Presently there are about 40 million Americans over the age of 65, and by 2030 that number is expected to grow to 72 million (
http://www.aoa.gov/AoARoot/Aging_Statistics/). The fastest-growing segment of the population is people over 80 (
http://transgenerational.org/aging/demographics.htm). Traditionally, aging has been viewed as a period of progressive decline in physical, cognitive, and psychosocial functioning and consequently, a growing health care burden on the society. Many believe that aging is the top public health problem we face today (
1), and the coming wave of aging baby boomers has been dubbed the “silver tsunami.” This negative view of old age contrasts with some exciting empirical research on older adults who continue to function well and are aging “successfully.” However, research advances in successful aging have been hampered by inconsistencies in operationalizing this construct—we found 29 different definitions of successful aging in 28 published studies on this topic (
2). Many of these investigations have focused primarily on physical health. The most widely used definition of successful aging, employed in the pioneering MacArthur studies (
3), is based on objective measures used by researchers to assess freedom from chronic disease and disability, along with high physical and cognitive functioning and social engagement. These studies are important because health care utilization and costs for older adults might be determined by such objective measures of successful aging. Moreover, this type of work may yield valuable information on modifiable factors, such as diet and exercise, to prevent or reduce physical disability.
A few studies that included subjective perceptions on aging indicated that at least some older adults felt they were aging successfully despite having substantive physical challenges (
5,
6). Self-assessments of successful aging have typically employed single items, e.g., questions such as, “How do you rate yourself on successful aging on a scale from 1 to 10?” or Likert-scale ratings of agreement with the statement “I am aging well” (
7,
8). Qualitative studies of successful aging (
9,
10) have shown that older adults center their definitions of successful aging on attitudinal factors, rather than merely physical health status.
The partial independence of self-rated successful aging from physical functioning suggests that successful aging should be conceptualized as a multidimensional construct. Pruchno et al. (
5) found empirical support for a two-factor model of successful aging consisting of subjective and objective components. Doyle et al. (
11) reported a multifactorial model of successful aging with interacting components including physical functioning and risk, activity, social engagement, and psychological traits such as confidence. Similarly, employing factor analysis in a convenience sample of postmenopausal women, our research group noted evidence supporting a model in which positive psychological traits seemed to interact with each individual's evaluation of her own physical and mental (but not cognitive) functioning, with the ultimate downstream outcome of importance to the individual’s successful aging (
12). However, such models have not been examined in large, randomly selected community samples with overrepresentation of old-old people and multipronged assessments. Greater understanding of significant associations of successful aging is likely to help identify potentially modifiable characteristics in the individual’s behavior or environment.
The goal of the present investigation was to study self-rated successful aging along with several specific domains of aging and positive psychological traits in randomly selected, community-based middle-aged and older adults, with oversampling of those over age 80. Given the normative age-related declines in physical and cognitive functioning, we hypothesized that older age would be associated with worse physical and cognitive functioning and lower self-ratings of successful aging. On the basis of the literature (
3,
5,
7,
8,
11,
12), we also hypothesized that self-rated successful aging would be positively related to physical, cognitive, and mental functioning and to positive psychological traits (
13). Finally, we hypothesized that in a multivariate analysis, physical and mental (but not cognitive) functioning and positive psychological traits would predict self-ratings of successful aging, as in our previous investigation (
12).
Results
Table 1 summarizes sociodemographic and other characteristics related to successful aging for each of the five age decades studied. The overall sample had a mean age of 77.3 years (SD=12.2), and the mean score for self-rated successful aging was 8.2 (SD=1.5). Older age was significantly associated with worse physical functioning (r=–0.35, N=945, p<0.001), objective cognitive functioning (r=–0.46, N=1,004, p<0.001), and subjective cognitive functioning (r=0.12, N=859, p=0.001), but it was also related to better mental functioning (r=0.12, N=945, p<0.001). Age was not related to the level of depression, optimism, or resilience. The bivariate associations of each potential correlate with self-rated successful aging are listed in
Table 2.
Contrary to our hypothesis, older age was associated with a higher score for self-rated successful aging. After adjustment for age, a higher self-rating of successful aging was associated with higher education, better objective and subjective cognitive functioning, better self-perceived physical and mental health, less depression, and greater optimism and resilience.
The best multiple regression model achieved with all the variables as potential correlates of self-rated successful aging is shown in
Table 3. This model accounted for 30% of the variance. We cross-checked these results using a random forests regression procedure (
27). In a model trained with the same variables obtained from the LASSO analysis, random forests produced an out-of-bag estimate of R
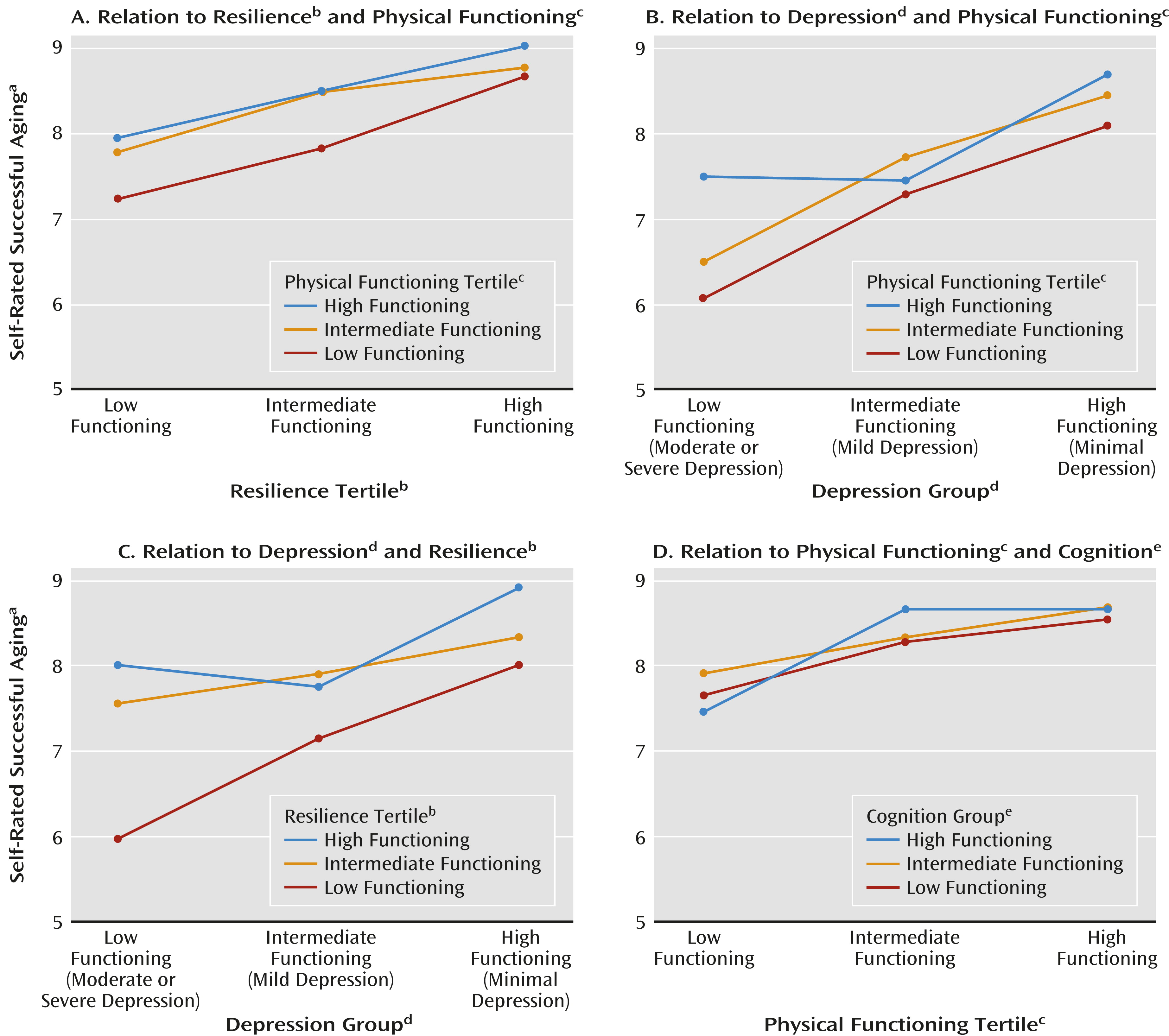
2 of 27%, indicating that the estimate was not biased upward from overfitting the data. Our model included resilience, depression, physical health, and age, entering the regression model in that order. Notably, cognitive impairment was not significant in the multiple regression analysis. Thus, while we did not find interactive effects, we did find independent additive effects in multiple regression analyses. These effects are displayed in
Figure 2, which illustrates scores for self-rated successful aging for pairs of variables by tertiles. These plots demonstrate relative effect sizes of different correlates of self-rated successful aging when the analysis controlled for other variables. Thus,
Figure 2a shows that
people in the bottom tertile of physical functioning who had high resilience (i.e., were in the top tertile of resilience) had self-ratings of successful aging similar to those of physically healthy people with low resilience. Likewise,
Figure 2b shows that people in the bottom tertile of physical functioning but with no or minimal depression had scores for self-rated successful aging comparable to those of physically healthy people with moderate to severe depression.
Discussion
Contrary to our hypothesis, older age was associated with higher self-ratings of successful aging, despite worse physical and cognitive functioning. The best multivariate model included greater resilience, lower depression, better physical health, and older age. Even though in bivariate analyses, self-rated successful aging was associated with physical health and cognitive functioning, which typically decline with age, older age was associated with higher self-rated successful aging. Resilience and depression seemed to have effects on successful aging with magnitudes that seemed at least comparable to that of physical health (
Figure 2).
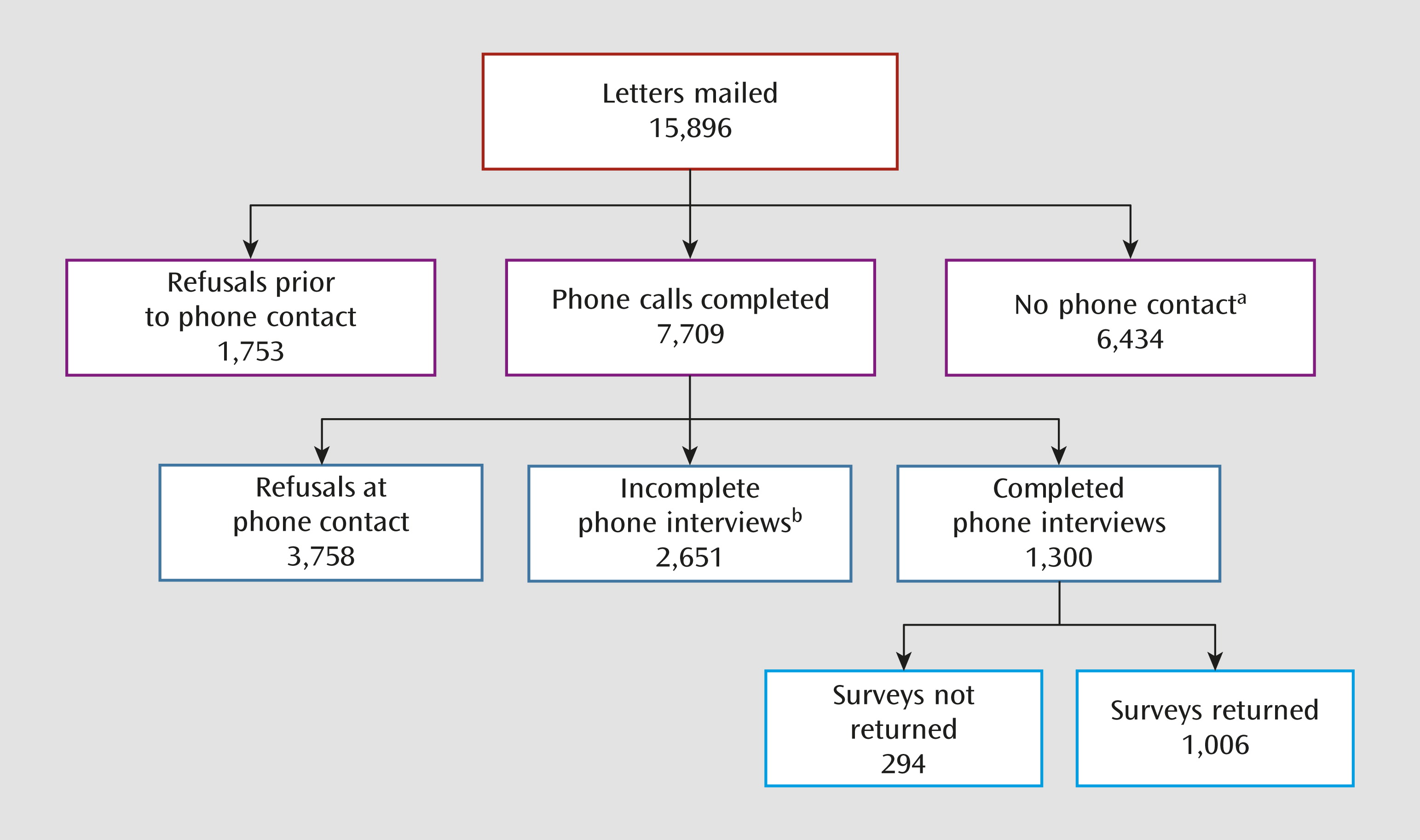
The SAGE investigation builds on the foundations of prior research into psychosocial aspects of successful aging (
5,
14,
28,
29). To our knowledge, this is the first study of self-rated successful aging to employ a large population-based sample of adults over 50 recruited with a structured multicohort design using list-assisted random-digit dialing procedures. Thus, except for the planned oversampling of adults over age 80, the present sample may be more representative of the broader community-dwelling population of older people than similarly aged samples of convenience. Also, in addition to assessing self-rated successful aging, participants were comprehensively characterized on self-reported physical and mental health and positive psychological traits, along with subjective and objective measures of cognitive functioning.
Our study has several limitations, especially the cross-sectional design and use of self-report-based assessments for most measures. Because of the cross-sectional nature of the data, a “potential survivor bias,” and more specifically a “community survival effect,” may confound interpretation of age effects. Since we excluded people in nursing homes or other institutions, it is possible that the positive association between greater self-rated successful aging and older age may be due to attrition of low-functioning (with low self-rated successful aging) older adults due to death or institutionalization. It should be noted, however, that in our sample, older age was associated with worse physical and cognitive functioning, i.e., our elderly group did not comprise exceptionally healthy seniors. Also, the survey response rate for people who completed our initial telephone interview was higher among 80–89-year-old individuals than in 50–59-year-old persons. Therefore, a survivor effect is unlikely to be the primary explanation for our findings. At the same time, the cross-sectional design prevents one from making causal inferences based on observed associations, e.g., whether higher resilience leads to greater self-rated successful aging or vice versa. Longitudinal follow-up may help specify causal relationships.
Another study limitation is that the data were collected through self-report measures (except for the Telephone Interview for Cognitive Status). It may be argued, for example, that optimism and self-rated successful aging are both self-rated and highly interrelated. However, optimism was not significant in the multiple regression model of successful aging. With self-reports, it is important to consider the likely influence of a tendency to give socially desirable responses on the validity of the results. However, in an earlier study of 1,860 nonrandomly selected community-dwelling older women, when we used the Marlowe-Crowne Social Desirability Scale we did not find evidence for a social desirability bias in most of the self-report measures of successful aging, including self-rated successful aging and physical and cognitive functioning (
30).
The relatively weak association between self-rated successful aging and objective cognitive functioning might be partially attributable to the use of the Telephone Interview for Cognitive Status, which is primarily a dementia screening measure. With a comprehensive neurocognitive battery, a stronger association between self-rated successful aging and objective cognitive functioning might have emerged.
Notwithstanding these limitations, our findings could be relevant to clinicians and researchers in at least three ways: modification of the attitude toward aging, use of self-rated successful aging as a meaningful outcome measure, and most important, the potential for enhancing successful aging by fostering resilience and treating or preventing depression. First, in terms of the attitude toward aging, most of the public discourse on population aging involves dire predictions and negative stereotypes. Yet the subjective experience of older people in our study seemed to improve with age even in the midst of physical and cognitive declines. The apparent trajectory of self-rated successful aging in middle and old age parallels published findings on well-being. Negative emotions have been reported to display a curvilinear relationship through the life course, with mental distress reaching a maximum in middle age and then decreasing progressively into later life, with an inverse change in positive emotions (
31). This finding of a counterintuitive increase in well-being with aging persists after accounting for the confounding influences of cohort, income, education, and marriage. Possible explanations for this paradoxical result include acceptance of physical limitations (
32,
33), contentedness with overall accomplishments in life (
34), a more realistic appraisal of one’s own strengths and limitations (
31), reduced preoccupation with social comparison (peer pressure), and greater emotional stability (
14,
35). Clinicians can help reduce societal ageism through their optimistic approach to the care of seniors. Further research on how older adults develop and maintain positive self-appraisals in the presence of biological declines may also inform similar adaptations across the lifespan.
Second, the present study illustrates the potential value of a subjective measure of overall functioning in later life, i.e., self-rated successful aging. Subjective outcomes are gaining increasing credence in intervention and services research (
4). At the individual level, self-rated health has been found to be a significant predictor of morbidity and mortality in old age (
36). At the population level, a large study of U.S. citizens living in different parts of the country (
37) correlated data on self-rated quality of well-being with objective indicators of quality of life—such as cost of living, environmental “greenness,” air quality, and local taxes—among people in the same region. The authors found a strong region-by-region match between subjective and objective well-being, attesting to the validity of self-reports of personal constructs. The subjective appraisal of overall aging by older adults themselves may be an important outcome in clinical practice and intervention research. For this to be useful as a patient-centered outcome, future longitudinal research would need to determine the responsiveness of self-rated successful aging to change and its applicability across cultures and population subgroups, including people with mental illnesses.
Finally, an important implication of the present study relates to the finding that resilience and depression were significantly associated with self-rated successful aging, with an effect comparable in size to that for physical health. While no causality can be inferred from these cross-sectional data, it is possible to speculate that increasing resilience and reducing depression might have effects on successful aging as strong as the effects of reducing physical disability. This finding points to an important role for psychiatry in enhancing successful aging in older adults, even in those with physical disabilities (
38). Resilience is often described in response to acute stressors, yet it may be an important aspect of maintaining well-being in the context of losses in functioning with aging (
39). To date there has been only limited research focused on enhancing positive psychological traits, such as resilience (
40,
41). We found a significant association between depression and self-rated successful aging despite the relatively low levels of depression in our sample, i.e., only a few of the respondents likely would have met the DSM-IV-TR criteria for major depression. Prior literature suggests that older adults are more likely to have subsyndromal depression than major depressive disorder (
42). The fact that even low levels of depressive symptoms appeared to influence self-rated successful aging suggests the potential value of interventions to treat or prevent subsyndromal depression in order to enhance successful aging. Greater understanding of the psychosocial and neurobiological underpinnings of the interaction between resilience and depression in older age (
43) may identify routes to promote successful aging.
In conclusion, the present results have important implications for psychiatry and aging. Perfect physical health is neither necessary nor sufficient for successful aging as defined by the older adults themselves. Their holistic self-appraisal involves strong emphasis on psychological factors such as resilience, optimism, and well-being, along with an absence of depression. Combined with evidence showing that traits such as resilience and optimism are associated with greater longevity and reduced physical morbidity (
11), with the reverse being true for depression, our findings suggest that psychiatry should take center stage within medicine and health care. Paralleling the recent positive psychology movement (
44), the time may be ripe for a “positive psychiatry” movement (
38).