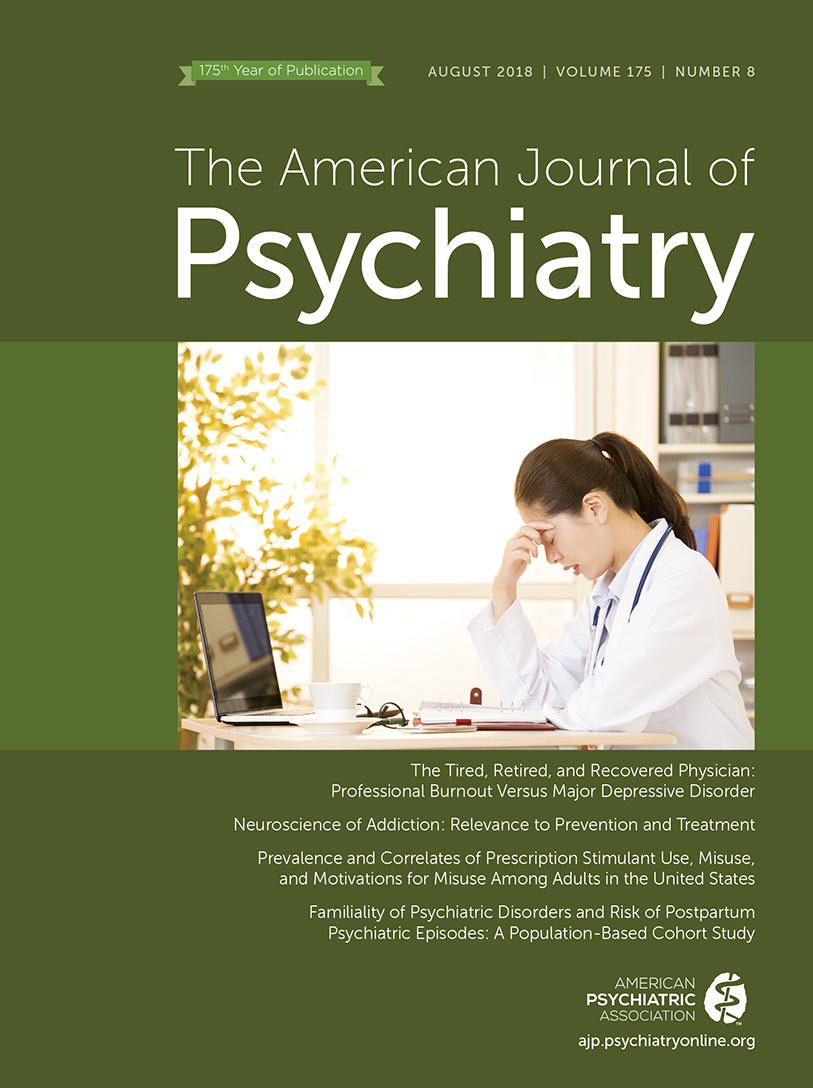
The Tired, Retired, and Recovered Physician: Professional Burnout Versus Major Depressive Disorder
Interventions to Address Burnout in Health Care Professionals
| Mayo Clinic: Nine Organizational Steps | Institute for Healthcare Improvement: Improving Joy in Work | Joy in Practice Framework |
|---|---|---|
| 1. Acknowledge and assess the problem | 1. Physical and psychological safety | 1. Design organizational systems to address human needs |
| 2. Harness the power of leadership | 2. Meaning and purpose | 2. Develop leaders with participative management competency |
| 3. Develop and implement targeted interventions | 3. Choice and autonomy | 3. Build social community |
| 4. Cultivate community at work | 4. Recognition and rewards | 4. Remove sources of frustration and inefficiency |
| 5. Use rewards and incentives wisely | 5. Participative management | 5. Reduce preventable patient harm and support second victim |
| 6. Align values and strengthen culture | 6. Camaraderie and teamwork | 6. Bolster individual wellness |
| 7. Promote flexibility and work-life integration | 7. Daily improvement | |
| 8. Provide resources to promote resilience and self-care | 8. Wellness and resilience | |
| 9. Facilitate and fund organizational science | 9. Real-time measurement |
Burnout Versus Depression
Advantages and Disadvantages of Conceptualizing Burnout as Depression
Distinguishing Burnout From Depression
“In distinguishing burnout from a major depressive episode, it is useful to consider that in burnout the predominant affect is feelings of exhaustion, cynicism, and inefficacy, whereas in major depressive episode it is persistent depressed mood and the inability to anticipate happiness or pleasure. The dysphoria in burnout is likely to correlate with fluctuations in workload demands (24), whereas the depressed mood in a major depressive episode is more persistent and is not tied to specific thoughts and preoccupations. The pain of burnout may be accompanied by positive emotions and humor that are uncharacteristic of the pervasive unhappiness and misery seen in a major depressive episode. The thought content associated with burnout generally features a preoccupation with work rather than the self-critical or pessimistic ruminations seen in major depressive episode. In burnout, self-esteem is generally preserved, whereas in major depressive episode, feelings of worthlessness and self-loathing are common. If self-derogatory ideation is present in burnout, it typically involves perceived failings related to work.”
| Major Depressive Episode (DSM–5) | Burnout Syndrome |
|---|---|
| Depressed mood | Emotional exhaustion—stress response |
| Diminished interest or pleasure | Depersonalization or cynicism—negative response to job and to others |
| Changes in body weight or appetite | Reduced personal accomplishment or inefficacy—negative response to self |
| Changes in sleep habits | |
| Psychomotor agitation or retardation | |
| Fatigue or loss of energy | |
| Diminished ability to think or make decisions | |
| Feelings of worthlessness or unwarranted guilt | |
| Recurrent thoughts of death |
Conclusions
References
Information & Authors
Information
Published In
History
Keywords
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).