Across follow-up studies of first-episode patients, a complex pattern of structural alterations has been described over the course of illness, with frontotemporal cortex abnormalities being most consistently observed (
4,
7,
8). However, follow-up studies of first-episode patients are restricted to the early illness course for the foreseeable future because of the decades required to track lifespan effects. Further, these longitudinal studies are all conducted with patients treated with antipsychotic medications, which may adversely impact brain anatomy and confound tests for disease effects over the illness course (
3). Therefore, questions about how different brain regions may be altered over the longer-term course of schizophrenia and the degree to which identified changes represent treatment or illness effects remain unresolved.
In this circumstance, cross-sectional studies that examine structural abnormalities in relation to age or disease duration in chronically ill patients never treated with antipsychotic medication may provide important insights about longer-term changes in brain anatomy over the illness course (
9,
10), without the confounding influences of antipsychotic and other psychiatric medications (
11–
13) or other secondary factors (
14). This could help determine the degree to which progressive effects seen in childhood-onset schizophrenia (
15) are also seen following illness onset in more typical patients, with onset in early adulthood, and whether such changes are seen in specific brain regions in patients never exposed to antipsychotic medications.
In the present study, we conducted MRI studies of never-medicated chronic schizophrenia patients with illness durations ranging from 5 to 47 years. We sought first to identify brain regions where cortical thickness or gray matter volume differed from that of matched comparison subjects, and we then determined whether within those regions there were group differences in age-related abnormalities in brain anatomy. Primary analyses were performed with the cortical thickness data; key findings from brain volume analyses are summarized in this article, with the full analyses presented in the data supplement that accompanies on the online version of the article.
Method
Participants
The study included 25 chronically ill, never-medicated schizophrenia patients. Most patients were identified from the Mental Health Screening Program supported by West China Hospital, a project aiming to provide psychiatric care to people living in the community who have serious mental illness but who have not had access to or previously sought psychiatric treatment. When a suitable individual was identified from local medical or police records, a psychiatrist from the program visited the person’s home, accompanied by a psychiatrist from our research team. Nearly 90% of identified individuals agreed to participate in this imaging study. All were living with their families, as is common in west China, and family members provided history information. Clinical diagnostic evaluations were conducted by the research team to confirm clinical diagnoses with the Structured Interview for DSM-IV Axis I Disorders (SCID). If the diagnosis of schizophrenia was confirmed, affected individuals were brought to our MRI facility for scans, after which the majority began treatment.
These patients, 18 in their 40s or older, were recruited from within approximately 35 km of downtown Chengdu in west China. The mean duration of illness was 21 years. Patients were all of Han ancestry. Fifteen lived in rural areas, mostly in small villages 10 km away from Chengdu with tight social networks; the others were living in urban or suburban areas. The onsets of symptoms were gradual and insidious for 16 of the patients, while the other nine developed acute psychosis after some significant life trauma, such as the loss of a close relative, parental marital difficulties, or infidelity by the patient’s spouse. Before the study, 14 of them had not been involved in any type of employment and had not contributed any significant physical work in their home or community, and 11 were able to care for themselves in many activities of daily living. The families of 23 patients had regular incomes, even though some were relatively low, and two patients and their families were living primarily with support from the government. The family members worked mainly as manual laborers and farmers, and their education levels were not high. Most of the patients and their family members had 9 years of typical education, including 6 years in primary school and 3 years in junior high school, as is most common in China. All of the patients had been well taken care of by their families since the onset of their illness.
These patients had not received any prior treatment with psychiatric medications for various reasons, primarily because of 1) parental concern about family stigma associated with mental illness (prominent in 11 cases), 2) a lack of understanding or recognition of the severity of mental illness in a child or spouse (noteworthy in seven cases), 3) poor socioeconomic conditions that limited travel and funds for medical care (four cases), and 4) emotional rejection of medical care by the family due to conflicts with physicians when the patient was first brought to medical attention close to the time of illness onset (three cases). As a result of these factors, each patient had been cared for and sheltered in the parents’ home without medical care through the course of the illness. While not common practice now, in the years during and immediately following the Cultural Revolution, many patients with serious mental illness did not receive psychiatric care for similar reasons.
Duration of untreated illness was evaluated by the Nottingham Onset Schedule (
18) (with information provided by the patients, other family members, and other sources). Psychopathology ratings were obtained by using the Positive and Negative Syndrome Scale (PANSS) (
19), and they included total scores as well as factor scores derived by using the previously published six-factor structure pattern of PANSS items (
20).
Healthy comparison subjects (N=33) were recruited through poster advertisements; they were from the same geographical region as the patients and had similar socioeconomic and educational backgrounds. The nonpatient edition of the SCID was used to establish the lifetime absence of psychiatric illness, and there was no known history of major psychiatric illness in their first-degree relatives. The patients and comparison subjects were matched in age, sex, and years of education (
Table 1). Age distributions for male and female subjects did not differ across subject groups.
No participants had a history of significant systemic or neurological illness. All were right-handed as assessed with the Annett Handedness Scale (
21). The following exclusion criteria applied to both groups: 1) age younger than 18 years or older than 80 years, 2) history of substance abuse, 3) pregnancy, and 4) major physical illness, such as cardiovascular disease or hepatitis, as assessed by clinical evaluations and medical records. The ethics committee of Sichuan University approved the study, and all participants gave written informed consent to their participation.
Data Acquisition
MRI examinations were performed on a 3-T GE Signa EXCITE scanner (General Electric, Milwaukee, Wis.) with an eight-channel phase array head coil. High-resolution T1-weighted images were acquired with a volumetric three-dimensional spoiled gradient recall (SPGR) sequence (repetition time=8.5 ms, echo time=3.4 ms, flip angle=12°). A field of view of 240×240 mm2 was used with an acquisition matrix comprising 256 readings of 128 phase-encoding steps, producing 156 contiguous 1.0-mm coronal slices. The final matrix of T1-weighted images was automatically interpolated in plane to 512×512, yielding an in-plane resolution of 0.47×0.47 mm2. T1- and T2-weighted magnetic resonance (MR) images were inspected by an experienced neuroradiologist; no scan artifacts or gross brain abnormalities were observed in any participant.
Imaging Processing
Cortical modeling and volumetric segmentation of structural MRI data were performed with the FreeSurfer package (version 5.1.0,
http://surfer.nmr.mgh.harvard.edu/). Cortical thickness was measured as the difference between equivalent vertices in the pial and gray/white matter surfaces (
22), by using both intensity and continuity information from the entire three-dimensional MR volume in segmentation and deformation procedures. The reliability of the method has been validated against histological analysis on postmortem brains (
23) and manual measurements (
24), and test-retest reliability is high (
25). Briefly, the main process included automated registration to Talairach space, segmentation of the subcortical white matter and gray matter volumetric structures, intensity normalization, tessellation of gray matter and white matter boundaries, and automated topology correction and surface deformation following intensity gradients to optimally place the gray/white and gray/CSF borders defined at the location with the greatest shift in signal intensity (
22,
26–
30). The surface maps, following registration of all subjects’ cortical reconstructions to a common average surface, were analyzed after the interpolation steps, and they are thus capable of detecting submillimeter differences between groups (
22). Since the surface-based analysis was restricted to the cortical mantle, we used volumetric analysis to assess deep gray matter by means of diffeomorphic anatomical registration using the exponentiated lie algebra (DARTEL) toolbox (
31). Details of the standard analysis procedures are presented in the
online data supplement. Postprocessing visual inspection for quality of both imaging processes was conducted without knowledge of subject characteristics.
Statistical Analysis
In the graphical interface of FreeSurfer known as QDEC (Query, Design, Estimate, Contrast), a smoothing step with 10 mm full width at half maximum was initiated to average the cortical thickness data across participants in the common spherical coordinate system. Then vertex-by-vertex cortical maps of the patients and comparison subjects were compared by using a general linear model with age, sex, and total intracranial volume included as covariates. Nonparametric cluster-wise correction for multiple comparisons was performed by means of the FreeSurfer Monte Carlo simulation tool with a corrected cluster-forming threshold of p<0.05 (
32).
To identify differential relationships between anatomical measures and age in regions where group differences were detected, we first extracted and averaged values of cortical thickness and gray matter volume in regions with significant group differences for each subject. Aging effects on the human brain are believed to follow a nonlinear trajectory in schizophrenia patients (
15,
33), as in healthy individuals (
34). Therefore, nonlinear regression analyses using a quadratic model of age effects in relation to anatomic measures were conducted for each group. Age-related trajectories of brain changes have been modeled with this approach as it is straightforward and flexible for accommodating different nonlinear effects (
34–
36). These models were compared across groups to determine whether there was a significant differential rate of age-related change in patients and comparison subjects. This was achieved by conducting F tests to determine whether the shapes of regression curves were significantly different (
37). A “leave-one-out” cross-validation approach was adopted to identify potential high-impact cases in modeling of age effects and group differences in aging effects; in all cases, the significant effects reported below were confirmed. The effect of duration of illness was examined with the same modeling approach in patients. Partial correlations controlling for age and sex were determined for associations between structural brain measurements and clinical symptom severity ratings at the time of the scans, as determined by PANSS total score, subscales, and factor scores.
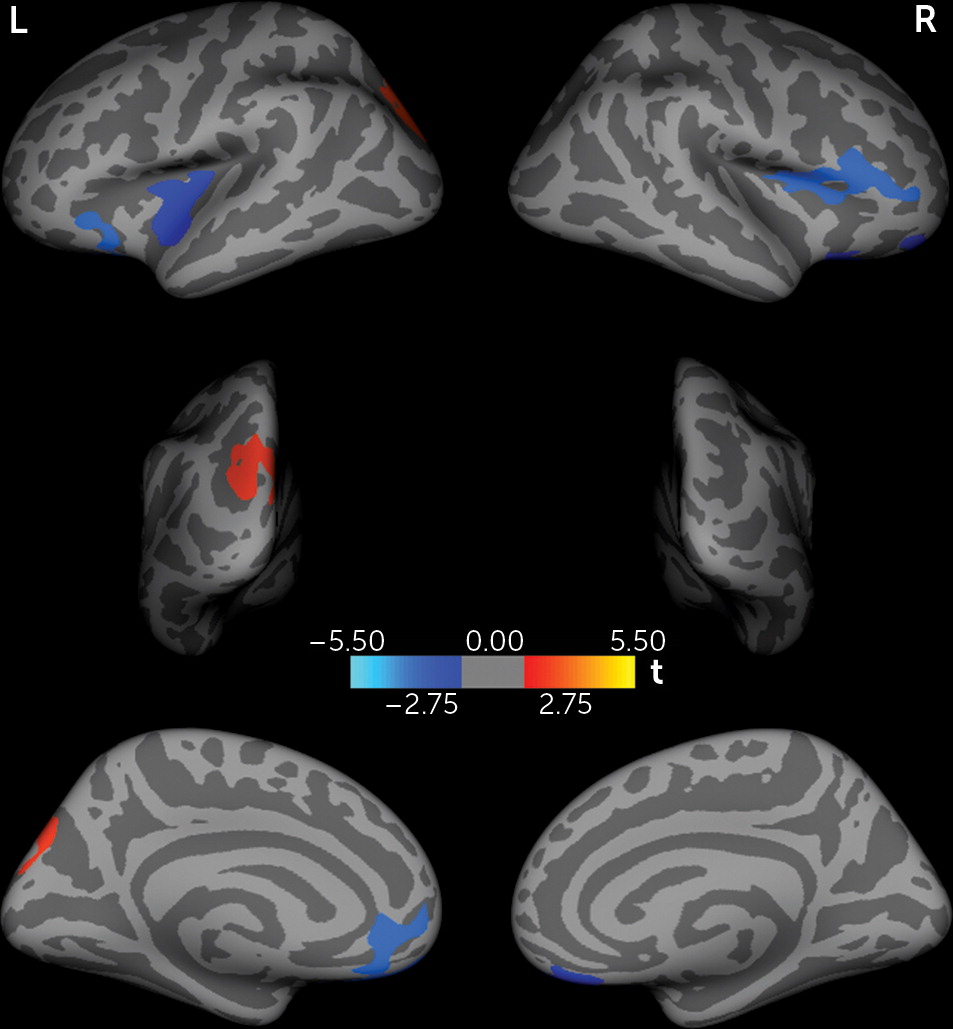
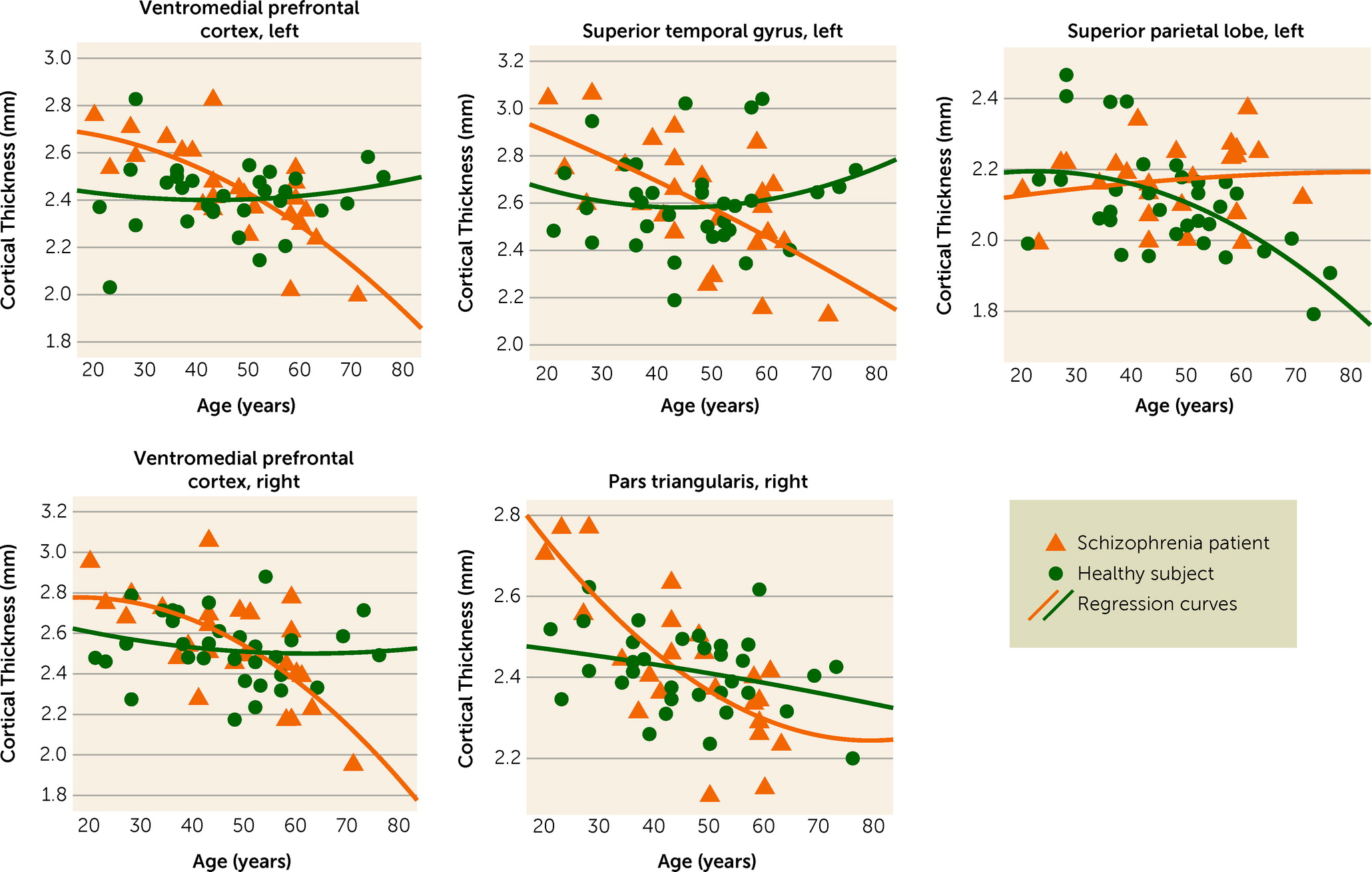
Discussion
By studying this relatively unique sample of chronically ill but never-medicated schizophrenia patients, the current study adds important new evidence about gray matter changes over the course of schizophrenia without the potential confounding influences of antipsychotic treatment. Surface-based analysis demonstrated cortical abnormalities in schizophrenia patients involving prefrontal, temporal, and parietal lobe regions. More important, age-related effects suggest a more rapid rate of cortical thinning in the right ventromedial prefrontal cortex, right pars triangularis, and left superior temporal gyrus in patients than in healthy comparison subjects, whereas age-related changes in the posterior superior parietal lobe appeared to be less rapid than in the healthy subjects. Volumetric analysis demonstrated significant abnormalities in cortical and subcortical gray matter, notably including greater bilateral putamen volume in patients, but these effects did not have differential aging effects in the schizophrenia patients. Thus, the most important finding of our study is that age-related changes in cortical thickness suggestive of a neuroprogressive process in schizophrenia were found in the prefrontal and temporal cortices, while abnormalities in other areas, including the putamen and parietal cortex, did not show accelerated age-related changes, suggesting different pathological or compensatory processes. These results reinforce the notion that schizophrenia may involve neuroprogressive changes in specific brain regions over the course of the disease, potentially resulting from neuropathologic mechanisms, including the previously reported shrinkage of neuropil, reduced neuron size, and cell loss (
38–
40).
Previous longitudinal studies with 10-year follow-up of treated patients have shown that the lateral ventricles exhibited increased enlargement over the course of illness (
41,
42), suggesting atrophic changes over time. The current study of chronically ill but never-treated schizophrenia patients is consistent with this observation and extends it in two important ways. First, our findings suggest that this pattern may continue in some brain regions later in life. In fact, our modeling of age-related changes in cortical thickness suggests that neuroprogressive mechanisms may begin slowly in the early phase of the illness and become more prominent later in the course of illness in specific brain regions. This may account for why we and others have not identified progressive changes early in the illness course (
43–
45). However, the degree to which these changes represent a direct pathophysiological consequence of the disease or a secondary factor, such as long-term disengagement from social relations and other life activities, remains to be determined. Second, our findings suggest that changes over the course of illness are not secondary to antipsychotic treatment. Whether other regions might also show similar effects in addition to those identified is possible, as we may have lacked statistical power to detect less robust effects.
The accelerated reduction in cortical thickness in the frontal cortex in patients supports the view that frontal cortex abnormalities are an important component in schizophrenia-related morbidity, and it suggests that the identified frontal lobe regions may be more vulnerable to the long-term effects of the illness (
3,
4,
46,
47). Previously, medial prefrontal cortex pathology has been identified in multimodal imaging studies (
48), and volume loss in the ventromedial prefrontal cortex in schizophrenia has been associated with deficits in the theory of mind skills needed for social relationships (
49). Prolonged social isolation might contribute to progressive gray matter loss in this region, as suggested by animal models (
50).
Another frontal region exhibited age-related reductions in cortical thickness, the pars triangularis. This lateral-posterior part of the inferior frontal gyrus has been observed to manifest cortical thinning in untreated first-episode patients (
45). While volume reduction of this region has been suggested to represent a risk factor for schizophrenia (
51), the neuroprogressive changes in this region may represent a neurobiological underpinning of the early clinical changes associated with the prodrome period preceding onset of psychosis. Given the importance of this region for speech and language processing, there may be a broader clinical significance to changes in this region.
The superior temporal gyrus was also found to show progressive changes in our study, consistent with studies of early illness course in which progressive cortical alterations manifested their greatest severity in the frontal and temporal lobes (
5,
52). Cortical thinning in the left superior temporal gyrus was observed in a previous study with untreated chronically ill patients (
16). Temporal volume change has emerged as a promising predictor of treatment response, as gray matter loss in this region has been found in treatment-resistant schizophrenia (
53). Thus, progressive changes in this region might contribute to higher rates of poor outcome reported for patients with chronic schizophrenia than for first-episode patients (
5).
In individuals at high risk for psychosis, as in first-episode patients, cortical thinning and gray matter reduction of the superior temporal gyrus have been shown to progressively worsen over time (
7,
54,
55). The observed cortical thinning of the superior temporal gyrus appears to be a familial trait linked to schizophrenia (
56) that begins at or before illness onset and worsens over the course of illness. It also should be noted that such progressive effects seen in the frontal and temporal cortices have also been observed in childhood-onset schizophrenia, though the progressive volume loss in those patients seems to occur at a faster rate than is suggested by our data (
57,
58).
In contrast to findings of accelerated age-related cortical thinning in some brain regions, we observed a lower rate of decline in cortical thickness with age in the left superior parietal lobe in patients. Gray matter reduction and cortical thinning of the superior parietal lobe have been reported in previous MRI studies with first-episode or early-course patients (
59,
60). However, in the meta-analysis by Olabi et al. (
3), no progressive decline in patients was seen in parietal gray matter. In addition, increased cortical thickness in the parietal cortex of treated patients with chronic schizophrenia was reported previously in another study (
5). Without the confounds of medication, our findings suggest that changes over the course of illness in the parietal cortex are different from those seen in the frontal and temporal cortices. This might represent either a compensatory response related to increased use of the parietal cortex to support perceptual or other processes or a different pathological process, such as insufficient synaptic pruning with distinct anatomic and functional consequences (
61). As our observation of reduced age-related effects in the parietal cortex is relatively novel, more work is needed to confirm the effect and investigate its causes and clinical implications.
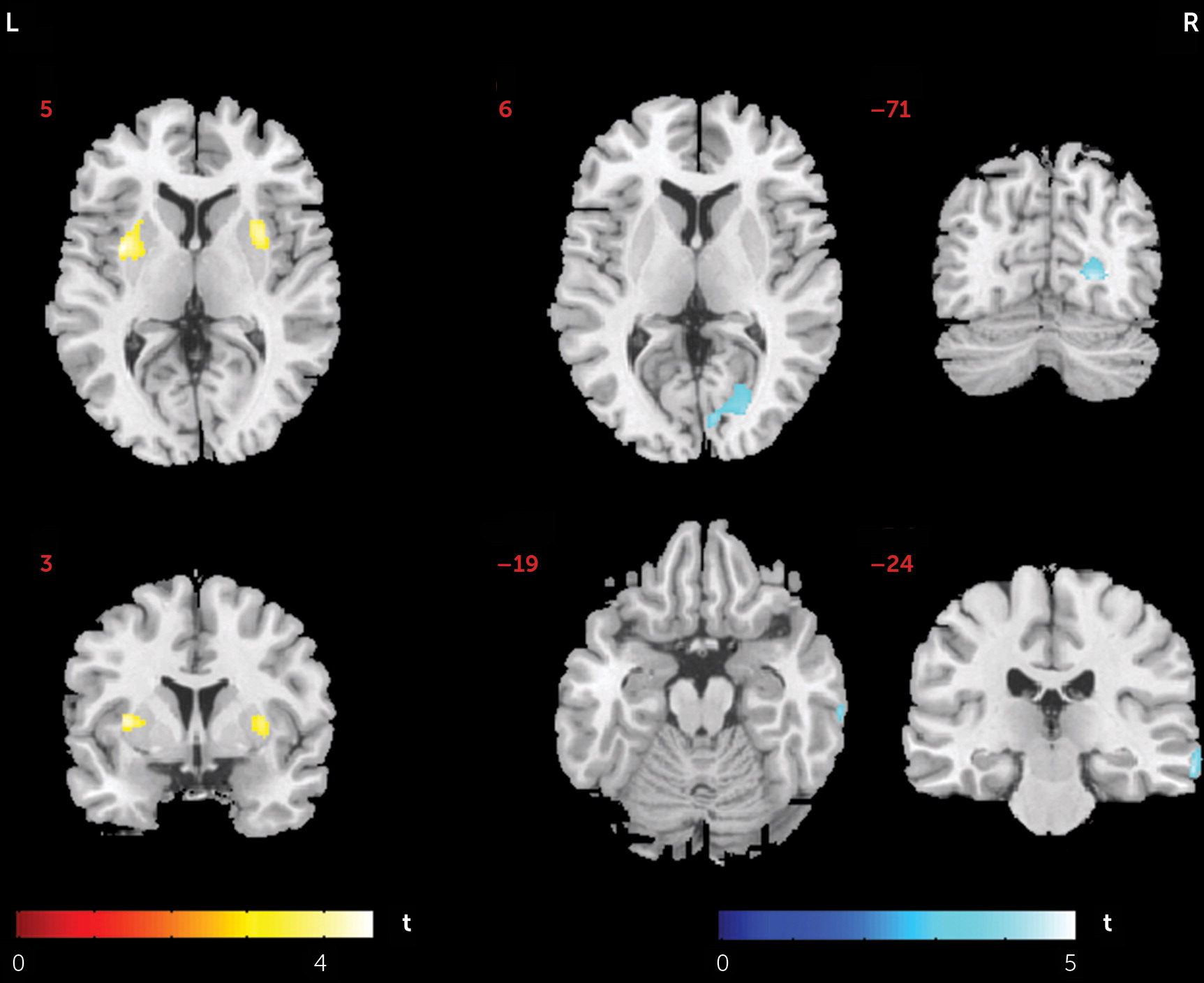
Another finding from our study was the larger bilateral putamen seen in the volumetric analysis. This effect has in the past been attributed to antipsychotic medication (
11,
12,
62), so our study adds important new knowledge by showing that illness-related processes can also induce hypertrophic striatal changes independent of effects of antipsychotic treatment. In our previous study of drug-naive first episode patients, we observed increased spontaneous neural activity in the putamen bilaterally by means of resting-state fMRI (
44), a finding similar to earlier observations of increased striatal metabolic rates in untreated schizophrenia patients (
63). As the dorsal striatum is rich in dopamine, it is intriguing to speculate that an abnormality in dopaminergic systems targeted by antipsychotic medication, or other factors related to increased striatal neural activity, might be a relevant pathophysiological process underlying these striatal changes (
64,
65). Given that striatal volume has been shown to be low in first-episode patients (
66) and that volume enlargement was not associated with age or illness duration effects in this region, it appears most likely that high neural and metabolic activity in the striatum after illness onset may increase striatal volumes early in the course of illness and then not progress appreciably after that time.
Several limitations in our study are important to recognize. First, the cross-sectional nature of our study limits any strong inference about age-related trajectories of brain changes. While we could not identify clinical or demographic factors related to illness duration that might artifactually induce differences from the comparison subjects in age-related effects, an unidentified factor related to patient age, rather than aging itself, might bias our findings. This limitation of our study design needs to be considered in balance with the impossibility of conducting prospective longitudinal studies of untreated patients. In this context, our study of a relatively large sample of never-treated patients with chronic schizophrenia who have a wide range of illness duration provides an important and novel approach for studying brain changes over the course of illness. The approach has two main advantages: it provides a window into later-course illness effects that will not be available from longitudinal studies for many years, and it avoids medication confounds that complicate interpretation of all ongoing longitudinal studies.
There are other limitations to be considered as well. First, while our sample of never-treated chronically ill patients was larger than those in previous studies, it was not large for precisely modeling age-related effects. In particular, the degree to which the age-related changes progress gradually or are prominent early or late is difficult to determine. Examination of the modeled age effects for different brain regions in
Figure 2 provides somewhat conflicting clues in this regard. While the models of the regions of interest tend to cross around age 50 (with the patient data showing atrophic changes relative to the healthy subjects only after that point), the rate of change in the modeled age effects seems to increase not long after illness onset. Research with larger samples is needed to model age effects and the rate of change more precisely so this issue can be addressed. Second, our study design did not include a parallel matched group of chronically ill treated schizophrenia patients with comparable disease duration and demographic characteristics. Last, some age-related effects were not seen in regions where they might be expected, especially in the comparison subjects. This may be due to our sample size but perhaps more likely to the fact that the individuals in our sample were mostly under the age of 60 years, when atrophic age-related changes are notably less prominent than in elderly individuals.
In conclusion, by studying a rare sample of never-medicated chronically ill schizophrenia patients with a wide range of illness duration, we found a faster rate of prefrontal and temporal cortical thinning and striatal hypertrophy, which may represent core components of the pathophysiological process of schizophrenia over the course of illness, effects that could not be attributed to antipsychotic treatment. These findings may provide important insights into the course and regional specificity of progressive brain changes associated with schizophrenia in the decades after illness onset.