The Editors are pleased to offer personal selections of some of the articles they found particularly interesting and important in this year’s Journal.
Mental Illness in Hotel Residents
“The Hotel Study: Multimorbidity in a Community Sample Living in Marginal Housing” by Vila-Rodriguez and colleagues is published in this issue (
1). The study is a survey of 293 men and women who were living alone in substandard hotels in poor Vancouver neighborhoods. Over half these people were psychotic and half had neurological illnesses, often traumatic brain injury. Over 95% abused substances. They are forgotten people, often homeless, who rarely come to medical attention until they die. The article’s senior author is William Honer, chair of the University of Vancouver Department of Psychiatry. His department, the Canadian health funding agencies, and the Portland Hotel Society are to be commended for reaching out to hotel residents. When I was in high school, my family owned such a hotel in St. Louis and I worked there. Indeed, alcoholism, brain injury, psychosis, and social isolation afflicted these tenants. Our mother told us their stories and taught us to treat them with the respect that their previous lives deserved, not with disdain over their afflicted condition. December was difficult. We put up a tree in the lobby, which everyone admired, but as the holiday week came closer, sadness overcame them. Our attorney, one of the most prominent in the city in his day, drank more heavily. His law firm could not stop him from drinking, but in a month they would detoxify him once again because the judge demanded his appearance in a pending litigation. They would drop him at our hotel after the hearing, still dressed in a new three-piece suit, and he would pawn his clothing to resume drinking. One morning we found him singing with several similar men, downcast and drunk, but still using the remnants they remembered of holiday songs to cheer themselves. I could not comprehend then his life or his illness, and after a career in psychiatry I am not sure that I have come any closer. But I understand that there are lessons to be learned from such lives.
Paternal Age and Psychiatric Disorders
I read The American Journal of Psychiatry, as I suspect most do, paying close attention to articles touching areas relevant to my own work or special interests and then skimming the others, reading abstracts, and exploring further those with clinical relevance or intellectual or scientific interest.
The review of “selfish spermatogonial selection” by Goriely et al. (
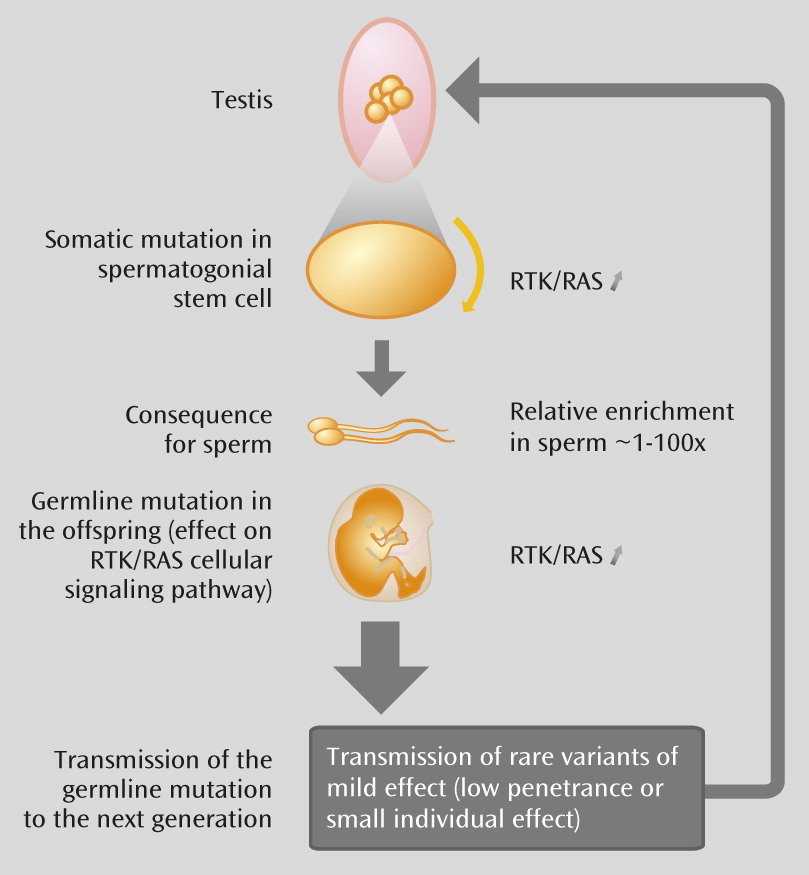
3), published in June 2013, is among the latter group. It continues and extends an important and fascinating scientific story that started with the observation that advancing paternal age correlates with an increase in several psychiatric disorders, including schizophrenia and autism, as well as several rare Mendelian dominant disorders.
This appears to be linked to an important difference in the sexual biology of men and women. Female germ cells have 22 mitotic cell divisions before maturation and meiosis into eggs; male germ cells have a mitotic division every 16 days from puberty until maturation (approximately 840 by age 50) and meiosis into sperm. As a result, mitotic copy errors are associated with paternal genes; 80% of de novo mutations are paternal in origin.
However, the story goes further. Mutations are random events occurring over time and most often result in no effect or perhaps inactivation of the affected genes, but occasionally one enhances the function of the gene or the protein it makes. Such rare mutations in certain metabolic pathways then provide “a selective advantage to the mutant spermatogonial cells in which they arose.” This means that not only will older men have more such mutations in their sperm, but rare precursor cells with such mutations will have a competitive advantage compared with sperm precursor cells without the mutation, and their sperm will become more abundant.
There are further fascinating extensions of this model. Not only older fathers, but older maternal grandfathers are risk factors. The competitive advantage of the mutated cells in the testes that enhances their proliferation appears to be related to the biology of both cancer and mental illnesses. Finally, since there is currently a trend toward later paternal age in many societies, and some of these mutations tend to accumulate over generations, we may be entering an era of increasing genetic risk for some major neuropsychiatric disorders.
Childhood Separation and Adult Panic
A key developmental principle suggests that one set of behaviors in a child can provide a foundation for a different set of behaviors in an adolescent or an adult, much in the way that the behaviors of the tadpole prepare the organism for life as a frog. It has been difficult to find clear illustrations of this principle in research on psychopathology. Kossowsky and colleagues (
4) reviewed the state of research on one of the few such examples where a wealth of rigorous, longitudinal research exists. This concerns the relationship between childhood separation anxiety disorder and various adult outcomes, particularly panic disorder.
Kossowsky and colleagues summarized data from nearly 15,000 subjects, examining the nature of longitudinal associations between separation anxiety disorder and later psychopathology. As with many individual longitudinal studies, the findings generate both interesting conclusions and questions. Overall, in terms of the most interesting points, the analysis documents an increased risk for a range of anxiety states, including panic disorder, among adults who suffered from separation anxiety disorder as children. This emphasizes the need to understand processes that sustain anxiety across development. In terms of questions, only modest evidence of specificity emerged, and this generates interest in understanding the causes of differential outcomes. While separation anxiety disorder did not strongly predict later major depressive disorder, it was associated with a range of anxiety disorders extending beyond panic disorder, the adult condition most typically examined in tests of the so-called “separation anxiety disorder hypothesis.”
Relapse Duration Is Aversive to the Schizophrenia Brain
Clear thinking about the causes and moderators of disease biomarkers in serious mental illness is not only critical but also possible in modern psychiatric research as long as strong tools are available and incorporated into research designs. In “Relapse Duration, Treatment Intensity, and Brain Tissue Loss in Schizophrenia: A Prospective Longitudinal MRI Study” (
6), Andreasen and colleagues logically considered the determinants of progressive brain volume loss as a biomarker of disease in schizophrenia and used a repeated-measures linear model to test multiple determinants of progressive brain volume loss, focusing in this study on three: antipsychotic medication, relapse number, and relapse duration. Moreover, they used the Iowa Longitudinal Study cohort, a meticulously collected data set of biomarkers and long-term outcome in a large patient cohort, to query the effects of these three determinants in progressive brain volume loss. This article reveals clinically relevant facts as well as important research outcomes: of the 202 patients, 157 (77.7%) relapsed at least once during the multiyear study, while 29 (14.4%) did not relapse and 16 (7.9%) remained so actively psychotic that relapse was not possible; and over the disease course, relapses were more frequent but relatively short in early illness, while in the late illness phase, relapse number went down but duration increased for some patients. Andreasen et al. found that
relapse duration was the strongest determinant of brain volume loss over time, although relapse number contributed weakly. And it was the frontal lobe and the white matter that suffered the greatest volume loss with relapse duration. Antipsychotic medication contributed modestly to the progressive volume loss, but this effect was distributed across brain regions and not focused predominantly on the frontal lobe. These observations will serve to focus mechanistic research on the volume-vulnerability elements of acute psychotic relapse (i.e., what is it about ongoing psychosis during relapse that could generate tissue volume loss with time) and the specific regional vulnerability of the frontal lobe to these elements. From a clinical perspective, these results emphasize the importance of minimizing relapse duration in schizophrenia.