The Separation Anxiety Hypothesis of Panic Disorder Revisited: A Meta-Analysis
Abstract
Objective
Method
Results
Conclusions
Method
Search Strategy and Inclusion Criteria
| Study | Group (Disorder) | Study Participants N | Mean Age or Range | SD | Female (%) | Study Design | Sample Type | Outcome | Comparison Group | Clinical Control Disorder | Separation Anxiety Disorder Measure | Separation Anxiety Disorder Measure Criteria | Informant | STROBE Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Aschenbrand et al. (2003) | Clinical control;separation anxiety disorder | 6718 | 19.3 (Total sample) | 1.7 | 36 | Prospective cohort | Clinical | Anxiety disorders; major depressive disorder; panic disorder | Clinical control | Generalized anxiety disorder; social phobia | Interview | DSM-III-R | Parent and child | 18.5 |
| Ayuso et al. (1989) | Nonclinical control; panic disorder | 50 107 | No data 35.1 | 9.0 | 65 | Case control | Clinical | Panic disorder | Nonclinical control | Checklist | DSM-III | Proband | 11 | |
| Balon et al. (1989) | Nonclinical control; | 100 | 29.5 | 5.9 | 55 | Case control | Clinical | Panic disorder | Nonclinical control | Checklist | DSM-III | Proband | 7 | |
| panic disorder | 100 | 32.8 | 8.0 | |||||||||||
| Bandelow et al. (2001) | Nonclinical control; panic disorder | 124 | 36.8 | 11.6 | 58 | Case control | Clinical | Panic disorder | Nonclinical control | Interview; checklist | DSM-IV | Proband | 16.5 | |
| 115 | 38.1 | 10.6 | ||||||||||||
| Battaglia et al. (1995) | Nonclinical control; | 131 | 37.3 | 12.0 | 68 | Case control | Clinical | Panic disorder | Nonclinical control | Panic disorder; major depressive disorder; social phobia; simple phobia | Checklist | DSM-III-R | Proband | 14.5 |
| panic disorder | 231 | 36.3 | 11.0 | |||||||||||
| Biederman et al. (2005)b | Nonclinical control referred; | 61 | 38.3 | 5.1 | 48 | Case control | Population | Panic disorder | Nonclinical control | Interview | DSM-III-R | Proband | 17.5 | |
| panic disorder in referred sample; | 131 | 38.8 | 5.4 | 85 | ||||||||||
| nonclinical control nonreferred; | 587 | 42.4 | 5.8 | |||||||||||
| panic disorder in nonreferred sample | 58 | 40.5 | 6.4 | |||||||||||
| Biederman et al. (2005)c | Nonclinical control; | 686 | 42.1 | 6.0 | 51 | Case control | Population | Major depressive disorder; panic disorder | Nonclinical control | Interview | DSM-III-R | Proband | 15.5 | |
| panic disorder; | 23 | 42.5 | 5.5 | |||||||||||
| major depressive disorder | 225 | 41.8 | 5.9 | |||||||||||
| Biederman et al. (2006) | Nonclinical control; | 960 | 42.0 | 6.0 | 51 | Case control | Population | Panic disorder | Nonclinical control | Interview | DSM-III-R | Proband | 17.5 | |
| panic disorder | 58 | 40.5 | 6.4 | |||||||||||
| Biederman et al. (2007) | Separation anxiety disorder; | 41 | 6.4 (Total sample) | No data | No data | Prospective cohort | Population | Major depressive disorder; panic disorder | Non-separation anxiety disorder | Interview | DSM-III-R | Parent and child | 16.5 | |
| non-separation anxiety disorder | 192 | |||||||||||||
| Bittner et al. (2007) | Separation anxiety disorder; | 68 | 9–19 (Total sample) | 50 | Prospective cohort | Population | Major depressive disorder; substance dependence | Non-separation anxiety disorder | Interview | DSM-IV | Parent and child | 17 | ||
| non-separation anxiety disorder | 812 | |||||||||||||
| Brückl et al. (2007) | Separation anxiety disorder; | 17 | 14–17 (Total sample) | 52 | Prospective cohort | Population | Anxiety disorders; major depressive disorder; panic disorder; substance dependence | Non-separation anxiety disorder | Interview | DSM-IV | Child | 15.5 | ||
| subthreshold separation anxiety disorder; | 99 | |||||||||||||
| symptomatic separation anxiety disorder; | 86 | |||||||||||||
| non-separation anxiety disorder | 888 | |||||||||||||
| Flakierska-Praquin et al. (1997) | Nonclinical control | 35 | 7–12 (Total sample) | 54 | Prospective cohort | Clinical | Anxiety disorders; major depressive disorder; panic disorder; substance dependence | Clinical control, nonclinical control | Oppositional disorder; attention deficit disorder; dysthymia; anxiety disorders; OCD; tics; reading disorder; enuresis/encopresis; atypical stereotyped movement disorder; adjustment disorder | Medical records | DSM-III | No information provided | 15.5 | |
| clinical control; | 35 | |||||||||||||
| separation anxiety disorder | 35 | |||||||||||||
| Gregory et al. (2007) | Nonclinical control; | 640 | 32 (Total sample) | No data | 62 | Case control | Population | Panic disorder | Non-separation anxiety disorder | Interview; checklist | DSM-III | Parent and child | 12 | |
| clinical control; | 307 | |||||||||||||
| panic disorder | 16 | |||||||||||||
| Hayward et al. (2000) | Major depressive disorder; non-separation anxiety disorder | 1241,917 | 15.4 (Total sample) | 0.9 | 47 | Prospective cohort | Population | Major depressive disorder | Non-separation anxiety disorder | Interview | DSM-III-R | Child | 13.5 | |
| Hayward et al. (2003) | Panic disorder; clinical control | 122,342 | 15.4 (Total sample) | 0.9 | 47 | Case control | Population | Panic disorder | Nonclinical control | No information provided | Interview | DSM-III-R | Child | 12.5 |
| Lewinsohn et al. (2008) | Nonclinical control; | 457 | 16.1 (Total sample) | No data | No data | Prospective cohort | Population | Anxiety disorders; major depressive disorder; panic disorder; substance dependence | Clinical control, nonclinical control | Affective disorder; nonaffective disorder; psychotic disorder; adjustment disorder | Interview | DSM-III-R | Child | 17.5 |
| clinical control; | 389 | |||||||||||||
| separation anxiety disorder; | 42 | |||||||||||||
| anxiety disorders | 88 | |||||||||||||
| Lipsitz et al. (1994) | Panic disorder; | 156 | 34.5 (Total sample) | 8.4 | 59 | Case control | Clinical | Panic disorder | Clinical control | Panic disorder; social phobia; OCD | Interview | DSM-III-R | Proband | 13.5 |
| social phobia; | 106 | |||||||||||||
| OCD; | 51 | |||||||||||||
| Mroczkowski et al. (2011) | Clinical control; | 390 | 42.2 | 14.7 | 71 | Retrospective cohort | Clinical | Major depressive disorder; panic disorder; substance dependence | Non-separation anxiety disorder | Interview | DSM-IV | Proband | 13 | |
| separation anxiety disorder | 80 | 34.2 | 12.9 | |||||||||||
| Otto et al. (2001) | Panic disorder; | 133 | 36.4 | 9.7 | 34 | Case control | Clinical | Panic disorder | Clinical control | Social phobia | Interview | DSM-III-R | Proband | 13.5 |
| social phobia | 97 | |||||||||||||
| Pine et al. (1998) | Non-separation anxiety disorder; | 601 | 9–18 (Total sample) | No data | 50 | Prospective cohort | Population | Major depressive disorder; panic disorder | Non-separation anxiety disorder | Interview | DSM-III; DSM-III-R | Parent and child | 15 | |
| separation anxiety disorder | 111 | |||||||||||||
| Pini et al. (2005) | Nonclinical control; | 15 | 27.1 | 6.0 | 54 | Case control | Clinical | Major depressive disorder; panic disorder | Nonclinical control | Interview | DSM-IV | Proband | 13.5 | |
| panic disorder; | 24 | 32.5 | 9.3 | |||||||||||
| major depressive disorder | 20 | 45.6 | 8.3 | |||||||||||
| Pini et al. (2010) | Non-separation anxiety disorder; | 250 | 42.0 | 12.1 | 66 | Case control | Clinical | Major depressive disorder; panic disorder; anxiety disorders | Non-separation anxiety disorder | Interview | DSM-IV | Proband | 14.5 | |
| adult separation anxiety disorder with history of childhood separation anxiety; | 110 | 39.4 | 13.3 | |||||||||||
| separation anxiety disorder | 43 | 36.9 | 10.5 | |||||||||||
| Raskin et al. (1982) | Clinical control; | 16 | 21–54 | No data | 70 | Case control | Clinical | Panic disorder | Clinical control | Generalized anxiety disorder | No information provided | DSM-III | Proband | 10.5 |
| panic disorder | 17 | 24–60 | ||||||||||||
| Silove et al. (2002) | Non-separation anxiety disorder; | 20 | 45.0 (Total sample) | 15.0 | 65 | Retrospective cohort | Population | Major depressive disorder; panic disorder | Non-separation anxiety disorder | Interview; checklist | DSM-IV | Proband | 14 | |
| separation anxiety disorder | 52 | |||||||||||||
| Yeragani et al. (1989) | Nonclinical control; | 30 | 33.4 | 6.2 | 54 | Case control | Clinical | Major depressive disorder; panic disorder | Nonclinical control | Checklist | DSM-III | Proband | 7.5 | |
| panic disorder; | 35 | 29.6 | 6.3 | |||||||||||
| major depressive disorder | 24 | 31.7 | 5.1 |
Quality Assessment
Data Extraction and Analysis
Results
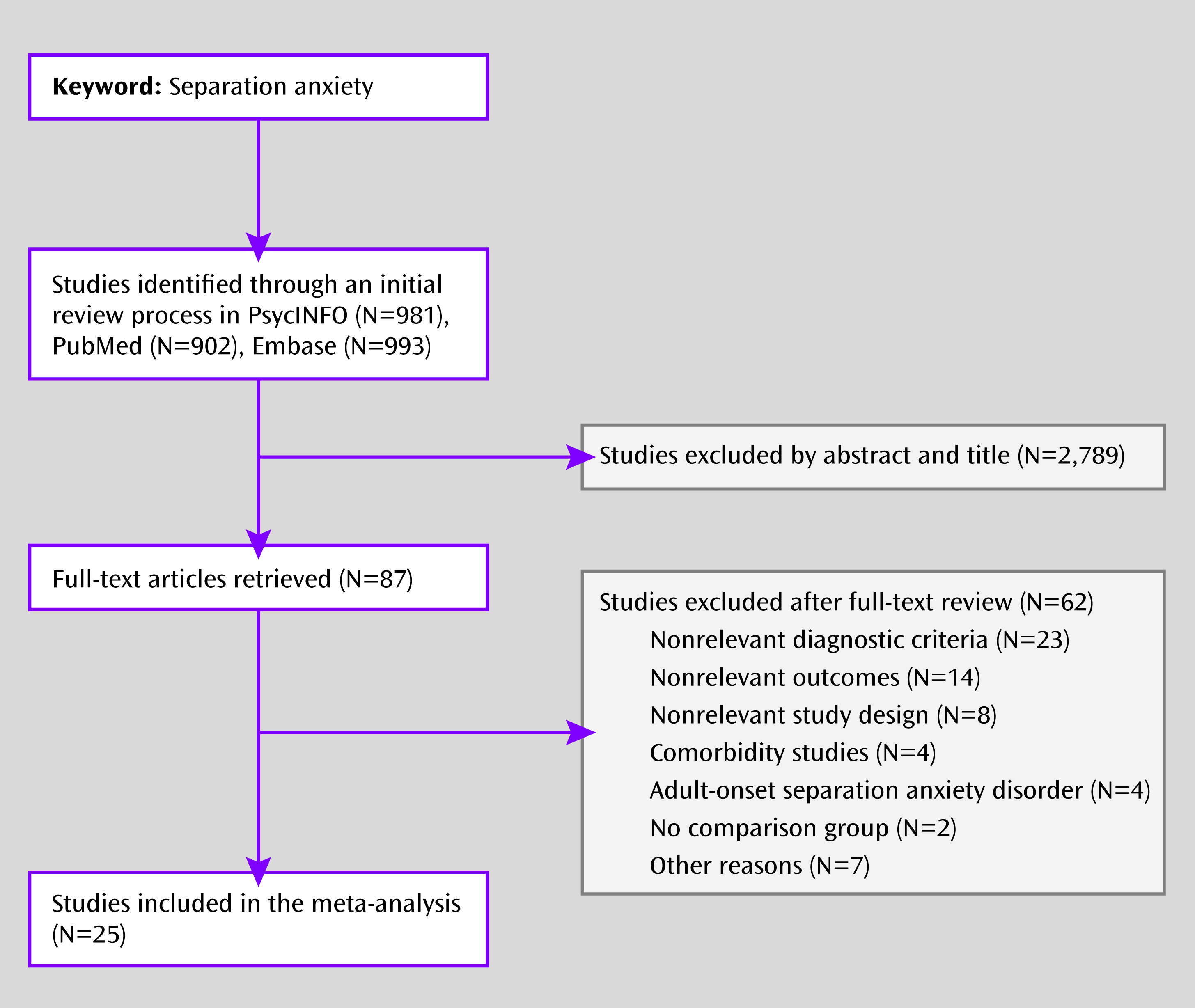
Study Selection
Association Between Separation Anxiety Disorder and Future Mental Disorders
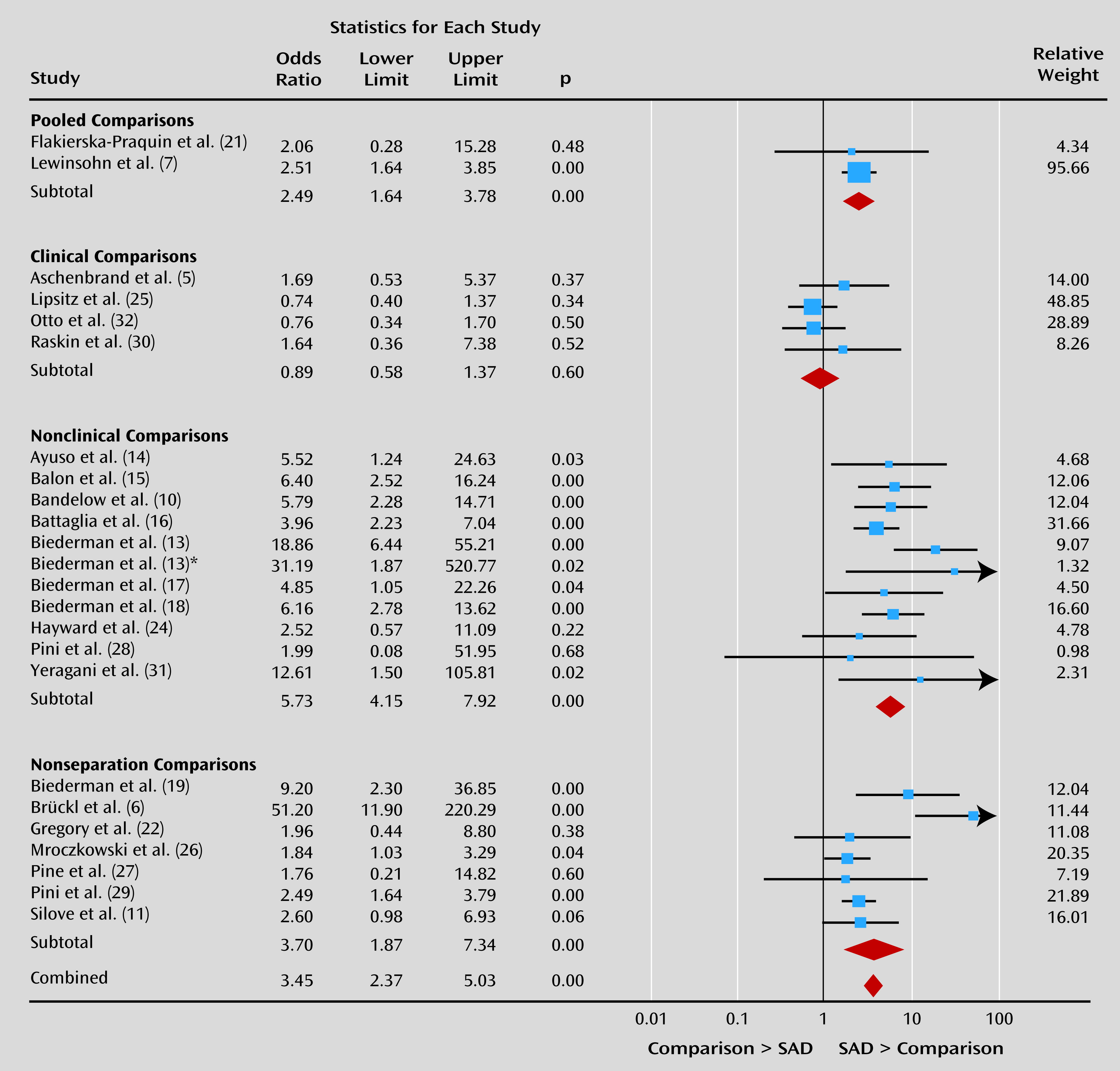
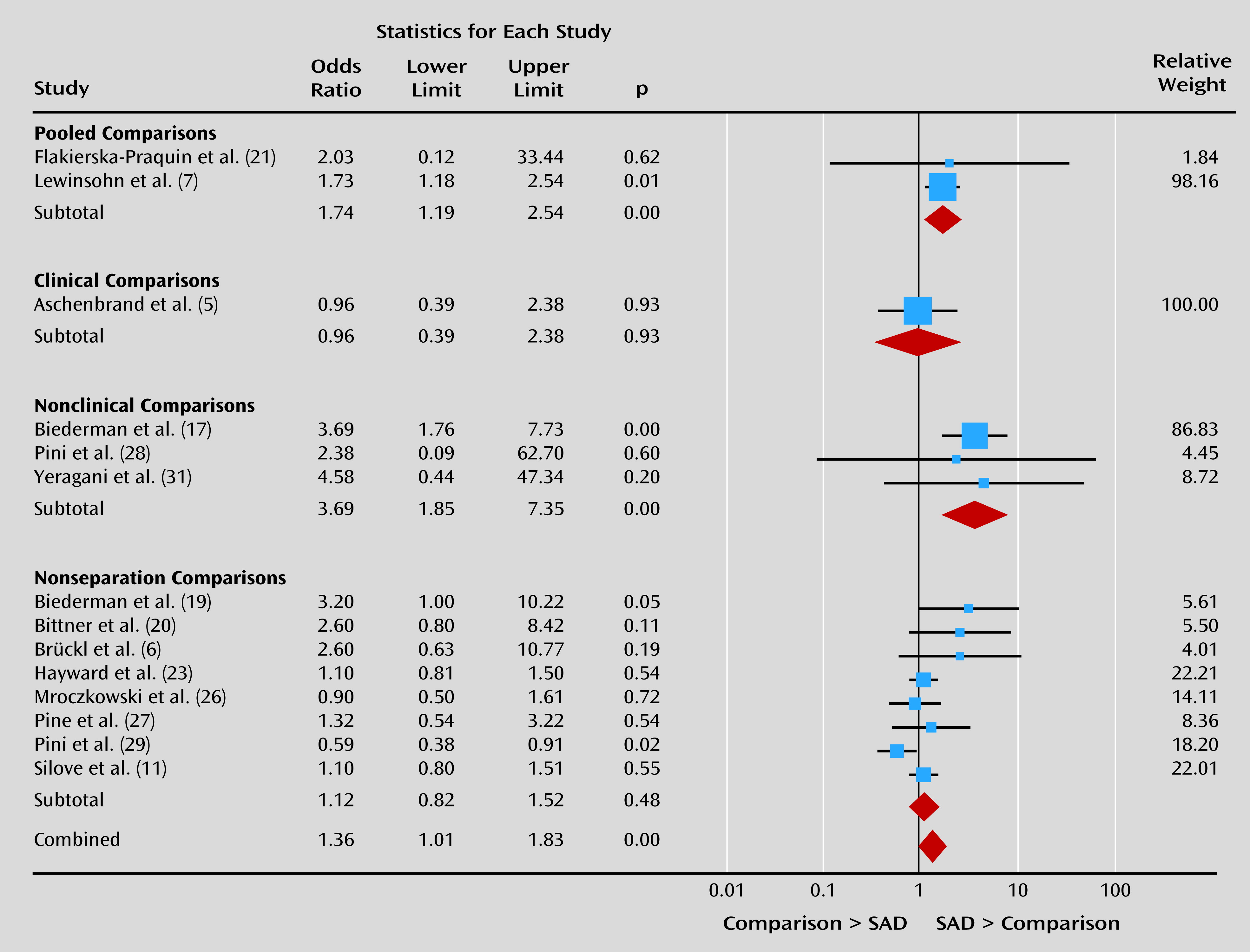
Sensitivity Analyses and Moderator Variables
| Variable | Outcome | |||
|---|---|---|---|---|
| Panic Disorder | df or 95% CI | Major Depressive Disorder | df or 95% CI | |
| Publication bias | ||||
| Funnel plot distribution | Symmetrical | Asymmetrical | ||
| Begg’s adjusted-rank correlation (p value) | 0.45 | 0.29 | ||
| Classic fail-safe N | 782 | 26 | ||
| Comparison group | ||||
| Separation anxiety disorder compared with clinical control | ||||
| Heterogeneitya | 0.00 | 3 | 0 | 0 |
| Heterogeneityb | 0 | 0 | ||
| Odds ratio | 0.89 | 0.58–1.37 | 0.96 | 0.39–2.38 |
| Separation anxiety disorder compared with non-separation anxiety disorder | ||||
| Heterogeneitya | 71.09** | 6 | 53.28* | 7 |
| Heterogeneityb | 0.51 | 0.09 | ||
| Odds ratio | 3.70 | 1.87–7.34 | 1.04 | 0.87–1.24 |
| Separation anxiety disorder compared with nonclinical control | ||||
| Heterogeneitya | 0.00 | 10 | 0.00 | 2 |
| Heterogeneityb | 0 | 0 | ||
| Odds ratio | 5.73 | 4.15–7.92 | 3.69 | 1.85–7.35 |
| Odds ratio of nonclinical control compared with odds ratio of clinical controlc | 6.78*** | 2.32* | ||
| Odds ratio of nonclinical control compared with odds ratio of non-separation anxiety disorderc | 1.13 | 3.49*** | ||
| Odds ratio of clinical control compared with odds ratio of non-separation anxiety disorderc | 3.45*** | 0.17 | ||
| Study type | ||||
| Case control | ||||
| Heterogeneitya | 74.80*** | 15 | 79.71*** | 4 |
| Heterogeneityb | 0.58 | 0.63 | ||
| Odds ratio | 3.36 | 2.09–5.41 | 1.43 | 0.59–3.45 |
| Prospective | ||||
| Heterogeneitya | 68.50** | 6 | 12.57 | 7 |
| Heterogeneityb | 0.79 | 0.02 | ||
| Odds ratio | 4.08 | 1.75–9.52 | 1.43 | 1.11–1.86 |
| Retrospective cohort | ||||
| Heterogeneitya | 0 | 0 | 0 | 0 |
| Heterogeneityb | 0 | 0 | ||
| Odds ratio | 2.60 | 0.98–6.93 | 1.10 | 0.80–1.51 |
| Odds ratio of case control compared with odds ratio of prospectivec | 0.39 | 0 | ||
| Odds ratio of case control compared with odds ratio of retrospectivec | 0.46 | 0.55 | ||
| Odds ratio of prospective compared with odds ratio of retrospectivec | 0.68 | 1.25 | ||
| DSM criteria | ||||
| DSM-III/DSM-III-R | ||||
| Heterogeneitya | 69.61*** | 18 | 70.85*** | 8 |
| Heterogeneityb | 0.47 | 0.24 | ||
| Odds ratio | 3.18 | 2.11–4.81 | 1.45 | 0.94–2.23 |
| DSM-IV/DSM-IV-TR | ||||
| Heterogeneitya | 82.65*** | 3 | 1.51 | 4 |
| Heterogeneityb | 1.58 | 0 | ||
| Odds ratio | 4.79 | 1.13–20.29 | 1.14 | 0.87–1.50 |
| Odds ratio of DSM-III compared with odds ratio of DSM-IVc | 0.53 | 0.92 | ||
| Sample type | ||||
| Clinical | ||||
| Heterogeneitya | 67.55*** | 13 | 3.14 | 5 |
| Heterogeneityb | 0.38 | 0.01 | ||
| Odds ratio | 2.40 | 1.53–3.76 | 0.77 | 0.55–1.07 |
| Population | ||||
| Heterogeneitya | 68.22*** | 10 | 56.51* | 7 |
| Heterogeneityb | 0.65 | 0.10 | ||
| Odds ratio | 5.63 | 3.01–10.50 | 1.63 | 1.18–2.25 |
| Odds ratio of clinical compared with odds ratio of populationc | 2.17* | 3.17** | ||
Discussion
References
Information & Authors
Information
Published In
History
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).

