Psychotic experiences are reported by approximately 5%–10% of the general population (
1,
2), although estimates differ substantially, partly because of variation in assessment methodologies, number of assessment items, and definitions of psychotic experiences (
3). Children reporting psychotic experiences are at greater risk of developing severe psychotic disorders later in life (
4), which suggests that psychotic experiences are on a phenotypic continuum with disorders such as schizophrenia (
5) and that these experiences represent an expression of vulnerability to psychotic disorder. This dimensional model of psychosis implies that similar etiological mechanisms underlie the range of phenotypes along this continuum and that psychotic experiences and psychotic disorders such as schizophrenia will share endophenotypes and risk factors (
6).
Impaired cognition has been regarded as a core feature of schizophrenia that often predates the development of psychosis in adulthood (
7). Deficits have been repeatedly and robustly detected in several cognitive domains, including attention, working memory, and executive function (
8). Processing speed has been identified as the single largest impairment, although it has been suggested that this observation may, at least in part, reflect the effects of psychotropic medication (
9). Nevertheless, these cognitive domains remain ill-defined because the cognitive measures are not equivalent in terms of established psychometric sensitivity and specificity (
10).
There has been less research conducted to date on the relationship between cognition and psychotic experiences in children, although earlier work has demonstrated that low IQ in childhood and decline in IQ and memory are related to a greater risk of developing psychotic experiences (
2,
7,
11). Findings from a longitudinal birth cohort twin study (
1) indicated that impaired social cognition was related to greater risk of psychotic experiences, but only weak evidence was found for an association between executive function and psychotic experiences. According to the study authors, this could be because the children in the sample were too young (5 years old) to exhibit executive function deficits in relation to psychosis. Whether or how other cognitive domains that are impaired in psychosis are related to psychotic experiences in children has not yet been examined in a large population-based study.
Additionally, although cognitive change in patients with schizophrenia has been investigated in clinical samples (
12) and epidemiological studies (
13), cognitive change in relation to psychotic experiences during adolescence, before the onset of schizophrenia, may be important to study but has only been examined in relatively small high-risk samples.
We set out to address this gap in the literature by exploring the longitudinal relationships in a birth cohort between psychotic experiences at age 12 years and key cognitive domains at ages 8, 10, and 11 years, selected a priori based on their association with psychosis and schizophrenia (
14). We hypothesized that impaired performance in these cognitive domains during childhood, as well as decline in the performance of these domains over time, would be related to psychotic experiences in children at age 12.
Method
Sample
The Avon Longitudinal Study of Parents and Children (ALSPAC;
http://www.bristol.ac.uk/alspac/) started in 1991 and 1992, when all pregnant women from a geographically defined region in the southwest of England were recruited. The initial ALSPAC cohort consisted of 14,062 live births and 13,988 infants still alive at 12 months (
15,
16). A total of 6,784 cohort members completed the Psychosis-Like Symptoms Interview at age 12. Variable numbers of these participants also completed other cognitive tests.
Ethical Approval
Ethical approval was obtained from ALSPAC’s Law and Ethics Committee and the local research ethics committees. Parents who enrolled their children in ALSPAC provided written informed consent at the time of enrollment, and they or their child are free to withdraw at any time.
Cognitive Assessments
All measures of cognitive domains were administered by trained psychologists. Cognitive tests were selected for analysis in this study a priori according to the Measurement and Treatment Research in Cognition in Schizophrenia (MATRICS) initiative (
14) on the basis that they were representative of the key cognitive domains identified as impaired in schizophrenia. The MATRICS framework served only as a loose concept, as not all of the selected cognitive measures corresponded perfectly to the MATRICS domains. Tests corresponding to four of the seven MATRICS cognitive domains were available.
Processing speed (ages 8 and 11).
Processing speed at age 8 was assessed using measures from two different tasks: 1) the sky search task, which was taken from the Tests of Everyday Attention for Children (
17), and 2) the coding subtest of the Wechsler Intelligence Scale for Children, 3rd edition (WISC-III;
18). Processing speed at age 11 was again assessed with the sky search task, but WISC-III was not administered at this age.
Attention/vigilance (ages 8 and 11).
The opposite worlds task from the Tests of Everyday Attention for Children (
17) was used to assess attention/vigilance at both ages. It should be noted that this test is related to but somewhat different from the attention/vigilance measure in the MATRICS.
Working memory (ages 8 and 10).
Working memory at age 8 was assessed using the backward digit span test and the arithmetic task from the WISC-III. At age 10, the counting span task (
19) was used to assess working memory, as the tests used at age 8 were not available.
Reasoning and problem solving (age 8).
The domain of reasoning and problem solving was assessed using the following WISC-III tasks: picture completion, picture arrangement, block design, and object assembly. A description of the cognitive tasks is provided in the data supplement that accompanies the online edition of this article.
The MATRICS procedure was used to incorporate all cognitive measures into cognitive domains, allowing consistency with a wider theoretical framework and limiting the number of statistical comparisons. As in the development of the MATRICS battery, we included multiple tests within domains where suitable tests were available, and this inclusion was supported by the observed high correlations of the tests within domains.
Assessment of Psychotic Experiences
The semistructured Psychosis-Like Symptoms Interview was conducted at age 12 (
2). Information on this interview is described in the online data supplement.
Our primary outcome measure was suspected or definite psychotic experiences (coded 1) or no psychotic experiences (coded 0). This approach was chosen rather than grouping suspected psychotic experiences together with no psychotic experiences, which has been criticized as being overconservative (
1).
Confounders
The variables examined as potential confounders were in the following domains: demographic characteristics (gender, parental education, parental social class, crowding index, and ethnic group), parental psychiatric problems, and development (developmental delay, assessed with the Denver Developmental Screening Test [
20], and behavioral/emotional difficulties, assessed with the total score from the Strengths and Difficulties Questionnaire [
21] at age 7).
Data Analysis
All cognitive measures were standardized to have a mean of zero and a standard deviation of 1. Children who scored more than three standard deviations from the mean were excluded from further analysis because their scores were unlikely to accurately reflect cognitive performance. We conducted sensitivity analyses whereby we included children with scores above or below three standard deviations from the mean by collapsing measures into quintiles, and the results from these analyses were similar to those excluding the children with extreme scores. Where domains were comprised of more than one test (e.g., working memory at age 8), a summary statistic was calculated by averaging and standardizing the z scores from the tests that comprised each domain. This procedure parallels the methodology used in the MATRICS, generating a summary statistic that represents the score of each child in this domain.
Logistic regression analyses were conducted in Stata, version 11 (StataCorp, College Station, Tex.) to estimate odds ratios and 95% confidence intervals for associations between cognitive domains and psychotic experiences at age 12. To facilitate interpretation of the results, the cognitive measures were recoded so that higher score indicated worse performance. Seven independent regressions were conducted to determine whether the independent variables (the scores on each of the seven neurocognitive domains) predicted group status (0=children without psychotic experiences, 1=children with psychotic experiences). These associations were subsequently adjusted for possible confounders. To examine whether the associations for any of the cognitive domains were independent of one another, we also adjusted for all other cognitive domains (domains at ages 10 and 11 were adjusted only for earlier measures of the different domains).
We examined nonlinear relationships between the cognitive domains and psychotic experiences by examining likelihood ratio tests for the addition of quadratic as well as linear terms to the models.
Because of the problems of repeated measures when examining change (
22), we examined change in cognitive performance over time by applying principal components analysis to measures of both time points. This identified two factors (s1 and s2) for each cognitive domain, where s1 represented the average performance across both time points and s2 represented change. We used logistic regression analysis to test for associations between s2 and psychotic experiences after adjusting for s1.
Missing Data
The cognitive performance of children who were not assessed with the Psychosis-Like Symptoms Interview at age 12, along with information regarding the imputation analysis, is described in the online data supplement.
Results
Cognitive Domains and Psychotic Experiences at Age 12
Among the children interviewed, 787 (11.6%, 95% CI=10.9%–12.4%) had suspected or definite psychotic experiences. A descriptive summary of children’s cognitive performance is presented in
Table 1.
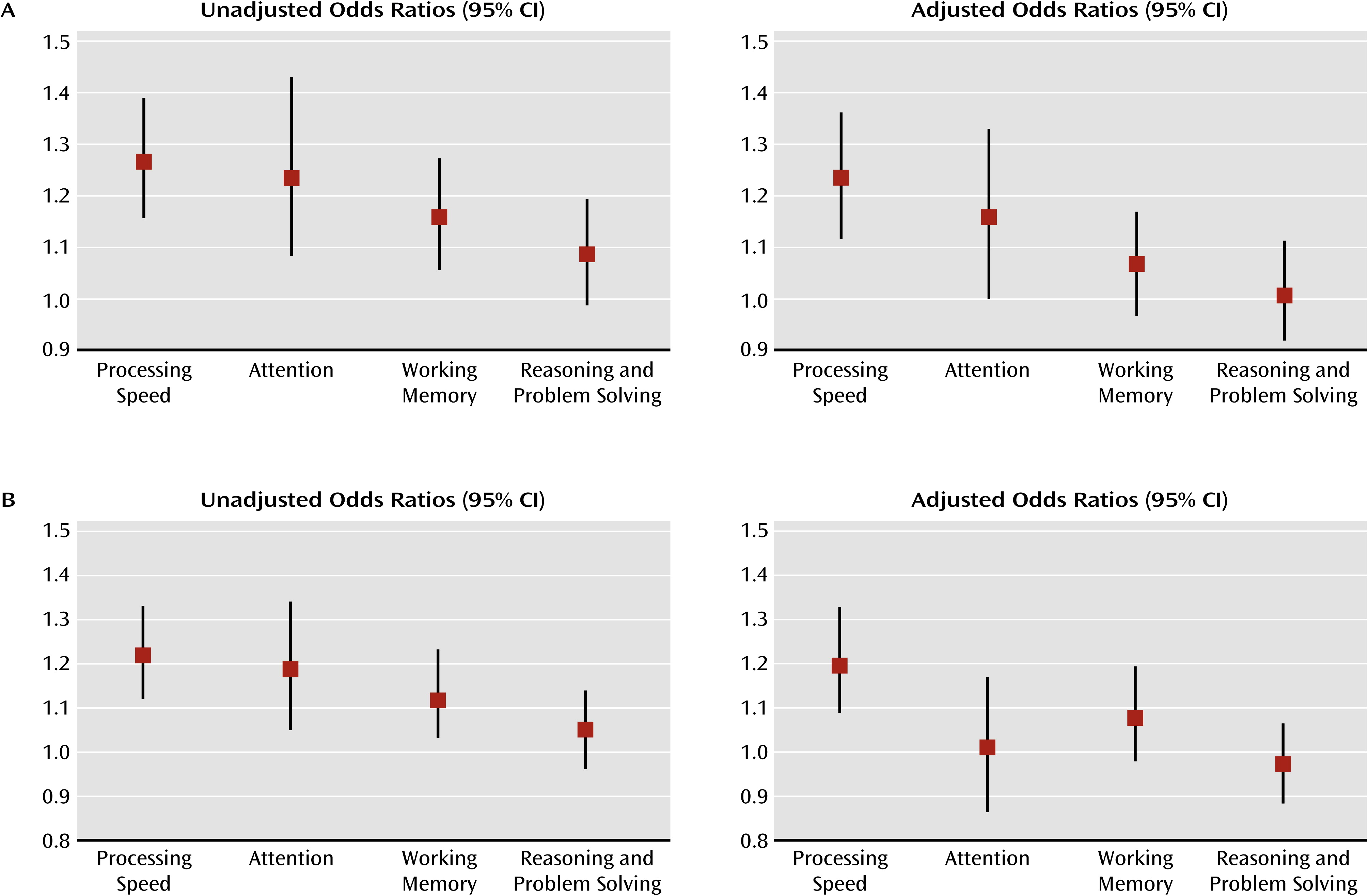
Poorer performance in the domains of processing speed (age 8), attention (ages 8 and 11), and working memory (ages 8 and 10) was associated with greater risk of psychotic experiences (
Table 2 and
Figure 1), but the domain of reasoning and problem solving (age 8) was more weakly associated. There was weak evidence for a nonlinear relationship between performance in the domain of reasoning and problem solving (p=0.032) and risk of developing psychotic experiences.
Of the potential confounders, parental social class, crowding index, ethnic group, parental psychiatric problems, and developmental delay had no effect on the associations and therefore were not included in the analyses.
Most associations changed only slightly after adjusting for gender and maternal education (
Tables 2 and
3 and
Figure 1). Adjusting for behavioral and emotional difficulties attenuated most associations somewhat, but the associations between psychotic experiences and processing speed at age 8 and attention at age 11 remained. We found weak evidence for an association between psychotic experiences and attention at age 8 and working memory at age 10 after these adjustments. After exploring the separate effects of the Strengths and Difficulties Questionnaire subscales, it seemed that the hyperactivity and peer problems subscales had the greatest effects on attenuating the associations between cognition and psychotic experiences. The results of the individual tests are described in the online data supplement.
We also examined the extent to which performance on these cognitive domains affected psychotic experiences independently of one another. When adjusting for other cognitive domains, only processing speed remained associated with greater risk of psychotic experiences at age 12 (
Table 4 and
Figure 1).
We conducted further logistic regressions as sensitivity analyses, in which we adjusted all cognitive domains at age 8 separately for processing speed at age 8. This produced results similar to those of the analysis that adjusted for all the cognitive domains (attention [p=0.76], working memory [p=0.15], and reasoning and problem solving [p=0.80]). Generally, these findings revealed that processing speed had the strongest effect of all the cognitive domains examined.
Finally, of the children who scored below the 25th percentile in the domains of processing speed (age 8) and attention (age 11), only 14% and 12%, respectively, reported psychotic experiences at age 12.
Change Over Time in Cognitive Performance and Psychotic Experiences at Age 12
All domains correlated positively with one another across ages at p<0.001, which supported the subsequent examination of change over time (see Table S3 of the online data supplement). Summary scores of change are presented in
Table 5.
Logistic regression analyses based on factors identified by the principal components analysis revealed that decline of processing speed over time was associated with greater odds of psychotic experiences (odds ratio=1.29, 95% CI=1.15–1.45, p<0.001). As a sensitivity analysis, we also calculated change by using only the sky search task at both time points, and the results were similar. There was weaker evidence of an association between risk of developing psychotic experiences and decline of attention (odds ratio=0.94, 95% CI=0.82–1.07, p=0.33), and there was no evidence of an association for decline of working memory (odds ratio=0.99, 95% CI=0.88–1.10, p=0.78).
Missing Data
Results from the multiply imputed data sets were similar to those from the main data set when both outcomes and confounders or only confounders were imputed, and these did not change any of the substantive findings. To be more specific, sample attrition appears to have led to an underestimation of the associations between the cognitive domains and psychotic experiences (section SA2 in the online data supplement).
Discussion
Cognitive Domains and Psychotic Experiences
Our results show that lower performance in the domains of processing speed, attention, and working memory was associated with a greater risk of the later development of psychotic experiences in children. The associations were not explained by the background characteristics that were adjusted for, but some domains were attenuated substantially after adjustment for behavioral and emotional difficulties. Associations between psychotic experiences and processing speed at age 8 and attention at age 11 remained after these adjustments.
By adjusting for behavioral and emotional difficulties over and above background factors, we may have been overly conservative if these are on the causal pathway between cognitive ability and psychotic experiences. However, it is also possible that behavioral problems contribute to impaired performance on cognitive tests (e.g., poor concentration), in which case adjustment presents a clearer picture of the relationships we sought to evaluate in this study.
Impaired Processing Speed and Psychotic Experiences
When all other cognitive domains were adjusted for, processing speed was most strongly related to psychotic experiences, which is in line with the existing literature describing processing speed as a fundamental cognitive construct close to the core of psychosis (
23). This finding linking processing speed performance with psychotic experiences cannot be ascribed to the effects of medication as has been recently suggested (
9), given that none of the children in this study had ever taken psychotropic medication.
Nevertheless, taking into account that a proportion of the genetic variance for schizophrenia is shared with that of cognition (
24), the association between processing speed and psychotic experiences might result from pleiotropic genetic effects and other confounders. Furthermore, reverse causation, whereby psychotic experiences that are present before age 8 result in impaired cognitive performance, cannot be excluded as we do not have measures of psychotic experiences at this age. It is difficult to distinguish magical thinking from psychotic experiences in younger children. Indeed, the ages of 11 and 12 have been suggested as ideal for the assessment of psychotic experiences, as children around this age are still unaware of the consequences of revealing such experiences (such as stigmatization and social rejection) and are therefore less inhibited about sharing them (
1).
If processing speed deficits are causally related to psychotic experiences, then one possible mechanism might be an increase in false prediction errors, that is, failure to efficiently inform one’s existing beliefs about what the world probably looks like in the face of new evidence (
25). Disturbed brain connectivity has been suggested as a probable mechanism that could lead to false prediction errors (
25) and has also been associated with both hallucinations (
26) and reduced processing speed (
27). Research in healthy children and patients with adolescent-onset psychosis has shown that cognitive slowing might restrict performance in other cognitive processes, such as executive function (
28). Therefore, abnormal brain connectivity could affect processing speed, which in turn could restrict the optimal performance of other cognitive operations, resulting in false prediction errors and thus positive symptoms.
Attention
Attention also appeared to be related to psychotic experiences independent of confounding, although these effects did not persist when we adjusted for processing speed. Impaired attention has been systematically reported in children at high risk of developing schizophrenia (
29). Moreover, according to findings from the Israeli Kibbutz-City high-risk study, impaired attention at age 11 predicted the development of schizophrenia (
30). Similar results were reported by the New York High-Risk Project (
31). It should be noted, however, that processing speed was not adjusted for in these studies.
Change in Cognition Over Time
To our knowledge, this is the first study to examine the change in performance in cognitive domains over time in relation to psychotic experiences in a population-based sample of children. Our finding that decline in processing speed may be particularly associated with the later development of psychotic experiences further supports the existence of an aberrant neurodevelopmental process in children at high risk of developing schizophrenia and is in agreement with the schizophrenia literature (
13). Whether or how premorbid decline in attention over time manifests in individuals with schizophrenia has not yet been examined. In contrast to previous findings (
13), we did not find evidence of an association between decline in working memory over time and psychotic experiences. We cannot exclude the possibility that this discrepancy may be due to different measures of working memory over time in our study. Other possibilities for not finding evidence of decline include repeated testing and differential practice effects between the children with and without psychotic experiences.
Theoretical Implications
Our findings support a dimensional model of psychotic experiences, with psychotic disorder at the extreme end. In clinical populations, the cognitive domains we examined have been found to be associated with schizophrenia; in accordance with the dimensional model, we would expect the same associations to exist between cognitive function and psychotic manifestations, if to a lesser degree. Indeed, the effect sizes of the cognitive domains reported in our study, although smaller, followed the same pattern as those reported in a number of meta-analyses of schizophrenia patients and healthy comparison subjects (
9,
23,
32–
35). For example, in our study, processing speed at age 8 had the largest, albeit still small, effect size (Hedge’s g=−0.195, 95% CI=−0.279 to −0.111), followed by working memory (g=−0.115, 95% CI=−0.199 to −0.031) and attention (g=−0.114, 95% CI=−0.198 to −0.030).
On the other hand, not all cognitive domains were associated with psychotic experiences. The effect size of the domain of reasoning and problem solving did not reach significance (g=−0.041, 95% CI=−0.125 to 0.043), whereas the effect sizes reported in meta-analyses of schizophrenia (
33,
34) ranged from −1.06 to −0.53. Although type II errors cannot be excluded, another explanation could be that the tasks used in the meta-analyses (e.g., the Wisconsin Card Sorting Test) were different from the ones used in our study. Furthermore, although the domain of reasoning and problem solving has been identified as a separable impaired cognitive domain in schizophrenia, there is evidence that the impairments of patients with positive symptoms are not of a general reasoning nature (
36) but are more specific, and such specificity could explain the observed lack of associations.
Furthermore, the fact that the associations between processing speed at age 11 and psychotic experiences were weak could be a result of practice effects or because the children had developed cognitively and therefore performed better on the test.
Strengths and Limitations
Our study focused on psychotic experiences and not psychotic disorder. Nevertheless, such experiences are an integral part of diagnosis for any psychotic disorder; they are associated with substantial adverse outcomes in social achievement and functioning in their own right (
37), and psychotic experiences in childhood are strongly associated with psychotic disorders in adult life (
4). Our finding that processing speed is the strongest predictor of psychotic experiences, irrespective of psychotropic medication, indicates that the mechanisms mediating the association between impaired cognition and schizophrenia also mediate the association between impaired cognition and psychotic experiences. Thus, our study provides further insight into understanding the pathogenesis of psychotic phenomena and the cognitive deficits that may place children at higher risk of developing schizophrenia. The predictive value of the findings is rather limited (only 14% of the children who scored below the 25th percentile for the processing speed domain developed psychotic experiences), and the predictive value of psychotic experiences for uncommon disorders such as schizophrenia is also likely to be low (
38). Nevertheless, these findings assist in better characterizing and defining the cognitive mechanisms associated with elevated psychopathological risk, and they inform potential prevention strategies.
One of the limitations of this study is that we were not able to test all the MATRICS domains because they had not all been assessed in our study sample. Therefore, the results could be confounded by another underlying cognitive domain that was not examined. Moreover, a common criticism of neuropsychological tests is that they do not measure cognitive processes in isolation (
10), and our tests may have been less than perfect in capturing the specific cognitive domains. For example, the arithmetic test (which we classified as part of the working memory domain) might overlap to some extent with the domain of reasoning and problem solving. Differential loss to follow-up could introduce attrition bias, although our imputation analyses indicated that missingness is unlikely to have biased the observed relationships.
Conclusions
We examined the longitudinal relationships between cognitive domains previously associated with schizophrenia (
14) and psychotic experiences in children in a large birth cohort. Our findings suggest that processing speed and attention are related to higher risk of psychotic experiences in children, with processing speed being the key cognitive feature. Additional research is required to determine whether this has implications for the higher risk of subsequent psychotic disorder associated with psychotic experiences in children and whether potential future interventions to improve processing speed might lead to a decrease in the incidence of psychotic experiences or to fewer transitions to psychotic disorders in at-risk populations.
Acknowledgments
The authors thank all the families who took part in this study, the midwives for their help in recruiting them, and the whole Avon Longitudinal Study of Parents and Children team.