A growing body of evidence has linked insomnia to suicidal ideation, suicidal behavior, and suicide death, referred to here collectively as suicide (
1). Insomnia has had an evolving definition over the past 30 years and is now defined as a complaint of inadequate duration or poor quality of sleep, with adverse daytime consequences, despite adequate opportunity to sleep (
2). Insomnia often accompanies psychiatric disorders, but it can also be related to chronic pain or other medical conditions. The relationship between insomnia and suicide is maintained after controlling for symptoms of depressive illness (
3). It is not clear whether insomnia is causally related to suicide or is an indicator for another factor that drives the risk for suicide, such as CNS and psychological hyperarousal (
1).
The insomnia-suicide association suggests that treatment of insomnia would reduce the risk of suicide. This hypothesis is currently being tested in a multisite randomized clinical trial (
4). In the meantime, the proposition of routinely prescribing hypnotic medications to suicidal depressed patients is countered by the fact that hypnotics can be part of an intentional overdose or may induce or aggravate suicidal thoughts. The latter possibility has public health significance, as 3% of noninstitutionalized adult Americans report past-month use of a hypnotic (
5). Up to 10% of adults in the United States use over-the-counter sleep aids (
6), but over-the-counter sleep aids have not been linked with suicide and carry no Food and Drug Administration (FDA) warnings about suicide, and they will not be considered further in this article.
There have been previous reviews of the relationship between hypnotics and suicide. One study found increased rates of suicide death among hypnotic users and hypothesized that the relationship resulted from an impairment of judgment and promotion of violent and risky behaviors (
7). A review of sedative-hypnotic agents similarly concluded that hypnotics could increase the risk of suicide through disinhibition and that a definitive answer as to whether hypnotics increase or reduce risk requires trials specifically naming suicide as the primary outcome (
8). The most recent summary of this topic is a commentary on a single epidemiological survey reviewed below (
9).
Based on available reviews and epidemiological surveys, the link between sedative-hypnotic agents and suicidality appears to be uncertain. However, no review has considered published case reports of suicide death as related to hypnotic medication or considered adverse event reports on suicide and hypnotics in the FDA’s 2006 postmarketing safety review of zolpidem, zaleplon, and eszopiclone (the “Z-drugs”) (
10).
Before 2006, the FDA required that package labels for hypnotics include a warning about the risk of prescribing hypnotics to patients with severe depression, “particularly the recognition that suicidal tendencies may be present and protective measures may be necessary” (flurazepam label). By 2006, the FDA expressed concern that there was an increased risk of suicide linked to the newer Z-drugs (
10). Correspondingly, the package labels for zolpidem, zaleplon, and eszopiclone include the following statement: “In primarily depressed patients, worsening of depression, including suicidal thoughts and actions (including completed suicides), has been reported in association with the use of sedative/hypnotics.” The labels of hypnotics subsequently approved by the FDA (doxepin at 3 mg and at 6 mg, and ramelteon) also include this warning. However, the label of suvorexant, the agent most recently approved by the FDA for insomnia treatment, also included a stronger statement: “In clinical studies, a dose-dependent increase in suicidal ideation was observed in patients taking Belsomra as assessed by questionnaires.” Ramelteon, doxepin at 3 mg and at 6 mg, and suvorexant have mechanisms of action different from benzodiazepine hypnotics and the Z-drugs, all of which are positive allosteric modulators of the GABA type A receptor at the benzodiazepine binding site. Therefore, an increased risk of suicide with ramelteon, doxepin, or suvorexant would signal a broader problem with hypnotics, beyond the GABA-ergic mechanism of benzodiazepines and Z-drugs.
These warnings have ambiguous implications. They could give the impression that all hypnotic prescriptions are associated with a significant risk of suicide, but they do not address whether suicide risk is elevated more with some hypnotics than with others or in depressed insomniacs relative to nondepressed insomniacs. The warning also does not speak to the temporal association between hypnotic use and suicidality. For example, would risk be greater in the interval just after initiation of the prescription, but less so in the long term, or would risk be greater during the period of peak drug effect, and less so hours after significant drug metabolism has occurred?
We have conducted a review of the medical literature and FDA documents to provide greater clarity with respect to these possibilities. Our aim is to describe the toxicology of hypnotics in the setting of suicide, the epidemiological relationship between hypnotic use and suicide, and illustrative case data on hypnotics and suicide as found in the published literature and FDA databases that have generally not been included in published reviews of the relationship between sedative-hypnotic medications and suicidality.
Method
This review focused on modern, FDA-approved hypnotics, beginning with the introduction of benzodiazepines, and it excludes non-FDA-approved barbiturate hypnotics, ethchlorvynol, and chloral hydrate. Therefore, the medications of principal interest are flurazepam, temazepam, triazolam, estazolam, quazepam, zolpidem, zaleplon, eszopiclone, ramelteon, doxepin at 3 mg and at 6 mg, and suvorexant. This review is limited to adults 18 years old and older, as there was insufficient information to form opinions regarding effects in children and adolescents. The literature search process began with an inspection of the FDA-approved labeling of all of these agents and then proceeded to a PubMed search that crossed the terms “suicide” and “suicidal” with each of these agents. A similar process was undertaken with the Web of Science database in the hope of locating relevant abstracts that might not be found in PubMed. Next, the FDA web site was searched for postmarketing safety reviews and for commentaries on adverse event reporting for each agent considered. The bibliographies of each document were examined for additional relevant citations. Finally, under the Freedom of Information Act, the FDA was contacted from December 2015 through February 2016 with requests to provide detailed case reports for hypnotic-related suicide deaths reported through the FDA Adverse Event Reporting System, specifically for those medications that have no accounts published in the medical literature of suicide death by single-agent overdose. We examined FDA reports from as far back as the 1970s to capture adverse events related to flurazepam and all subsequent FDA-approved hypnotics.
We note that a meta-analysis, although preferred, could not be carried out because of limitations of the available data, including few studies with the same types of design and nonuniformity in the types of outcomes reported.
Results
Hypnotic Toxicology Studies in Suicide Victims
Studies from the United States.
Our review found one hypnotic medication toxicology study from the United States. Toxicology findings of 187 consecutive suicide victims (137 men and 50 women; mean age=44 years) from the San Diego coroner’s office in 1981 and 1982 indicated that hypnotics were found in 10.7% of cases, and a third of those taking hypnotics also tested positive for alcohol (
11). There were no cases in which a benzodiazepine was the only drug detected and also judged to be the sole cause of death. The authors of the study concluded that in cases of suicide related to benzodiazepines, multidrug overdoses are of primary concern.
Studies outside of the United States.
Our review found two hypnotic medication toxicology studies from outside the United States. A study of 1,467 suicide deaths in Switzerland in 1990 reported 22 cases in which a benzodiazepine hypnotic was the single agent leading to a suicide poisoning (1.5% of all suicide deaths); there were 16 cases involving flunitrazepam, four with midazolam, and two with triazolam (
12). However, the authors conceded that the role of alcohol in these single-agent cases may have been underestimated.
A study of 2,245 elderly suicides in 2003 using the Swedish Cause of Death Register found that 548 of the suicides were by poisoning, with benzodiazepines playing a role in 216 cases. A single benzodiazepine was the cause of death in 155 cases, and these included the hypnotics flunitrazepam (N=104), nitrazepam (N=36), and triazolam (N=1) (
13). Upon reviewing all suicides in Sweden between 1992 and 1996, the authors found that after correcting for the differences in rates of prescribing for flunitrazepam, nitrazepam, zopiclone, and zolpidem, the associations between these four hypnotics and suicide were about the same, with approximately one suicide per million daily doses of each drug. Together, these toxicology studies show that modern hypnotics are often involved in suicide deaths but are usually taken in combination with other sedatives or alcohol.
Retrospective Cohort Studies on the Topic of Hypnotics and Suicide
Studies from the United States.
We found one retrospective cohort study from the United States. A secondary analysis of the National Comorbidity Survey Replication surveyed 5,692 randomly selected community-dwelling adults between 2001 and 2003, with 5.8% of respondents answering “yes” to a question inquiring about the use of sleeping pills such as zolpidem or zaleplon in the past 12 months (
14). Of these, 2.6% endorsed suicidal thinking in the past 12 months, 0.7% endorsed suicide plans, and 0.4% admitted to a suicide attempt. Hierarchical multivariate logistic regression models, with suicidal thinking, plans, and behaviors as the dependent variables, and with hypnotic use as the independent variable adjusting for gender, age, ethnicity, marital status, education, poverty status, general health conditions, mood disorders, anxiety disorders, substance use disorders, and insomnia, indicated odds ratios of 2.2 (95% CI=1.5–3.3) for suicidal ideation, 1.9 (95% CI=1.1–3.3) for suicide plan, and 3.4 (95% CI=1.6–7.4) for a suicide attempt, as compared with persons who did not use hypnotics. Strengths of the study include its representative sampling technique, large size, adjustment for insomnia, and inclusion of the Z-drugs. Weaknesses include lack of consideration of high-risk personality disorders, lack of measurement of the severity of depressive illness, the possibility of recollection bias, lack of measurement of completed suicide deaths, and a retrospective design that makes it impossible to understand the temporal association between hypnotic use and suicidal phenomena. Overall, the study adds credence to the idea that in some instances hypnotics may increase risk for suicide, but the study does not shed light on mechanism. The authors correctly point out that clinical trials are required to show causality between hypnotics and suicide. However, the authors calculated the sample size required to identify a difference between hypnotics and placebo in rates of suicide attempts in a sample of insomniacs, and this calculation yielded a sample size of 1,068 participants (534 per group). It seems unlikely that such a large trial would ever be attempted; therefore, there is justification for trials to detect a proxy risk factor, such as suicidal ideation, rather than suicide attempts.
Studies outside of the United States.
We discovered two retrospective case-control studies from outside the United States on the topic of suicide and hypnotics. A retrospective case-control study examined medications prescribed to 25 Finnish psychiatric inpatients who died by suicide during their hospitalization, compared with 25 inpatient comparison subjects matched on age, gender, and psychiatric diagnosis (schizophrenia [N=14]; major depression [N=7]; personality disorder [N=3]; “neurosis” [N=1]) (
15). The suicide victims were more likely to be receiving a benzodiazepine (72%) than the comparison subjects (44%) (p<0.05). Limitations included lack of detail on whether the benzodiazepines were prescribed for anxiety or insomnia, lack of matching the groups on severity of symptoms, and small sample size.
The second study reported on the association between zolpidem and suicide (defined here as suicide death plus hospitalizations for suicide attempt) from a Taiwanese nationwide register covering 2002–2011. Each suicide case was matched on age, gender, occupation, and urban or rural setting with 10 comparison subjects without a history of suicide attempts (
16). The adjusted odds ratio for exposure to zolpidem was 2.08 (95% CI=1.83–2.36) and remained significant regardless of whether depression, insomnia, anxiety, bipolar disorder, or other comorbidities were present. However, the study was limited by imprecision in establishing the diagnoses of depression, insomnia, and other mental disorders and by the lack of measurement of severity of symptoms. The investigators speculated that zolpidem use could lead to a “dreamlike confusion state [that may] cause bizarre behavior [and] lead to potentially dangerous self-harm and even fatality” (
16).
Prospective Cohort Studies Regarding Hypnotics and Suicide
Studies from the United States.
Our review produced one prospective cohort study regarding hypnotics and suicide. In 1982, the American Cancer Society evaluated frequency of use of “prescription sleeping pills” in a convenience sample of 1,099,830 participants (
17). Respondents self-determined whether they were taking a “prescription sleeping pill,” and hence the data likely mixed benzodiazepines with barbiturates and antidepressants. The sample was followed prospectively until 1986. During this interval, adjusted hazard ratios for suicide were elevated in men (1.32) and women (1.22) who had nightly use of “prescription sleeping pills,” compared with those who did not, after controlling for body mass index (BMI), cigarette smoking, diet, and other mortality predictors. Apart from the nonrepresentative nature of the sample and poor characterization of “prescription sleeping pills,” another weakness of the study included failure to take into account psychiatric diagnoses. The authors called for the measurement of suicidal ideation and behavior in clinical trials.
Studies outside of the United States.
This review produced three prospective cohort studies from outside the United States that examined hypnotics and suicide. The first of these studies examined 26,952 adult Swedes between 1975 and 1981, 500 of whom (2%) were frequent hypnotic users (345 women and 155 men), and tracked suicides until 1985 in the national Cause of Death Registry (
18). Subsequent suicides were found in 1.1% of hypnotic-treated women, compared with 0.1% of the women not taking hypnotics (odds ratio=2.6, p<0.05). No men died by suicide. Study strengths include prospective measurement, which reduces ascertainment bias risk. Weaknesses include the inability to adequately control for depression diagnoses, other psychiatric disorders, and insomnia, which are known risk factors for suicide, and the failure to define “hypnotics.”
In the second prospective cohort study, the rate of suicide attempts among benzodiazepine users was evaluated in persons enrolled in the Saskatchewan Health Databases (
19). The study compared 225,796 adults taking benzodiazepines (all new prescriptions from 1979 to 1986) and 97,862 age- and gender-matched comparison subjects. The benzodiazepines included triazolam, flurazepam, lorazepam, diazepam, and oxazepam. Relative to comparison subjects, patients receiving an antidepressant concurrent with a benzodiazepine did not have increased rates of suicide attempt or suicide death over the 60 days following the filling of a new benzodiazepine prescription. In contrast, patients not taking an antidepressant when filling a benzodiazepine prescription had six times the odds (odds ratio=6.2, p<0.05) for suicide attempt or suicide death during the 60 days after the filling of a prescription, relative to comparison subjects. The authors speculated that “benzodiazepines may cause disinhibition, consisting of poor impulse control, and paradoxical reactions that may induce suicidal impulse” (
19). Weaknesses of the study include the confounding of treatment (benzodiazepines and antidepressants) with diagnoses, as mood disorder diagnoses were not considered in the analyses.
In the third prospective cohort study, cause-specific mortality was tracked for 20 years in a randomly selected sample of 1,750 men and 1,773 women who responded to a mail survey in Sweden in 1983 asking, “How often do you use sleep medication?” (
20). Data were collected regarding sleeping problems, medical diagnoses, depression, and BMI. There were 19 suicide deaths (10 men and nine women). The adjusted hazard ratio for suicide among regular male hypnotic users was 21.2 (95% CI=2.6–173.7), and the hazard ratio in women was 24.3 (95% CI=4.4–132.2). Limitations include the small number of observed events, the lack of measurement of alcohol and substance abuse, and uncertainty as to what medications were being included among “sleep medications.” The authors concluded that regular hypnotic use is an indicator of increased risk of mortality, including suicide, but that the study design did not show causality. They called for clinical trials to clarify the directionality of these relationships.
Collectively, these prospective cohort studies show an association between hypnotic use and suicide, but all of these studies suffer from confounding of hypnotic use with psychiatric and substance abuse diagnoses.
Illustrative Cases on the Topic of Hypnotics and Suicide
Flurazepam (original approval April 7, 1970).
•
The toxicology results from a suicide were reported in which the only drug isolated was flurazepam, and measures of postmortem flurazepam concentration in the blood indicated ingestion of 80 30-mg tablets (
21). Alcohol was not involved.
•
A 52-year-old woman with a history of depression and prior suicide attempts was found dead in her bed (
22). Toxicology reports on blood, urine, and bile indicated the presence of flurazepam only and no other drugs, poisons, or alcohol, as well as the equivalent of 20 30-mg flurazepam tablets in her stomach. A total of 70 flurazepam tablets were missing from a prescription filled 2 days earlier.
•
A 68-year-old woman was found dead at home with no evidence of trauma (
23). Her body was surrounded by empty medication boxes. Autopsy results revealed no evidence of significant natural disease. Toxicology reports revealed a blood flurazepam level of 2.8 μg/mL. Other than a trace amount of alcohol in her blood (0.1 mg/mL), no other drugs were detected. The authors postulated that the cause of death was respiratory depression due to a single-drug overdose from flurazepam.
Temazepam (original approval Feb. 27, 1981).
There are two cases in the medical literature of suicide from temazepam as a single agent (
24,
25), four cases reported by poison control centers (
26–
29), and two more adverse event reports from the FDA, altogether accounting for eight cases of suicide death from overdose of temazepam as a single agent. These cases included six men (ages 49, 66, 73, 74, 77, and 92 years) and two women (ages 83 and 85 years). The suicide of the 73-year-old man occurred after he took temazepam for only 2–3 nights, and he gave no prior indication that he was suicidal.
Triazolam (original approval Nov. 15, 1982).
•
A 77-year-old woman was found dead at home. Empty triazolam bottles were at the scene (
30). A complete autopsy report was unremarkable. Toxicological analysis of blood and urine indicated no alcohol or other drugs besides triazolam.
•
A 57-year-old man was found dead outdoors in winter in Japan (
31). A full autopsy report failed to reveal a cause of death from natural causes. Stomach contents included 8.4 mg of triazolam (equivalent to 33 0.25-mg tablets). Toxicological analysis of blood and urine revealed high levels of triazolam but no other drugs.
•
Two additional cases of suicide death were reported due to triazolam alone, as confirmed by gas chromatography and mass spectrometry (
32).
Quazepam (original approval Dec. 27, 1985).
There are no published cases of suicide with quazepam. A search of the FDA’s adverse event files failed to reveal any possible single-agent suicide deaths related to quazepam.
Estazolam (original approval Dec. 26, 1990).
There are no published cases of suicide with estazolam. A search of the FDA’s adverse event files failed to reveal any possible single-agent suicide deaths related to estazolam.
Zolpidem (original approval Dec. 16, 1992).
•
A 68-year-old woman was found dead in her bed with an empty bottle of zolpidem (at 10 mg), 30 pills of which had been dispensed the day before (
33).
•
A suicide death of an 86-year-old woman who drowned in her bathtub after ingestion of zolpidem as a single-agent overdose was reported and confirmed by gas chromatography and mass spectrometry (
34).
•
Two cases of suicide death from zolpidem poisoning were reported, including the case of a 58-year-old woman in which zolpidem was a single agent, as confirmed by gas chromatography (
35).
Apart from suicide deaths, there are numerous publications of suicide attempts that occurred during intoxication with zolpidem. A compilation of spontaneous adverse event reports from Australia between 2001 and 2008 indicated that zolpidem had higher odds for “parasomnia, amnesia, hallucinations, and perhaps suicidality compared to either all other drugs or hypnotics” (
36). This study calculated an odds ratio of 8.3 (95% CI=5.4–12.8) for suicidality related to zolpidem compared with other psychotropic drugs in the survey. The authors acknowledged that a role for alcohol in the findings could not be ruled out, and they implicitly raised the concern that some of the unexpectedly high risk for suicide attempts with zolpidem could be related to a higher rate of parasomnia behavior during the period of peak drug effect. This possibility is supported by several detailed case reports.
A report of 91 coroner cases from New South Wales, Australia, between 2001 and 2010 noted two cases of “bizarre, dissociative” behavior leading to suicide death in decedents with toxicology-proven zolpidem use (
37). In one case, the person was dancing on a high ledge before falling, and in another case, the person impulsively jumped out of a window during an argument. A 27-year-old man with no known history of psychiatric illness, suicidal ideation, or sleep disorder took 20 mg of zolpidem, in the absence of alcohol, and then took an additional 40 mg sometime in the middle of the night. The patient’s only explanation was that he remembered feeling suicidal later in the night (
38).
The FDA’s postmarketing safety review of the Z-drugs in 2006 included additional adverse event reports for zolpidem that were not found in the medical literature (
10). The FDA report describes a total of 49 suicidal-related adverse events in which zolpidem was judged to be a factor, including suicidal ideation (N=12), suicide attempt or self-harm (N=16), and suicide deaths (N=21). In nine of the 49 cases, there was no prior history of psychiatric illness, and in eight cases, there was no other use of psychotropic medication. In one instance, a 33-year-old man with no history of mental illness took zolpidem for 4 or 5 nights, then on the last night took 10 mg of zolpidem at 2:30 a.m., awoke at 6 a.m. (3.5 hours later), went to work, and the next thing he remembered was “standing on a pile of boxes with a noose around his neck.” In another case, a 38-year-old man with no history of mental disorder began using 10 mg of zolpidem and died by suicide on the fourth day (method not described). Finally, a 39-year-old man with no history of mental illness took 10 mg of zolpidem for 3 nights. On the third night, his wife “found him sleep walking in the closet with no memory of how he got there.” The next morning he “could not focus” and walked into the woods and shot himself. The FDA report summarized the zolpidem cases by noting that the suicidal events often occurred within a week of initiation and that many were accompanied by bizarre behavior, hallucinations, or paranoia.
Zaleplon (original approval Aug. 13, 1999).
While there are no published cases of suicide with zaleplon, the FDA’s postmarketing safety review described one case of suicidal ideation, three cases of self-harm or suicide attempt, and three cases of suicide death related to zaleplon; however, only one of these cases had no prior psychiatric history. All of the zaleplon adverse events occurred within 14 days of drug initiation (
10).
Eszopiclone (original approval Dec. 15, 2004).
Sixty instances of poisoning with eszopiclone as a single agent were reported in Texas between 2005 and 2006 (
39). There were no instances of death when eszopiclone was taken as a single agent in an overdose. However, the FDA’s postmarketing safety review described 16 suicide-related adverse events, including seven cases of suicidal ideation, five cases of self-injury or suicidal attempt, and four suicide deaths. A psychiatric history was reported in all but one case, and in 13 cases the adverse event occurred within 1 month of initiation. Several cases were accompanied by “irritability, agitation, confusion, or worsening depression” before the event (
10).
Ramelteon (original approval July 22, 2005).
There are no published cases of suicide with ramelteon. A search of the FDA’s adverse event files failed to reveal any possible single-agent suicide deaths related to ramelteon.
Doxepin at 3 mg and at 6 mg (original approval March 17, 2010).
There are no published cases of suicide with doxepin prescribed in low dosages for insomnia.
Suvorexant (original approval Aug. 13, 2014).
In 2012, the FDA recommended prospective, systematic assessment of suicide in all clinical trials used in the registration of any new psychoactive medication. The Columbia-Suicide Severity Rating Scale was specifically named as a suitable instrument for this purpose (
40). Consequently, the research and development of suvorexant followed these FDA recommendations, and the findings were reported at the FDA suvorexant advisory committee meeting in 2013 (
41). Per the 2012 FDA recommendations, data were pooled across all phase III trials. In the case of the new drug application for suvorexant, this meant the collation of one combined-age, blinded, randomized, high-dose trial and one blinded, randomized, combined-age, low-dose trial. High dose and low dose were defined as follows: young adults: low dose of 20 mg and high dose of 40 mg; elderly (individuals older than age 65): low dose of 15 mg and high dose of 30 mg. A total of 11 persons expressed suicidal ideation across both studies, as defined by the Columbia-Suicide Severity Rating Scale (
Table 1).
While there were no suicidal behaviors reported, and while the majority of suicidal ideation events lasted “minutes to hours and were mild to moderate in intensity,” the FDA interpreted the results as supporting a dose-response relationship between suvorexant exposure and suicidal ideation (
41). As a result, the package label for suvorexant carries the unique warning that “in clinical studies, a dose-dependent increase in suicidal ideation was observed in patients taking Belsomra as assessed by questionnaires.” Examination of the specific cases of suicidal ideation as described in the advisory committee meeting shows that the data collection method failed to record whether suicidal ideation occurred in temporal proximity to drug ingestion (i.e., at night, within a few hours of ingestion) or later in the day after the drug effect would have dissipated. Finally, a search of the FDA’s adverse event files failed to reveal any possible single-agent suicide deaths related to suvorexant.
Discussion
Toxicology studies show that modern hypnotics have frequently been taken before suicide deaths, although the hypnotics are often taken in combination with other sedatives or alcohol. Still, death is possible when hypnotics are used as a single agent for self-poisoning, and we found examples of this for flurazepam, temazepam, triazolam, and zolpidem. While the available data might give the impression that some hypnotics are more likely than others to be associated with suicide, this conclusion should be tempered by the large variation in the time that different agents have been available and by different rates of prescribing (
42).
The retrospective case series have consistently shown that hypnotic users are overrepresented among suicide victims, with odds ratios in the range of 2–3, but these studies have been unable to disentangle the confounding effect of treatment and diagnosis. Similarly, the prospective cohort studies show elevated odds and hazard ratios from 1.2 to 24.3. The prospective design solves the problem of demonstrating exposure to hypnotics before the suicide event, but three of the available prospective cohort studies did not collect information about diagnosis, so treatment and diagnosis are again confounded. The fourth of these studies considered psychiatric diagnosis but not alcohol or substance abuse. Understandably, the retrospective and prospective cohort studies call for clinical trials to disentangle diagnoses and treatment effects. The implications of cohort studies are weakened by the frequent omission of a definition of what was considered a “hypnotic” and by the inclusion of medications not usually considered hypnotics (i.e., phenothiazines). The clinical trials of suvorexant are the only hypnotic trials that have prospectively and systematically measured suicidal ideation, and the pooled data may suggest a dose-response relationship between suvorexant exposure and risk of suicidal ideation in individuals with primary insomnia, albeit a small risk.
The possibility of a causal relationship between suvorexant exposure and suicidal ideation raises the question of whether risk of suicide is limited to the benzodiazepine receptor mechanism or whether suicide risk may be a more general risk from exposure to various types of hypnotics. A common feature of risk could be disinhibition or increased impulsivity during the time of peak drug effect for some hypnotics.
This scenario is reinforced by published case reports and by FDA adverse event reports that show that some suicidal behaviors and suicide deaths occur during a period of confusion, amnesia, hallucination, or paranoia in the first few hours after ingestion of a hypnotic; that is, that suicide is linked to hypnotic-induced parasomnia during the time of peak drug effect. Cognitive impairment, specifically problems with decision making and executive function, are common to both insomnia and suicide (
43,
44); hence, further cognitive impairment at the time of peak drug effect may further tilt the balance toward suicide. The risk of this scenario appears to be higher if the drug is consumed with alcohol, if it is taken at a dosage higher than recommended, or if the patient does not go to bed or fall asleep soon after ingestion or awakens a few hours after ingestion. This proposition does not address whether suicide risk is higher in hypnotic users during those hours long after the drug should have been metabolized. For example, is the risk of suicide elevated in a person who consumes zolpidem at 9:50 p.m., is in bed by 10:00 p.m., sleeps uninterrupted for 8 hours, and rises at 6 a.m. (assuming that the drug is nearly completely eliminated by that time)?
At the same time, however, the possibility remains open that judicious prescription of hypnotics, when taken appropriately, might reduce (not increase) the risk of suicide. While this premise has not been directly tested, it has been shown that the addition of an FDA-approved hypnotic to an antidepressant will improve the overall rates of response to the antidepressant (
45,
46), and it is reasonable to posit that superior antidepressant response would lead to superior reduction in suicide risk. Although alprazolam is approved as a benzodiazepine anxiolytic and not as a hypnotic, a meta-analysis of alprazolam clinical trials nonetheless showed that alprazolam was no more likely than placebo to be associated with the emergence of worsening of suicidal ideation and that alprazolam was more likely than placebo to be associated with an improvement in preexisting suicidal ideation (
47).
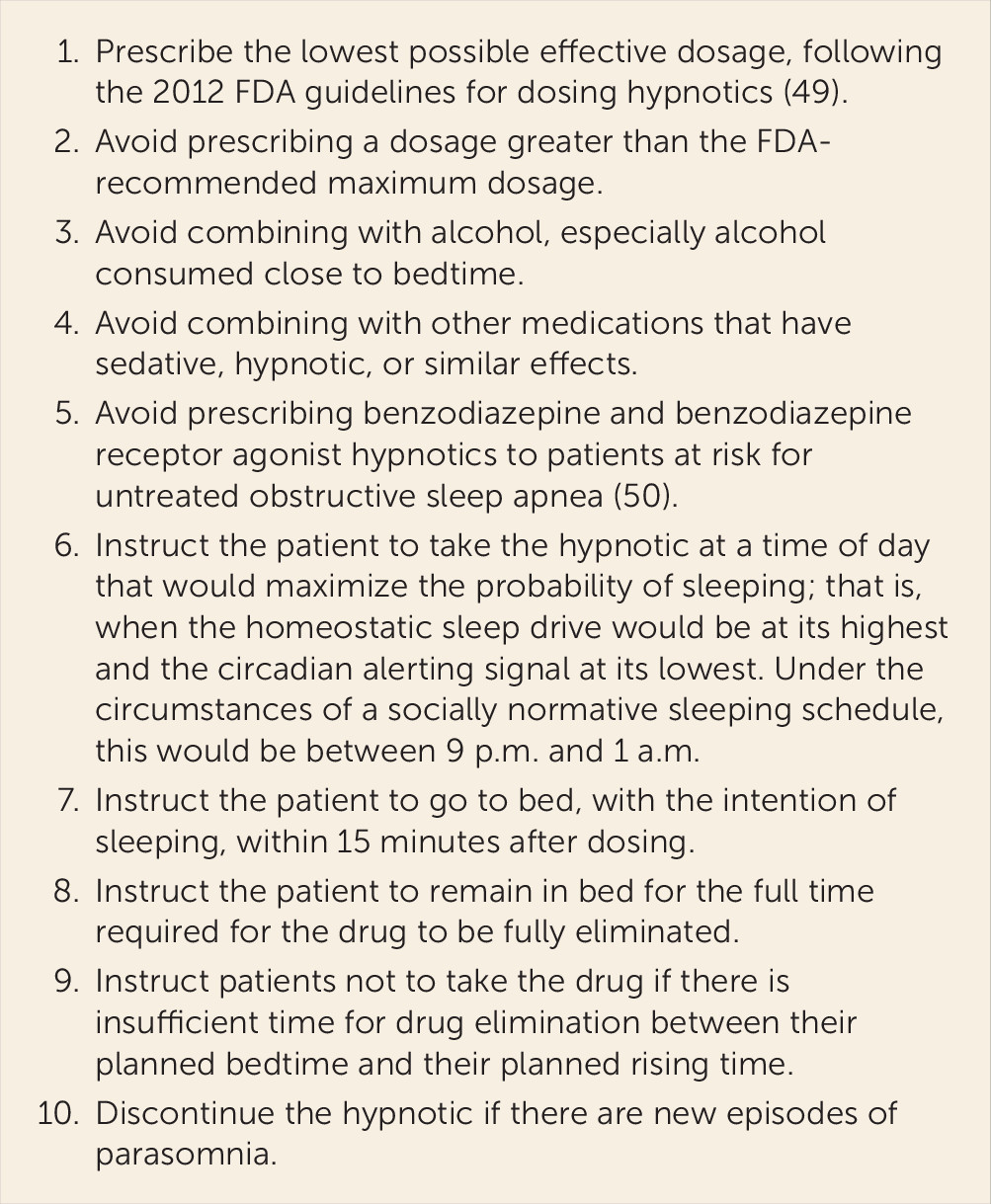
The principal new contribution of this review is the clarification regarding the timing of suicide risk related to ingestion of hypnotics. Under specific conditions, hypnotics may induce or exacerbate suicidality by altering consciousness or disinhibition at the time of peak drug effect, and at the same time may reduce or prevent suicidal ideation in persons with insomnia and mental illness after appropriate drug metabolism. While the latter possibility is being evaluated, the risk of the former might be reduced through the steps outlined in
Figure 1 when prescribing hypnotics.