus, while impulsive aggression does appear to explain the familial transmission of early-onset suicidal behavior, it may do so through mechanisms that are both environmental and genetic, which may undercut its utility as a purely genetic endophenotype.
Third, the tacit assumption in this article and in the field is that impulsive aggression is a trait that is orthogonal to depression, when, in fact, the two are interrelated. The levels of both suicidal behavior and cluster B traits among the nonsuicidal depressed probands and their relatives are intermediate between those of depressed probands who committed suicide and healthy comparison probands. If these two sets of traits are really independent, one would not expect to find any difference between the nonsuicidal depressed and healthy comparison proband groups, and both would be equally distinguished from the depressed probands who committed suicide. Retrospective studies show that an earlier age of onset of mood disorder is associated with a higher rate of cluster B disorders
(8), and prospective studies indicate that higher levels of impulsive aggression predict earlier age of onset of mood disorder and suicidal behavior
(4,
9) . Impulsive aggression may be a precursor of depression, a
forme fruste, or may predispose to life events that are likely to bring on depression. Conversely, early onset of mood disorder may impair the development of adequate affective regulation strategies needed to constrain impulsive aggressive tendencies. Furthermore, studies have shown relationships among high family loading for mood disorder and suicidal behavior, abuse in the parent and in the child, and earlier onset of mood disorder
(10), which further supports the need to characterize age of onset of depression, early childhood adversity, and impulsive aggression in future genetic studies.
In summary, McGirr and colleagues have made an elegant and important contribution to our understanding of the role of impulsive aggression as an endophenotype for early-onset suicidal behavior. Future studies should use performance-based measures to further deconstruct impulsive aggression, carefully assess the relationship of impulsive aggression to the intergenerational transmission of trauma, and characterize the temporal and causal relationship between impulsive aggression and age of onset of mood disorder. These strategies should improve our chances of finding genes associated with suicidal behavior, help identify individuals at highest risk for suicide, and frame targets for the prevention and treatment of suicidal behavior.