Suicide is a rare event, with an incidence of 12.0 deaths per 100,000 population (
www.cdc.gov/nchs/fastats/suicide.htm). The rarity of suicide makes it impossible to predict on the basis of known risk factors if or when a given patient will die by suicide (
1). While it is impossible to predict individual suicides, suicide rates in the general population may be reduced by systematic physician education on the identification and treatment of modifiable risk factors (
2). Identifying clinically relevant risk and protective factors requires prospective studies of patients at high risk for suicide that use multidimensional assessments and systematic follow-up. The results of such studies are immediately applicable to clinical assessments and treatment interventions.
Borderline personality disorder is the only DSM-IV diagnosis defined in part by recurrent suicidal and self-injurious behaviors (called the “behavioral specialty of the borderline patient” by Gunderson and Ridolfi [
3]). In one study, history of suicide attempt was noted in over 70% of consecutively studied borderline inpatients, with an average of three or more attempts at the time of initial assessment (
4). Comorbidity with borderline personality disorder increases the likelihood of suicidal behavior in other high-risk disorders (
5). Some population studies found a comorbid diagnosis of borderline personality disorder in one-quarter to one-third of completed suicides (
6,
7), and in half of parasuicidal patients admitted to hospital (
8), although prevalence varied greatly with sample characteristics and study methods. With a suicide completion rate up to 10% and a community prevalence estimated at 2% in the Epidemiologic Catchment Area Study (
9), borderline personality disorder is a high-risk, clinically relevant model for the study of suicidal behavior.
A history of prior attempts is among the most powerful predictors of completed suicide. While only 10%–15% of suicide attempters become completers, 30%–40% of completers have a history of attempts (
10). Previous attempts increase the likelihood of subsequent attempts (
11). Attempters and completers are overlapping populations, with outcome determined in part by seriousness of intent and degree of medical lethality (
10). High-lethality attempters with borderline personality disorder share many characteristics with patients who complete suicide (
9); however, the literature is inconsistent on the degree of overlap and on which characteristics confer greatest risk. Different methods and sample characteristics have produced differing results across studies. In a psychological autopsy study using a case-control design, McGirr et al. (
12) found that suicide in borderline personality disorder was best predicted by cluster B comorbidity (especially antisocial personality disorder) and a risk-enhancing interaction between impulsivity and aggression. Suicides were more likely to have comorbidity with axis I disorders and substance dependence but less likely to have previous attempts and many hospitalizations. Retrospective studies using chart reviews of suicide completers and cross-diagnostic studies of high-lethality attempters have also reported the association of antisocial comorbidity and substance use with completion but found that previous attempts and serious attempts are more characteristic of borderline completers and high-lethality attempters (
9). Systematic prospective studies of high-risk patients using standardized multidimensional methods are needed to clarify which risk factors confer the greatest risk for completed suicide.
Following Mann et al. (
5), we studied a stress-diathesis model of suicidal behavior that predicts an increase in suicide risk when state stressors such as acute depression, drug abuse, or interpersonal crises interact with chronic personality traits such as impulsive aggression, pessimism, and hopelessness. In the first report from this longitudinal study (
13), we noted a very high rate of suicide attempts in the first 2 years of follow-up (24.8% of 133 subjects). An acute stressor, major depressive disorder, was predictive of attempts only in the short term (e.g., 12 months), while measures of psychosocial functioning and illness severity were predictive of attempt behavior through the first 2 years. A low baseline Global Assessment Scale (GAS) score, assessed independently of previous attempt experience, was associated with a higher risk of suicide attempt in a pooled interval 2–5 years after intake. A high baseline GAS score indicated a protective factor. Outpatient treatment was a protective factor that diminished the risk of attempt in both short-term (12-month) and long-term (2- to 5-year) intervals. In this report, we extend our analysis to an interval of 6 years and analyze predictors of suicide attempts at 1-, 2-, 4-, and 6-year intervals.
Method
This study was approved by the institutional review board of the University of Pittsburgh and funded by the National Institute of Mental Health. Participants were recruited both from the inpatient and outpatient services of the Western Psychiatric Institute and Clinic and from the surrounding community by advertisement. Written informed consent was obtained after participants were given a complete description of the study. Participants were assessed in multiple sessions by experienced master's-level clinical raters using semistructured interviews and standardized self-rated and interviewer-rated measures. Axis I diagnoses were made using the Structured Clinical Interview for DSM-III-R (SCID;
14). DSM-IV criteria were used after that version was introduced. Axis II disorders were diagnosed using the International Personality Disorders Examination, which has a lifetime time frame (
15), and borderline personality disorder was diagnosed using the Diagnostic Interview for Borderline Patients (DIB;
16), which has a 3-month to 2-year time frame for subsection scores. The Diagnostic Interview for Borderline Patients–Revised (DIB-R) was added when that version became available (
17), and it was scored concurrently to preserve continuity with the longitudinal study. The DIB-R has a 2-year time frame. For inclusion in the study, participants met criteria for “probable” or “definite” borderline personality disorder on the International Personality Disorders Examination and “definite” on both versions of the DIB. Exclusion criteria included presence of schizophrenia, delusional (paranoid) disorder, schizoaffective disorder, any bipolar disorder, psychotic depression, CNS pathology (e.g., organic mood disorders and seizure disorder), drug or alcohol dependence, physical disorders with known psychiatric consequences (e.g., hypothyroidism), and borderline intellectual functioning (IQ <70 as measured by the WAIS). Final diagnoses were determined by consensus of raters using all available data.
The variables assessed as risk factors included 1) demographic variables; 2) axis I and II diagnoses; 3) history of suicidal behavior (
18) and scores on the Suicide Intent Scale and the Scale for Suicidal Ideation (
19); 4) scores on the Beck Depression Inventory (
20), the 24-item Hamilton Depression Rating Scale (
21), the Beck Hopelessness Scale (
22), and the GAS (
23); 5) scores on the Barratt Impulsiveness Scale, version 11 (
24), and the Buss-Durkee Hostility Inventory (
25), the lifetime history of aggression (
26), score on the MMPI psychopathic deviate subscale (
27), the number of borderline and schizotypal diagnostic criteria, and dimensional scores on the International Personality Disorders Examination; 6) childhood history of abuse; 7) family history of psychiatric disorders and suicide; 8) score on the Social Adjustment Scale–Self-Report (
28); and 9) history of psychiatric treatment.
Suicidal behavior was defined as self-injurious behavior with intent to die. Suicidal behavior was rated for medical seriousness using the Lethality Rating Scale, which assesses medical consequences on a scale from 0 (no consequences) to 8 (death) for methods of suicide (
18). Subjects were assessed at baseline and at 3- and 12-month intervals in the first year and annually thereafter, supplemented by semiannual telephone assessments. At each assessment, all data were updated. Deaths were discovered through the Social Security Death Index and family contacts. Participants were paid for all their time and effort.
Statistical Analyses
Participants with a baseline assessment and at least one follow-up were screened for this study; however, only those with a minimum of 6 years in the study and a follow-up at 6 years or beyond were included in the analyses. Participants were included in the analysis only if their follow-up data on suicidality were complete. Cox proportional hazards regression models were constructed to examine the predictive association between risk factors and suicide attempts. The outcome of interest was defined as any medically significant suicide attempt within the 6-year interval that scored 2 or higher on the Lethality Rating Scale (i.e., some degree of medical attention). Time to event was computed as the difference between the baseline assessment date and the date of the first suicide attempt in the interval. To assess the effects of treatment on outcome, treatment variables were assessed within the 6-year interval, counting the most recent intervention before any suicide attempt in the interval. To use the entire interval for attempters would confound the role of treatment, as most medically significant suicide attempts at our medical center are followed by psychiatric treatment. For nonattempters, the entire interval was used.
Estimates of relative risk and associated 95% confidence intervals were obtained from these models. Missing data resulted in variable sample sizes for some analyses. Data that were missed at predefined assessment points (because of participant unavailability) but obtained later were counted retrospectively in the correct time frame for specific events, using only objective data (e.g., demographic changes, suicide attempts, hospitalizations, new onset of major axis I disorders, and treatment episodes). Analyses were performed using SPSS for Windows, version 17 (SPSS, Chicago).
Results
There were 121 participants with follow-up assessments, but only 90 (74.4%) with a follow-up at or beyond the sixth year of participation. Among the 90 participants, 44 completed the sixth year follow-up on time, and 46 completed a follow-up beyond the 6 years with objective data (e.g. suicide attempts) entered retrospectively for the sixth-year follow-up. The 6-year sample was 73.3% female, with a mean age of 29.1 years (SD=8.3). Participants were 79.8% Caucasian and had a mean socioeconomic status of 3.4 (SD=0.6) on the Hollingshead Index (class III). A majority of participants (62.5%) had never married, and 27.0% had children living with them. Inpatient recruitment yielded 48.9% of participants, while 21.6% were from outpatient clinics, and 29.5% were not patients at the time of intake. At the baseline assessment, 52.8% of participants had a current DSM-III-R diagnosis of major depressive disorder and 59.6% had substance use disorders. The most common axis II comorbidity was antisocial personality disorder, which was found in 20% of participants.
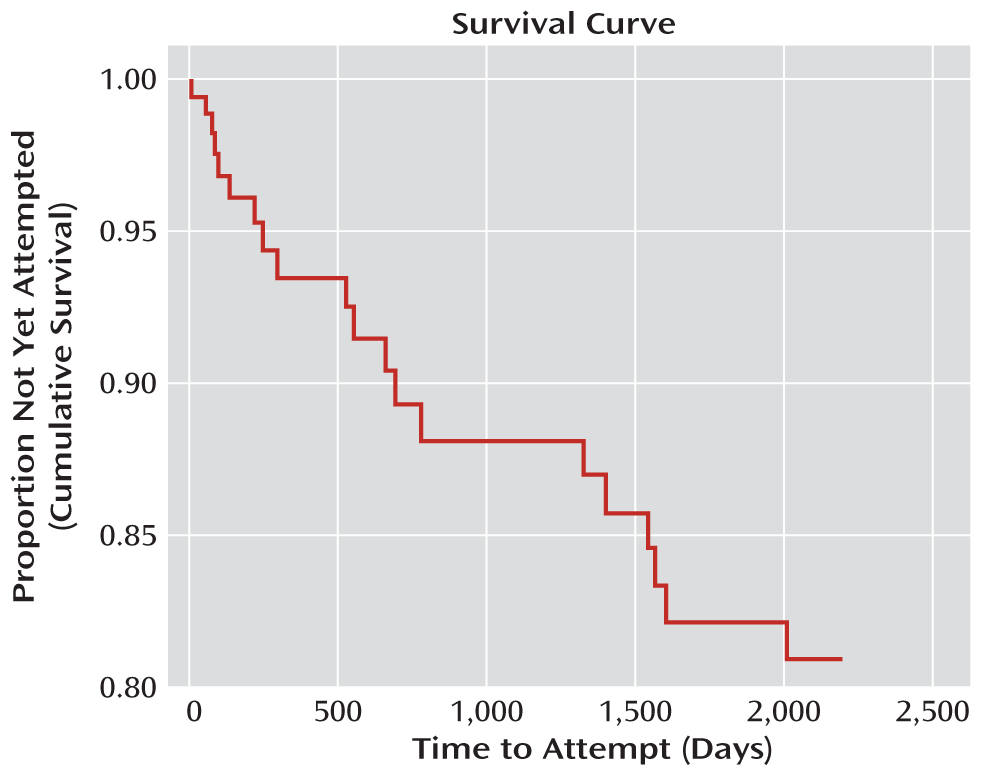
In the 6-year interval, 25 participants (27.8%) reported medically significant suicide attempts. The survival curve (
Figure 1) illustrates the fact that most suicidal behavior occurred in the first 2 years (24.8% of 133 participants at 2 years) (
13). Selected bivariate comparisons between groups are presented in
Table 1. (Bivariate comparisons for all variables in the study are presented in Tables S1–S6 in the data supplement that accompanies the online edition of this article.) Attempters differed from nonattempters in having significantly lower socioeconomic status, less education, and poorer social adjustment at baseline (p<0.05 in all cases); they also had a lower mean GAS score at baseline, although this difference fell short of statistical significance. Attempters were more likely to report a history of medication use and psychiatric hospitalization before the attempt and to report a family history of suicide, although these differences also fell short of significance (p<0.1 in all cases). There was no significant difference between groups in history of previous attempts at baseline. Ninety-two percent of those attempting suicide during the interval reported previous attempts at the baseline assessment compared with 81.3% of those who did not attempt suicide during the interval. There were no significant differences between groups in axis I or II comorbidities, depressive symptoms, measures of impulsivity or aggression, illness severity, childhood history of sexual abuse, age at first hospitalization, or total number of previous psychiatric admissions.
Results of Cox regression analyses are presented in
Table 2 for all intervals, including the 6-year model. At the 6-year follow-up, the variables that best predicted an elevated risk of suicide attempt during the interval were a family history of suicide, no outpatient treatment before the attempt, a low socioeconomic status at baseline, and poor baseline psychosocial functioning. A high GAS score at baseline was the only variable that was associated with lower risk.
There have been eight deaths since the inception of the study, occurring at a mean age of 41 years (range, 25–59). As stated on death certificates, causes for the eight deaths included one suicide (hanging), six accidental deaths, and one natural death. All accidental deaths were directly or indirectly related to acute or chronic effects of substance abuse: four were from acute drug toxicity, one from end-stage liver disease from alcoholism, and one from smoke inhalation (from a house fire) while comatose from alcohol. One death from pancreatitis was ruled “natural,” but it occurred in the context of chronic alcohol dependence.
Discussion
Suicide attempts occurred most frequently in the first 2 years of follow-up (19% of 137 participants in the first year and 24.8% of 133 participants by the second year) (
13). Thereafter, the number of new attempts decreased rapidly with time. Prospective predictors changed dramatically over time. In the shortest interval (12 months), attempts were predicted by major depressive disorder, an acute stressor. Thereafter, no acute clinical stressors predicted attempts. Both of these results may be attributable to illness severity and inpatient recruitment for nearly half of this sample. The frequency of repeat suicide attempts in the year after hospitalization for an index attempt has been reported at 17%, independent of diagnosis (
29). The Collaborative Longitudinal Personality Disorders Study, a prospective study including borderline personality disorder, found that 20.5% of treatment-seeking borderline patients attempted suicide during the first 2 years of the study (
30). Worsening of major depressive disorder predicted suicide attempt in the following month in that study's pooled personality disorders sample. Suicide attempt after hospitalization (and predicted by major depressive disorder) strongly suggests persisting depression. Similarly, illness severity, marked by psychiatric hospitalizations in the follow-up interval (but preceding any attempt), was predictive of subsequent attempt through the fourth year of follow-up. Notably, any outpatient treatment in the 12-month interval was associated with lower suicide risk, suggesting the successful treatment of major depressive disorder or decreased illness severity. The absence of outpatient treatment remained a predictor of suicide risk in the 6-year follow-up. The most consistent predictors of suicide attempt across all intervals were measures of psychosocial and global functioning. Poor psychosocial functioning predicted increased risk of suicidal behavior at 12 months, 2 years, and 6 years, while a high GAS score at baseline was protective at 4- and 6-year intervals. By the sixth year, low socioeconomic status was also a predictor of high risk. Poor psychosocial functioning at year 6 was most significant in the family, social, and vocational subscales of the Social Adjustment Scale. Good social support is a known protective factor against suicide, buffering the adverse effects of negative life events, which are prominent in the lives of patients with borderline personality disorder (
31). Negative life events among patients in the Collaborative Longitudinal Personality Disorders Study predicted suicidal behavior in the month during and preceding the adverse events (
32). Poor GAF scores at baseline and poor family relationships were significant predictors of poor psychosocial outcomes among borderline patients at the 2-year follow-up (
33). Functional impairment in social relationships changed little despite improvement in diagnostic criteria (
34). The McLean Study of Adult Development found that half of the subjects with borderline personality disorder failed to achieve social and vocational recovery at the 10-year follow-up despite symptomatic remission of diagnostic criteria in 93% (
35). Vocational failure contributed most to poor psychosocial functioning. Suicidal and self-injurious behaviors remitted early in the course of the McLean study (
35); however, symptomatic improvement did not prevent poor psychosocial outcome in the long term. If the majority of borderline patients can expect symptomatic remission in time, who dies by suicide?
The attempters in our study are characterized by low socioeconomic status, low educational achievement, and poor psychosocial adjustment. Across many studies, poor psychosocial functioning is a predictor of suicidal behavior independent of diagnoses (
5) and a predictor of high-lethality attempts and suicide completion in some, but not all, studies of borderline personality disorder (
9) as well as in nonclinical populations. Community members with personality disorders who complete suicide have more problems with relationships, jobs, unemployment, and family compared with community members with no personality disorders who complete suicide (
9). Community subjects with borderline personality disorder have lower educational and vocational achievement than subjects with other personality disorders, and they are more likely than other axis II patients to be receiving disability payments (
36).
Recurrent suicidal behavior early in the course of borderline personality disorder is often characterized by impulsive, angry acts in response to acute stressors, such as perceived rejection. These are “communicative gestures” (i.e., impulsive behaviors with little lethal intent, objective planning, or medical consequences). Impulsivity in borderline personality disorder is significantly associated with number of suicide attempts but not degree of medical lethality (
9). The McLean study found that “manipulative suicide efforts” diminished with time, from 56.4% of subjects at year 2 to 4.2% by year 10 (
35). Completed suicide in borderline personality disorder tends to occur after many years of illness, failure to benefit from treatment, loss of supportive relationships, and social isolation. In their 27-year naturalistic follow-up study, Paris and Zweig-Frank (
37) observed that borderline patients who completed suicide had “burned out” their social supports and were no longer involved in active treatment. The average age at death was 37 years. This suggests that there may be a high-lethality subgroup of borderline patients with poor prognosis who are at greater risk over time.
To identify subjects who had increasing degrees of medical lethality with recurrent attempts, we recently reported a trajectory analysis of Lethality Rating Scale scores in borderline patients who had three or more suicide attempts (
38). Two distinct patterns were identified: a low-lethality group of subjects who had recurrent but minimally lethal behaviors, and a high-lethality group who had increasing medical lethality scores with recurrent attempts. Those with the high-lethality trajectory were characterized by inpatient recruitment (a severity marker) and poor psychosocial functioning, while the low-lethality group had more negativism, substance use disorders, and histrionic or narcissistic comorbidity.
Our sample is still young (mean age=29 years) and early in the trajectory of their suicidal behaviors. However, after 6 years of follow-up, we have observed that low socioeconomic status, poor psychosocial adjustment, and absence of outpatient treatment are predictors of suicidal behavior. We suggest that these are characteristics of a poor prognosis subtype. By follow-up at 4 and 6 years, a family history of suicide is a prominent risk variable. This risk factor includes heritable biological traits that increase vulnerability to suicidal behavior. The poor prognosis subtype may include a biological diathesis to suicidal behavior.
We did not find any predictive associations between risk factors such as impulsivity or aggression, comorbidity with antisocial personality disorder, history of childhood maltreatment, and suicide attempts during the study interval, although each of these factors has been associated with suicidal behavior in borderline personality disorder in cross-diagnostic studies, psychological autopsy studies, or retrospective chart reviews of suicides (
9). Impulsivity is a diagnostic criterion for borderline personality disorder and is associated with number of suicide attempts but not with medical lethality. The McLean study showed that core symptoms of borderline personality disorder, including impulsivity, diminish over a 10-year period (
35). We observed that such borderline symptoms had no predictive value for suicidal behavior in the long term.
A review of deaths occurring in this study suggests that substance use disorders are a risk factor for premature death in patients with borderline personality disorder. Substance use disorders are common in this sample (59.6%). Although the diagnosis does not distinguish attempters (64%) from nonattempters (57.8%) or prospectively predict suicide attempts, the mortality associated with substance use disorders in our sample is a strong argument for early diagnosis and intervention for this comorbid condition.
We identified only one definite death by suicide at 6 years. Suicide rates vary widely among prospective studies, from 0.86% in the Collaborative Longitudinal Personality Disorders Study at 7 years (
39) to 4.1% in the McLean study at 10 years (
35). Recruitment source, which is related to illness severity, and prospective study designs may influence completion rates. Prospective studies rely on cooperative participants who comply with repeated follow-up interviews over many years. This design is required to assess the predictive power of predefined suicide risk factors; however, the resulting sample may exclude unstable patients who are more likely to drop out of treatment and complete suicide. With a mean age of 29 years, our sample is still not in the age range of highest risk for suicide and may experience further mortality in the years to come.
Our data suggest that outpatient treatment directed at enhancing family, social, and vocational functioning decreases the likelihood of suicidal behavior in borderline patients. However, our design does not permit inferences on treatment effectiveness, which would require random assignment to systematic treatments and comparison with control conditions. In a naturalistic design, it is likely that higher-functioning patients will choose to participate in treatment (and get the most out of it), while lower-functioning patients may not. This limits the interpretation of treatment participation in our data. Current treatment modalities for borderline personality disorder (e.g., dialectical behavior therapy and pharmacotherapy) are focused on symptomatic relief. A psychiatric rehabilitation model for borderline patients, emphasizing skills training and family involvement, may be required to improve long-term outcomes (
40).