Like the elephant is to the eight blind men, physician burnout is many things to many people. I have been reading about, conducting research on, and talking to many psychiatrists about burnout for 3 years, and here is my understanding of burnout—eight things it is, and eight things it is not. Only some major points are referenced here, but everything I discuss is supported in the literature on burnout.
Burnout Is…
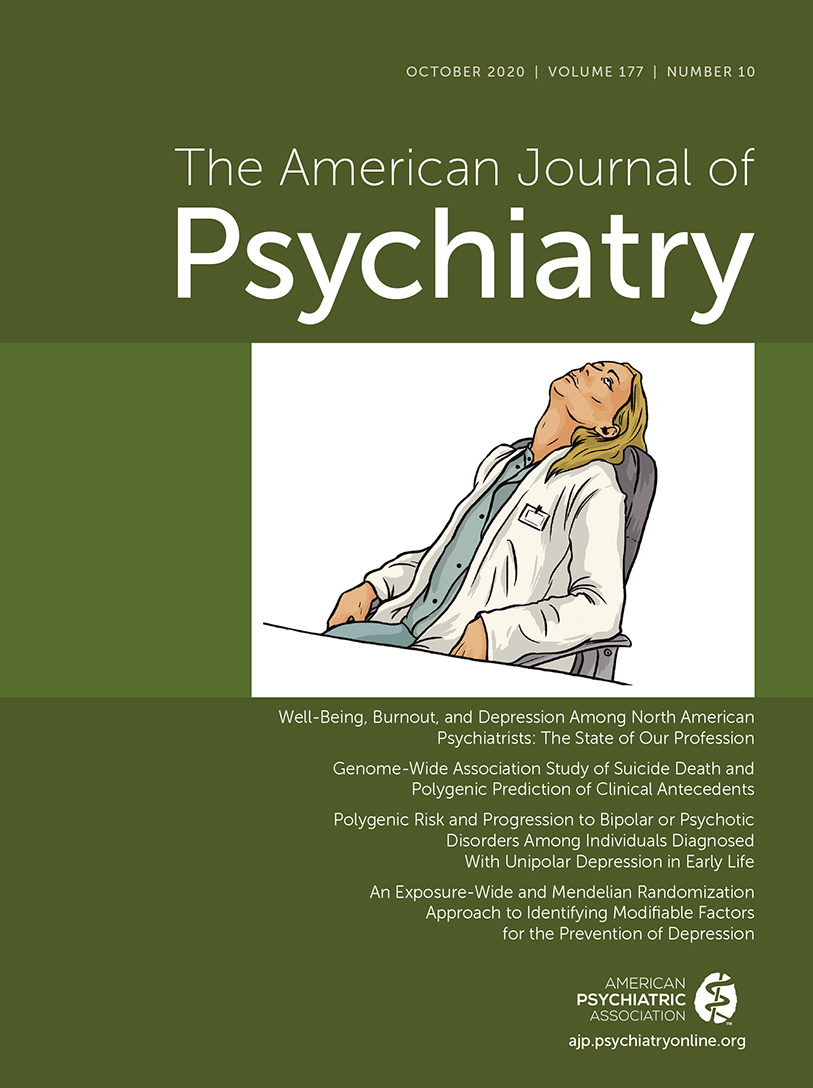
Burnout is a painful and lonely experience, often involving depersonalization, exhaustion, and a decreased sense of effectiveness, that has an insidious onset and takes many physicians by surprise.
Burnout is a mismatch between physicians’ expectations of their work and their actual experience, including the role of work in their lives and their work-life balance.
Burnout involves the loss of meaning in work, frequently a sense of curtailed autonomy, and almost always a loss of connection to community.
Burnout is a way to talk about problems in the workplace that feels more legitimate and less stigmatized than “complaining” and that exposes the culture of medicine’s limited space for sharing about negative emotions.
Burnout is an umbrella term for a wide range of experiences with similarities and significant differences. Burnout can include moral injury, anxiety, trauma, cognitive impairment, and functional difficulty. It may occur at any point in the career life cycle.
Burnout appears to be a risk factor for psychiatric problems, such as depression, anxiety disorders, substance use, posttraumatic stress disorder, and neurocognitive problems, as well as family and relationship problems.
Burnout is a problem that affects subgroups of doctors differently. Among psychiatrists, there is an increased risk of burnout among women, younger doctors, those with less perceived autonomy, and, possibly, minority physicians (
1). Although burnout appears to be less prevalent among psychiatrists than among physicians in many other specialties, it is present among psychiatrists to a significant degree (
2).
Burnout is a problem that requires solutions on multiple levels: the economic system (employer-employee balance of control, investment in human capital or technology), the health care system (the physician’s role, technology, licensure and credentialing policies), health care organizations (physician productivity, electronic medical records, organization of services, relationship and management structure), departments and clinics (leadership, administrative structure, relationships, workflow, support), and individuals (healthy work-life balance, resilience enhancement, access to mental health services).
Burnout is Not…
Burnout is not a categorical phenomenon, and it is more accurate to speak about the degree of burnout than to regard it as a binary phenomenon with an arbitrarily established cutoff point on measurement scales.
Burnout is not a medical diagnosis or illness. ICD-11 includes burnout as a “factor influencing health,” not as a diagnosis, as has been widely reported in the media.
Burnout is not “complaining.”
Burnout is not a reflection of entitlement, millennial culture, laziness, or an erosion of standards in physician behavior.
Burnout is not depression, because it is a normal response to a stressful workplace, although there is substantial overlap between burnout and depression.
Burnout is neither a uniquely American problem nor a reflection of specific attributes of American medicine; it is increasingly evident in physicians in many other countries (
3).
Burnout is not a trivial problem. It has an immense human cost to the 1 million American physicians and a massive financial cost that is incurred because of increased turnover, decreased productivity, increased part-time status, early retirement, increased medical errors, and decreased academic productivity by physicians with burnout (
4–
7).
Burnout cannot be solved simply through more meditation, yoga, free ice cream on National Doctors’ Day, annual wellness retreats, or a positive attitude, although some or all of these may be very helpful.
Defining the contours of burnout gives us all a common language and space to discuss this modern-day scourge on medicine. We can use this emerging understanding of burnout to continue to develop interventions, study them, and work together to address this elephant in the room.