Clinicians and researchers have long recognized that the negative symptoms of schizophrenia are a major contributor to the disability associated with the illness (
1,
2), typically persist even when the positive symptoms of the illness remit (
1), and are not well treated by either conventional or atypical antipsychotics (
3). The negative symptoms of schizophrenia include constructs such as asociality (disengagement from others), avolition (reduced initiation or persistence in goal-directed behavior), anhedonia (a putative reduction in the ability to experience pleasure), alogia (a reduction in speech output), and blunted or flat affect (a reduction in the display of affect in facial expressions, voice prosody, and gesture). Clinicians and researchers have had access to a number of instruments for rating the severity of negative symptoms for many years, and the availability of these seminal rating scales has played a major role in helping to alert the psychiatric community to the critical importance of these symptoms (
2). The article by Kring et al. in this issue (
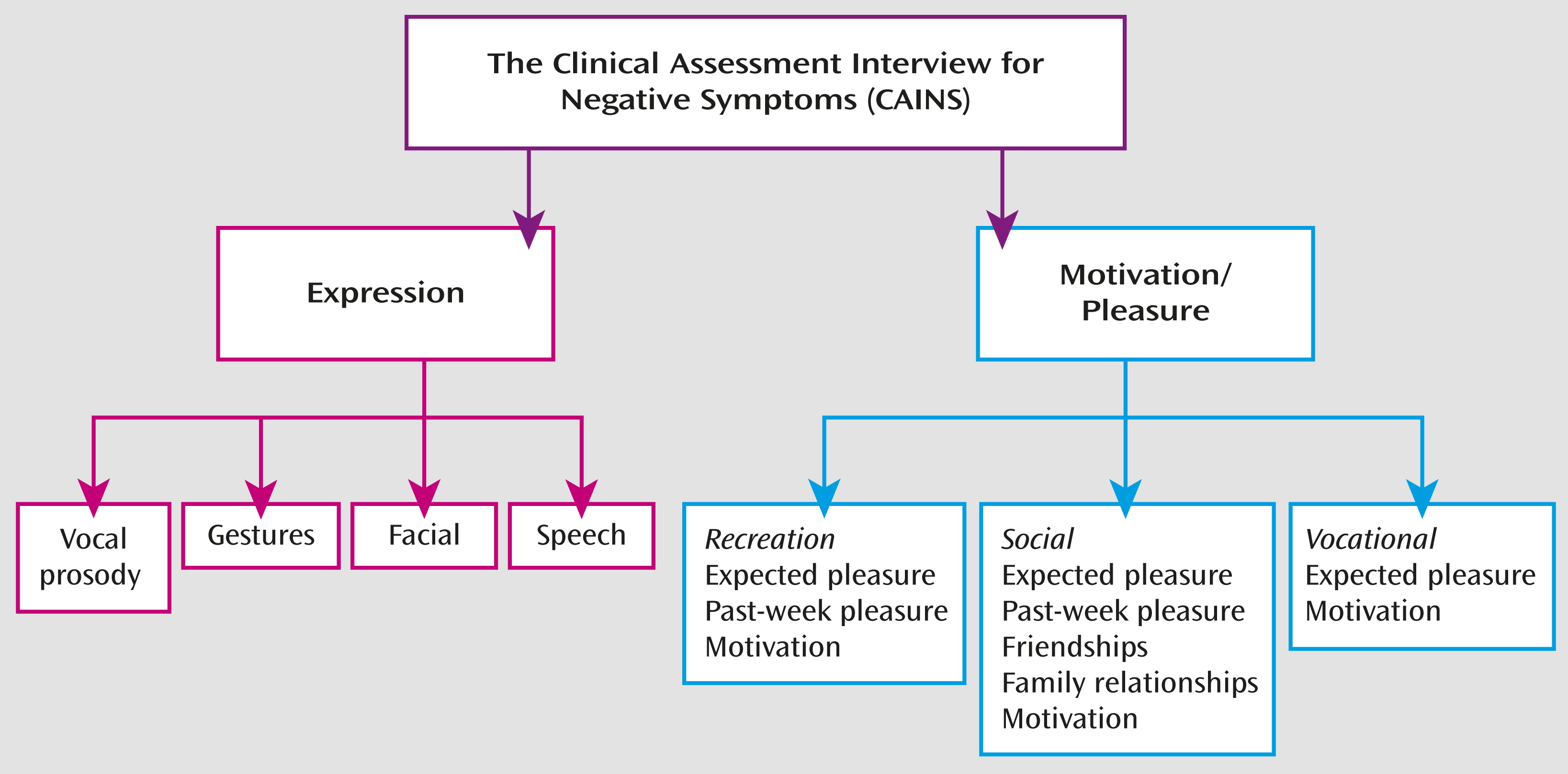
4) introduces a new scale, the Clinical Assessment Interview for Negative Symptoms (CAINS), which represents an important and novel addition to the tools available for assessing negative symptoms in schizophrenia and other psychotic disorders.
There are both theoretical and practical reasons why the CAINS represents a critical advance for our field. At the theoretical level, the constructs assessed by the CAINS and the approach to definition and evaluation take advantage of the major advances made in the past 30 years in affective science and neuroscience. The CAINS assesses domains that map both to the phenomenology of schizophrenia and to constructs that have been validated by neurobiological and psychological research on emotion, motivation, and affect processing. This is of critical importance, as it allows clinicians and researchers to draw on the wealth of human and animal neuroscience research that can inform our understanding of both mechanisms and potential novel pathways for treatment. One concrete example is the novel distinction the CAINS makes between anticipatory components of pleasure and motivation on the one hand and the experience or consummation of pleasurable activities on the other. This distinction reflects a large body of neuroscience research suggesting that anticipation or prediction of rewards depends on intact dopamine function, particularly the projections to the ventral and dorsal striatum (
5,
6), while hedonic experiences in the moment may be mediated more by activation of the opioid and GABA-ergic systems in the nucleus accumbens shell and its projections to the ventral pallidum, as well as in the orbitofrontal cortex (
6). The use of instruments such as the CAINS will help us integrate modern affective neuroscience into our understanding and assessment of psychiatric disorders such as schizophrenia. The development of the CAINS also included establishing its relationship to real-world function, although other measures of negative symptoms also show relationships to real-world functioning.
There are also a number of important practical issues that make the CAINS an important addition to the field. First, the CAINS provides much broader coverage of negative symptoms than some of the commonly used instruments, such as the Brief Psychiatric Rating Scale (BPRS) (
7) and the Positive and Negative Syndrome Scale (PANSS) (
8). The expanded BPRS includes only self-neglect, blunted affect, and emotional withdrawal as items that assess negative symptoms, and the PANSS has little coverage of motivational or hedonic impairments outside the social domain. The Scale for the Assessment of Negative Symptoms does cover the same major domains as the CAINS (
2), but it does not make the same distinctions between anticipation and experience in the social, recreational, work, and educational domains. The CAINS was also developed using the largest standardization samples of any scale developed for the assessment of symptoms in schizophrenia, and it used participants analogous to those who would be recruited for typical treatment trials. The CAINS has excellent psychometric properties that provide it with good power and sensitivity for detecting both individual differences in symptom severity across individuals and for detection change over time. It also has the advantage of having structured probes and questions that help ensure that different clinicians and researchers will use the scale in the same way in different settings. Given that good reliability has a major impact on the ability to see changes in symptom severity as a function of treatment, this is an important advance for treatment trials. Standardized training videos are also available for helping train clinicians and raters on the use of the instrument, which few other rating scales have; such training materials will be very helpful for individuals who want to incorporate use of the CAINS into their clinical practice or research. The CAINS has already been translated into Mandarin, Cantonese, and French, allowing it to be used in international trials. The Brief Negative Symptom Scale (
9) also makes the important distinction between expected and experienced pleasure and includes structured probes. However, its test-retest reliability has been assessed only in relatively small samples of individuals with schizophrenia to date (
9,
10).
The CAINS also has some potential limitations that should be noted. First, the instrument is somewhat long, which may limit the ability of some clinicians to incorporate it into their practices. This is a drawback common to most structured instruments assessing positive or negative symptoms in psychosis, and it is rooted in the very real constraints on time in the clinical practice setting. Second, the analyses of the CAINS data suggest that there are actually two major dimensions to negative symptoms, one reflecting the expression of emotion and the other reflecting “motivation and/or pleasure” (
Figure 1). Ideally, clinical trials focusing on the treatment of negative symptoms would assess these two endpoints separately, as they may reflect dissociable etiological mechanisms and thus may respond differentially to treatments. However, the use of more than one endpoint is frequently avoided in clinical trials because of concerns about statistical power. The CAINS can be used with a single endpoint that reflects combined negative symptom severity across both these domains.
Despite these potential limitations, the advances provided by both the theoretical and psychometric development of the CAINS make it an important advance in our field. The development of instruments like the CAINS, motivated by findings from affective neuroscience, allow our field to stay abreast of advances in the basic sciences and pave the way for a more rationally informed approach to treatment development, hopefully leading to more effective treatments for the debilitating negative symptoms of schizophrenia.