The provision of psychiatric treatment via live interactive videoconferencing, frequently termed telepsychiatry, has been employed since the 1950s, but only in the past decade has it reached maturation and broad use as a treatment modality (
1). A growing body of scientific evidence, coupled with burgeoning implementation, is demonstrating telepsychiatry’s ability to bring care closer to patients and to increase the range and quality of available mental health services (
2–
8). The past decade has witnessed the extension of telepsychiatry services from larger institutional programs (e.g., the Department of Veterans Affairs, health maintenance organizations) where patients are seen within a clinic or hospital, often referred to as “clinically supervised settings,” to use by individual psychiatrists treating patients directly in their homes, referred to as “clinically unsupervised settings” (
9). This development has paralleled consumers’ increasing familiarity with web-based videoconferencing platforms for social communication. The initial scientific literature on telepsychiatry focused on whether or not videoconferencing could be used for psychiatric treatments, which was answered affirmatively (
7,
10,
11). This line of inquiry is currently evolving into a more nuanced attempt to understand the inherent strengths and weaknesses of videoconferencing for patient-provider interactions.
Understanding telepsychiatry’s impact on clinical encounters is important for adaptation and modification of clinical processes to best tailor its use. Videoconferencing is currently a viable option for psychiatrists to provide care to individual patients, populations, and communities faced with limited access and to move the point of care delivery into patients’ living environments. Psychiatric providers who are new to videoconferencing should not be intimidated by the technology or its encompassing logistics, but they do need to develop an awareness of the salient regulatory, administrative, and clinical issues that may arise in the practice of videoconferencing-based telepsychiatry. This article is intended to increase knowledge of and comfort with the clinical use of videoconferencing by providing an overview of the current evidence base in telepsychiatry and reviewing administrative and clinical practices, and illustrating these points in a case example. Key issues arising in clinically supervised and unsupervised settings are addressed. The distinction between these two settings is becoming increasingly important given the current and potential growth of videoconferencing in clinically unsupervised settings, such as the provision of direct in-home psychiatric care.
Evidence Base Supporting Telepsychiatry
Although telepsychiatry has been discussed in the literature for more than half a century (
1), the majority of publications on the topic have appeared in the past two decades. Initial articles demonstrated feasibility through program and case description, and outcome research and controlled trials have been published in the past decade (
1–
7,
10). Telepsychiatry has been shown to be feasible in a wide range of settings, across a complement of psychiatric treatments, in different ethnic groups and populations, and in all age ranges, from child to geriatric psychiatry (
12). An increasing number of controlled trials are demonstrating the effectiveness and efficacy of telepsychiatry in specific treatments (e.g., anger management) as well as exploring wider benefits, such as cost savings associated with reduced travel, improved care coordination, and cost avoidance through early treatment (
1–
7,
10).
While this evidence base overall has been supportive of telepsychiatry as a clinical tool, intriguing questions have been raised about the impact of videoconferencing on clinical processes. For example, a randomized controlled trial investigating the reliability of Structured Clinical Interview for DSM-III-R diagnoses in a sample of American Indian veterans showed high reliability across diagnoses between in-person and videoconferencing assessments, although reliability was higher for externalizing disorders (i.e., outward expressions of internal states) than for internalizing disorders (i.e., moods, feelings) (
13). The study suggested that clinicians should be particularly thoughtful and vigilant in screening for these problems during initial assessments. Other programmatic and case descriptions from the literature present examples in which patients with certain diagnoses (e.g., posttraumatic stress disorder [PTSD], Asperger’s disorder) may prefer telepsychiatric over face-to-face assessments because of feelings of safety, control, and distance created in a telepsychiatric encounter (
14). Questions regarding the impact of telepsychiatry on clinical processes, therapeutic relationships, and treatment have been raised but not definitively addressed in the literature (
2).
Meanwhile, as in other fields in medicine, clinical practice and implementation of telepsychiatry have outpaced the scientific evidence. This state of affairs may leave the individual provider with questions on how best to adapt and modify clinical style/process and treatments to fit the videoconferencing encounter. Fortunately, a rich clinical experience in telepsychiatry has contributed to the development of clinical training in tele-mental health as well as clinical guidelines from multiple organizations to help educate clinicians. Two recent examples of publicly available materials include the introductory online “Telemental Health Guide” (
www.tmhguide.org; the site was developed at the University of Colorado Denver with support from the Center for Mental Health Services, Substance Abuse and Mental Health Services Administration) and the American Telemedicine Association’s “Practice Guidelines for Videoconferencing-Based Telemental Health” (
15; available at
www.americantelemed.org/i4a/pages/index.cfm?pageID=3311). These are some of several resources that provide further details related to the issues highlighted below.
Administrative Issues in Telepsychiatry
A number of unique administrative issues arise in the context of telepsychiatry, among them licensure, credentialing, malpractice, technology, and the clinical setting in which care is delivered. Videoconferencing has the potential to facilitate treatment regardless of the patient’s location, a feature that often raises jurisdictional issues of which providers need to be aware (
16,
17). With the exception of practitioners in federal health care systems (such as the Department of Veterans Affairs) and some consultations, a psychiatrist must hold a medical license in the state where the patient is located during a telepsychiatric encounter. Additional regulations in particular states may be applicable to physicians practicing telemedicine, such as the need for the presence of medical staff with the patient, written consent for the use of telemedicine, or requirements for face-to-face visits as part of telepsychiatric care. Payers (e.g., State Medicaid plans) and other licensing bodies (e.g., the Drug Enforcement Agency) may also have explicit rules that psychiatrists need to be knowledgeable of before beginning telepsychiatry.
Psychiatrists planning to begin telepsychiatry should inform their malpractice carriers of their specific involvement and make sure that there are no additional guidelines they need to follow or additional coverage they need to obtain. As in face-to-face visits, psychiatrists working within health care systems need to be appropriately credentialed in the setting where they are providing care, following the guidance of the appropriate oversight body. Generally, this requires that a psychiatrist be credentialed by each organization where the patient is located. A newer credentialing option, “privileging by proxy” for tele-health practice, has been established by the Center for Medicare and Medicaid Service; in this option, one hospital receiving tele-health services can credential a psychiatric provider by relying on the credentialing process of the hospital system in which the telepsychiatry service originates (
18). Psychiatrists providing telepsychiatric services across health care systems need to have a clear understanding of the ownership of medical records, how records are shared between systems, and provider obligations for documenting and recording.
There are a number of accepted standards for minimal technical specifications and configuration of the environment in which videoconferencing occurs. A transmission speed of 384 kilobytes per second is generally considered the minimally acceptable bandwidth in videoconferencing in psychiatry (
15). There is little guidance on the use of standard versus high-definition videoconferencing, although many advocate the use of the highest resolution available. Telepsychiatry conducted in the United States falls under the Health Insurance Portability and Accountability Act (HIPAA), which requires encryption of all electronic protected health information. Psychiatrists need to make sure that their videoconferencing system meets HIPAA requirements and is compliant with federal and state privacy requirements (
15). Psychiatrists new to videoconferencing should review recommendations for the setup of the videoconferencing system and the room—room configuration, security, lighting, angle and distance of videoconferencing equipment, types of camera controls (including remote capability), and backdrops during the videoconferencing session (
Figure 1; a more detailed description and interactive examples of room setup issues can be found at
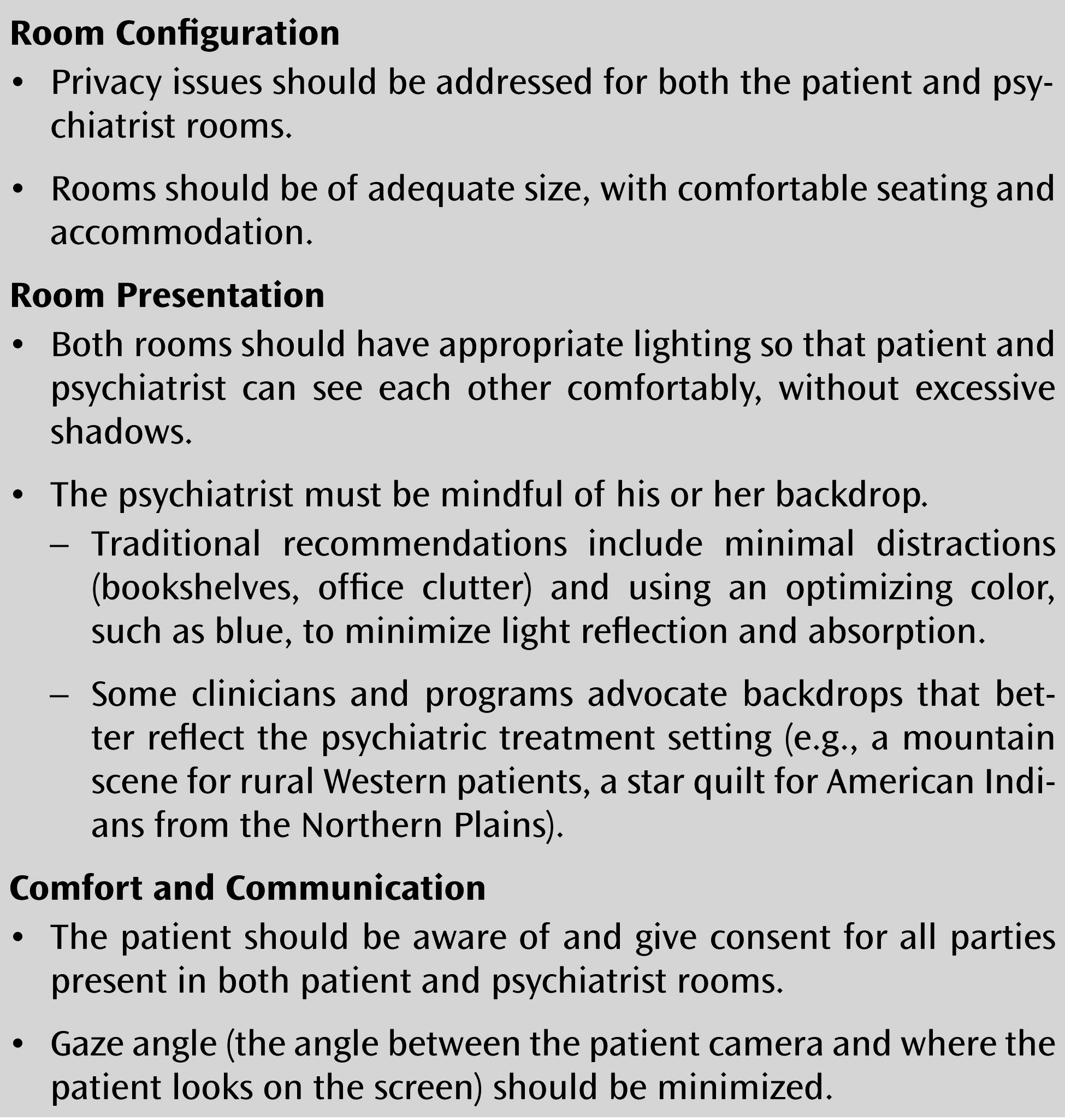
www.tmhguide.org).
Telepsychiatry services should have written protocols or procedures for the important administrative and clinical components of the telepsychiatry service. These protocols should address issues such as how patients obtain laboratory tests, schedule appointments, and receive prescriptions and how care coordination with a patient’s other medical care providers is accomplished (
15). Whether a patient is being seen in a clinically supervised or clinically unsupervised setting (
Table 1) also has an impact on the administrative handling of safety issues, environmental setup, and type of videoconferencing to be used (web-based versus standing unit) (
9). The bulk of the literature, guidelines, and clinical experience has been focused on telepsychiatry in clinically supervised settings, although there is an expanding literature describing work in clinically unsupervised settings. Guidelines on desktop videoconferencing are expected within the next year from the American Telemedicine Association.
Clinical Issues in Telepsychiatry
Psychiatry is an ideal fit with videoconferencing since, arguably, most psychiatric treatments can be translated to telepsychiatry. Telepsychiatry has no known absolute exclusion criteria or contraindications for any specific psychiatric diagnoses, treatments, or populations. Psychiatrists have wondered whether patients with ideas of reference or delusions involving technology, video, or televisions should not be treated over videoconferencing, but several case discussions (
19,
20) have documented successful telepsychiatric treatment of such cases. The key appears to be working with patients with intact reality testing and the ability to separate delusions from clinical interactions. Others have raised concerns about working with patients with cognitive impairments or sensory deficits, but these can be addressed as in face-to-face encounters through the inclusion of caregivers in sessions, as well as the use of technologies to aid with visual or auditory impairments (
21).
Before caring for any patients via videoconferencing, psychiatrists should develop an emergency protocol and procedures specific to each of the telepsychiatry services and environments in which they provide care, including local civil commitment laws and procedures. In developing these procedures, a psychiatrist will become familiar with the emergency psychiatric services available at the patient site and the processes and roles for collaborating to manage psychiatric emergencies (
22). Conceptually, telepsychiatric emergency management has many similarities to dealing with a patient calling in crisis outside of an office or clinic setting. Adhering to good psychiatric emergency management principles, regardless of the treatment modality, serves clinicians well. An issue specific to emergency management in telepsychiatry is the psychiatrist’s perception of having less clinical control because of the distance from the patient. Although there are no data or experience indicating less control in these circumstances, telepsychiatry can shatter the illusion of control afforded in face-to-face encounters, potentially increasing the psychiatrist’s anxiety while managing emergencies via videoconferencing. Providers should acknowledge this potential anxiety and actively manage it by following established protocols and procedures. Psychiatrists should also be aware that they may be able to tolerate stronger displays of affect or behavioral acting out in a telepsychiatry encounter because of the greater safety provided by not being in the room with the patient. While this may at times facilitate some clinical processes, psychiatrists need to be sensitive to any potential behavior or affect near the end of the session that could affect staff or family members present at the patient site when the session has finished (
22). Psychiatrists should make sure that both patients and staff at the point of care are familiar with emergency procedures and that staff have had appropriate training on procedures and techniques for managing emergencies.
Two other clinical issues of note in emergencies are intoxicated patients and attentiveness to firearms and other weapons. Although there are no published studies on this topic, clinical experience suggests that detecting when a patient is mildly intoxicated may be more difficult through videoconferencing than in person because of the lack of physical cues and smell. Psychiatrists should have a low threshold for inquiring about recent alcohol consumption, especially when working with patient populations at higher risk, such as those with substance use diagnoses. Those seeing patients in clinical settings should educate patient site staff to alert the psychiatrist prior to a session for any signs of possible intoxication and follow appropriate procedures for dealing with intoxication. Since many telepsychiatry services involve urban providers working with rural populations where firearm ownership rates are higher, psychiatrists providing direct telepsychiatry into a home environment also need to consider the location and availability of weapons. As clinically indicated, psychiatrists should dialogue with patients about weapons, location, availability, and firearm safety issues, especially when working with patients who report suicidal or homicidal ideation. Additionally, psychiatrists should be cognizant of the importance of firearm ownership in certain populations (e.g., rural residents, veterans), particularly when discussing weapons management in the context of treatment, and consider involving family or community members in these discussions as appropriate. Psychiatrists should address these issues in ongoing dialogue with patients rather than in a single discussion or assessment (
22).
Videoconferencing has a direct impact on communication styles and interactions. Providers using telepsychiatry need to be aware of this and appropriately adapt their clinical style and process. Psychiatrists should appreciate how they are coming across over the patient’s video display. Important components include how the psychiatrist is framed in the video display, the patient’s perception of where the psychiatrist’s eyes are looking (eye contact), and any transmission delay affecting speech flow. A general recommendation for framing of the psychiatrist in the video picture is from the midchest to 6 inches above the head, with both shoulders/arms in the picture. Psychiatrists can use framing to set the tone of a session with closer framing (a head shot) increasing the feeling of contact or emphasis and farther framing (full torso) to create more of a feeling of distance or space. An example of this would be to use closer framing when conducting a therapeutic confrontation on recent use of alcohol for a patient with a substance dependence diagnosis.
Gaze angle may be more difficult to control and is dependent on the location of the video display relative to the patient at the patient site. Even though the psychiatrist is looking directly into the video camera at the psychiatrist’s site, depending on the location of the video display at the patient site, the provider may or may not be making direct eye contact with the patient. Gaze angle should be minimized (gaze angles less than 7 degrees are hardly noticeable [
15]). Use of appropriate hand gestures and body movement can add dynamism to the presentation of the psychiatrist, but if these are excessive they can become distracting, and with lower bandwidth transmission speeds, they may cause motion artifact or blurring. Psychiatrists should utilize picture-in-picture or some other form of display during the telepsychiatry session so they are aware of what is being displayed on the patient’s display and how they are coming across.
Most videoconferencing sessions have a small (<1/4 second) but perceptible transmission delay, and delays are greater with lower transmission speeds. It is important that the psychiatrist account for this in the flow and cadence of conversation so as not to interrupt and to allow the patient enough time to answer questions. The psychiatrist should be attentive to establishing a natural conversational course, which can be facilitated by increasing or decreasing the frequency of pauses in speech.
Finally, psychiatrists may need to adapt their style for telepsychiatry, increasing their energy and expressiveness to project over video and to overcome any potential feelings of distance or remoteness that might occur as a result of videoconferencing. Small talk related to checking in about the patient’s environment and local events (e.g., weather, major news events at the patient’s location) can also help facilitate feelings of connectedness in a clinical encounter. Psychiatrists conducting group treatment via telepsychiatry may need to be more assertive with the group process to foster a stronger group dynamic and to avoid becoming a remote lecturer to the participants at the patient site. This can be assisted by being conscious of the amount of “screen time” they are taking as the group leader and by inviting specific group members to comment (
14).
Psychiatrists need to be mindful of patients’ reactions to videoconferencing. It is wise to assess patients’ previous experiences with, comfort with, and exposure to videoconferencing during the first telepsychiatric encounter. For patients with limited experience, continued education and inquiries regarding their level of comfort during the first and subsequent sessions allow identification and discussion of patients’ reservations and concerns about videoconferencing. The majority of patients, even those with limited experience, adapt quickly to the use of videoconferencing and express satisfaction and comfort with telepsychiatry.
Patients and psychiatrists may experience more of a feeling of clinical remoteness and distance, particularly in early videoconferencing encounters (
23). This perception often diminishes or disappears after a working alliance is established. In some cases this feeling can be of clinical benefit; for example, female victims of violence from male perpetrators may feel safer working with male providers via telepsychiatry and be able to discuss trauma-related symptoms more readily because of the feeling of distance and greater safety created by videoconferencing. From the psychiatrists’ perspective, a trade-off for times when they feel less engaged over videoconferencing is an increase in observing ego during sessions, with greater insight into clinical processes and reactions. Because many telepsychiatry services work across multiple systems and organizations, psychiatrists should be mindful that patients can have additional transferences onto the psychiatrist based on the organizations, locations, and systems associated with a telepsychiatry clinic. This “system transference” should be directly addressed by the psychiatrist through a clear delineation of personal and organizational roles during the education/orientation phase of the treatment (
14).
Additionally, the actual distance between patient and provider may help to facilitate feelings of confidentiality, since patients and psychiatrists may be less likely to encounter each other in a community setting, and videoconferencing into non-mental-health-affiliated locations (e.g., medical clinics, offices, homes) allows patients to receive psychiatric care without the potential stigma of visiting a mental health facility.
At the first meeting via telepsychiatry with a patient, prior to beginning the assessment, the psychiatrist should conduct a telepsychiatric orientation and consent process. This should involve the psychiatrist introducing him- or herself and identifying his or her location, organization, and certification. All parties present at both the patient’s and the psychiatrist’s sites should be introduced, and the psychiatrist should pan the camera around the room he or she is using so the patient can see who is present and be familiar with the psychiatrist’s room setup. The psychiatrist then assesses a patient’s past experience and knowledge of videoconferencing and provides information about the videoconferencing technical setup (video display, security). The psychiatrist should explain the organizations and staff involved in the clinic, emergency procedures for the clinic, the limits of confidentiality, how to interact and contact the psychiatrist outside of the clinic, and other logistical issues (laboratory tests, prescriptions). A review of the benefits and risks of telepsychiatry and alternatives (if any) should be conducted. At the end of this orientation, the psychiatrist should ask if the patient has any questions about these issues before beginning a clinical interview. A video sample that provides a brief overview of many of these elements is available at [
http://www.youtube.com/watch?v=zWBJDj9owv0&feature=youtu.be]. The psychiatrist should monitor the patient’s level of comfort during the session, and at the conclusion ask how the patient felt about using videoconferencing.
The coming decade will see continued expansion and integration of videoconferencing in routine psychiatric practice. A growing body of evidence, information, and training is available for psychiatrists interested in adopting telepsychiatry into their clinical practices. Many psychiatric residency programs are beginning to develop and offer telepsychiatry training as part of psychiatric education (
4,
24). These efforts and resources aid in the integration of videoconferencing as a routine component of psychiatric care benefiting patients through increased access to needed treatment.