Anxiety, mood, and posttraumatic stress disorders are more common among individuals with an alcohol or tobacco use disorder than among the general population (
1–
3). Individuals with a co-occurring substance use disorder and other psychiatric disorders are at increased risk for negative health consequences and have greater risk in other domains, including economic difficulties, social isolation, homelessness, and incarceration (
4,
5), compared with individuals with substance use disorders and no comorbid psychiatric disorders. In addition, individuals with comorbid psychiatric disorders have poorer substance use disorder treatment outcomes compared with individuals without psychiatric comorbidities (
6–
9).
Studies have established that sexual minorities have a greater prevalence of alcohol and tobacco use disorders (
10–
13). Sexual minorities also have a greater prevalence of anxiety and mood disorders (
11,
14,
15); in particular, substantially elevated rates of posttraumatic stress disorder (PTSD) have been found among sexual minorities (
15). Although other psychiatric disorders are also of public health concern, for this study, we focused on mood and anxiety disorders and PTSD. Mood disorders include major depressive disorder, dysthymia, bipolar I disorder, and bipolar II disorder. Anxiety disorders include generalized anxiety disorder, specific phobia, social anxiety disorder, panic disorder, and agoraphobia based on DSM-5 criteria (
16). Mood and anxiety disorders are two of the most prevalent types of psychiatric disorders in the United States, and both are highly comorbid with alcohol and tobacco use disorders (
17,
18). (Hereafter, we use the term comorbid psychiatric disorder to refer to comorbid mood and anxiety disorders. Hence, we use alcohol or tobacco use disorder psychiatric comorbidities to refer to alcohol use disorder comorbid with anxiety disorders, mood disorders, or PTSD, and to refer to tobacco use disorder comorbid with anxiety disorders, mood disorders, or PTSD.) Few studies have examined whether alcohol or tobacco use disorder psychiatric comorbidities are more prevalent among sexual minorities. One study using a Swedish sample examined the co-occurrence of alcohol and tobacco use with general psychological distress and found a stronger link among sexual minorities than among heterosexual individuals (
19). Another study using national U.S. data found that sexual minorities were overrepresented among those with alcohol use disorder and PTSD and those with a drug use disorder and PTSD (
9). However, few studies using national samples have examined sexual identity differences in the prevalence of alcohol or tobacco use disorder psychiatric comorbidities and their correlates.
The prevalence of alcohol use disorder, tobacco use disorder, and their psychiatric comorbidities differs between men and women (
20,
21). Sexual identity disparities also differ substantially for men and women. In particular, bisexual women are at heightened risk for alcohol, tobacco, and other substance use disorders (
12,
13), as well as anxiety and mood disorders (
14,
22), compared with heterosexual women.
The minority stress model (
23) is a prominent theory used to understand higher prevalences of substance use and psychiatric disorders among sexual minorities. A growing body of research has demonstrated that sexual minorities experience chronic and accumulating stressors in multiple domains of their lives specific to their identity as a sexual minority (
24). The domains include adverse childhood experiences and current stressful life events, which can be experienced by all individuals but occur more often among sexual minorities (
15,
25,
26). In addition to a higher prevalence of stressful experiences, sexual minorities often face stressors, such as sexual orientation discrimination, specific to being a member of a marginalized group (
27–
29). Adverse childhood experiences, stressful life events (
30–
32), and sexual orientation discrimination (
27–
29) are each associated with risk for alcohol or tobacco use disorder. However, it is not known whether each of these stress-related domains is also associated with co-occurring substance use and psychiatric disorders; moreover, these constructs are not often examined together in the same study.
More recent iterations of the minority stress model and related empirical research have demonstrated the importance of resilience and, in particular, highlighted the importance of considering social support and other potential protective factors (
33). Recent studies have found that social support is associated with lower odds of alcohol use disorder among sexual minority men (
34) and that a lack of social support (social isolation) is associated with problematic alcohol, tobacco, and marijuana use (
19).
In this study, we aimed, first, to examine the prevalence of the co-occurrence of psychiatric disorders with alcohol and tobacco use disorders by sex and sexual identity and, second, to examine whether stress-related risk and protective factors are associated with these comorbidities.
Methods
Participants
The data used in the study are from the nationally representative National Epidemiologic Survey on Alcohol and Related Conditions–III (NESARC-III) study, collected in 2012–2013. Noninstitutionalized civilian adults in the United States ages 18 and older (N=36,309) were surveyed via in-person interviews. Individuals were sampled at the household level, with oversampling for young adults (ages 18–24) and Black and Hispanic individuals (
35). Survey weights were used to adjust for oversampling of these groups and to account for varying rates of nonresponse. Household, person-level, and overall response rates were 72%, 84%, and 60%, respectively. Participants were informed in writing about the nature of the survey before they consented to participate in the study. Institutional review boards at both the National Institutes of Health and Westat approved the study protocol; the first author’s institution ruled the study exempt because it involved existing de-identified data. The analytic sample included all participants for whom valid data were available on sexual identity and other relevant covariates (N=35,796). The prevalence of psychiatric comorbidities was estimated among those who met criteria for a past-year alcohol use disorder (N=5,042) and a past-year tobacco use disorder (N=7,188). We examined correlates of psychiatric comorbidities among the full sample and among sexual minorities. For this study, sexual minorities included those who identified as gay or lesbian or bisexual, and individuals who identified as heterosexual but reported same-sex attraction or behavior (N=3,203).
Measures
Individuals reported which category best described them: heterosexual, gay or lesbian, bisexual, or not sure. Those who selected “not sure” were coded as missing. Previous research has shown the “not sure” group to have a distinct substance use risk (
10), but we did not have a sufficient sample size to examine this subgroup separately.
Past-year alcohol use disorder and tobacco use disorder were assessed using the National Institute on Alcohol Abuse and Alcoholism’s Alcohol Use Disorder and Associated Disabilities Interview Schedule–5 (AUDADIS-5). The AUDADIS-5 is a structured diagnostic interview that assesses DSM-5 diagnostic criteria and can be administered by nonclinician interviewers (
36). Consistent with DSM-5 criteria, a threshold of two symptoms was used to meet criteria for a diagnosis of alcohol use disorder or tobacco use disorder. We dichotomized each measure to compare those who met and did not meet criteria for a disorder in the past year. Because of the lower prevalence of other substance use disorders in the population and the heterogeneity within the “other” substance use disorder category, we focused on alcohol use disorder and tobacco use disorder in this study.
Past-year psychiatric disorders were also assessed with the AUDADIS-5 using DSM-5 diagnostic criteria. Past-year mood disorders (unrelated to substance use) included major depressive disorder, bipolar I and II disorder, and dysthymia. Past-year anxiety disorders included generalized anxiety disorder, specific phobia, social anxiety disorder, panic disorder, and agoraphobia. Past-year PTSD was examined as a separate psychiatric disorder.
Stress-Related Correlates
Individuals who identified as gay or lesbian, as bisexual, or as heterosexual and reported same-sex attraction or behavior were asked questions regarding sexual orientation discrimination. The discrimination measure was derived from the Major Experiences of Discrimination Scale (
37) and included six items assessed on a 4-point scale regarding the frequency of different types of discrimination (e.g., discrimination in health care settings, public settings, and obtaining a job). Responses were summed to create a scale ranging from 0 to 24. Adverse childhood experiences were assessed with 18 items (e.g., physical, sexual, and emotional abuse; exposure to family violence; parental incarceration) continuously in a scale ranging from 0 to 18. The measure of past-year stressful life events included 16 life events (e.g., moved, lost employment, divorced). We created a summary measure of the number of events experienced in the past year (scored from 0 to 16). Social support was assessed with 12 questions measuring perceived social support using items from the Interpersonal Support Evaluation List–General Populations (
38). Responses were on a 4-point scale ranging from definitely false to definitely true. Negative items were reverse coded such that higher scores indicated greater social support. The scale ranged from 0 to 48.
Control Variables
Multivariable regression analyses controlled for sex (male or female), sexual identity (heterosexual, bisexual, and gay or lesbian), race/ethnicity (White non-Hispanic, Black non-Hispanic, American Indian/Alaska Native non-Hispanic, Asian/Native Hawaiian/Other Pacific Islander non-Hispanic, and Hispanic), education (high school diploma or more, or less than a high school diploma), annual income (<$25,000, $25,000–$59,999, >$60,000), urbanicity (urban or rural), and region (Northeast, Midwest, South, and West).
Analysis
We first estimated psychiatric comorbidities (anxiety disorders, mood disorders, and PTSD) for alcohol use disorder and tobacco use disorder in the past year for men and women by sexual identity. We estimated the prevalence of these psychiatric comorbidities in the full sample (N=35,796), among those who met criteria for a past-year alcohol use disorder (N=5,133), and among those who met criteria for a past-year tobacco use disorder (N=7,303). Unadjusted bivariate logistic regression models were used to identify significant differences in comorbidity prevalence by sexual orientation using heterosexual-identifying individuals as the reference. Second, in the full sample (N=35,796), we examined stress-related correlates of alcohol and tobacco use disorder psychiatric comorbidities using six separate multivariable logistic regression models for each comorbidity. These correlates included stressful life events, adverse childhood experiences, and social support. Finally, we examined stress-related correlates of alcohol and tobacco use disorder psychiatric comorbidities among sexual minorities (N=3,202) using multivariable logistic regression models. Stress-related correlates among sexual minorities included sexual orientation discrimination, stressful life events, adverse childhood experiences, and social support. Multivariable logistic regression analyses controlled for sex, sexual identity, race/ethnicity, college degree attainment, family income, region, and urbanicity. All analyses were conducted using Stata’s svy procedures (
39) to account for the NESARC-III sample design.
Results
Descriptive Characteristics
Descriptive characteristics of the sample overall and by sexual identity and sex are summarized in
Table 1. Prevalence was significantly higher among bisexual and gay or lesbian individuals compared with heterosexual individuals for past-year alcohol use disorder, tobacco use disorder, anxiety disorders, mood disorders, and PTSD. Estimates for bisexual individuals were the highest of the three groups. One of the largest differences was the fourfold greater prevalence of PTSD among bisexual individuals (17.9%) compared with heterosexual individuals (4.4%). Men who identified as gay had a particularly high prevalence of past-year alcohol use disorder (31.4%, compared with 13.8% in the overall sample) and tobacco use disorder (40.8%, compared with 12.0% in the overall sample). Both gay men and bisexual men had a significantly higher prevalence of all disorders compared with heterosexual men. Bisexual women had a particularly high prevalence of anxiety disorders (32.5%, compared with 13.0% in the overall sample), mood disorders (34.9%, compared with 12.8% in the overall sample), and PTSD (21.0%, compared with 5.6% in the overall sample) and a significantly higher prevalence of alcohol and tobacco use disorders compared with heterosexual women. Gay or lesbian women had a higher prevalence of alcohol use disorder, tobacco use disorder, and mood disorders compared with heterosexual women.
Past-Year Alcohol Use Disorder, Tobacco Use Disorder, and Psychiatric Comorbidities by Sexual Identity and Sex
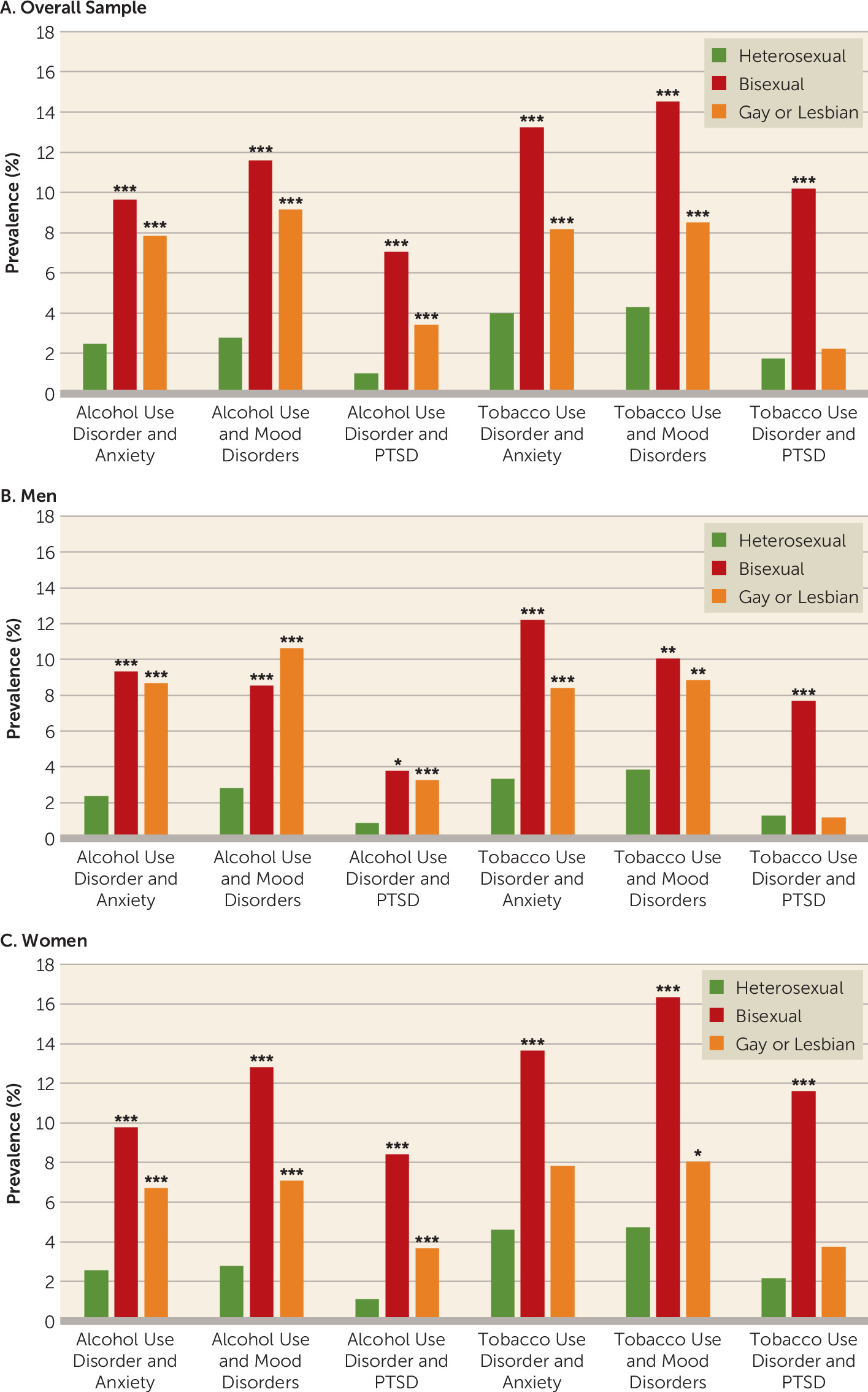
We examined the prevalence of past-year comorbid disorders by sexual identity and sex as follows: alcohol use disorder and anxiety disorders, alcohol use disorder and mood disorders, alcohol use disorder and PTSD, tobacco use disorder and anxiety disorders, tobacco use disorder and mood disorders, and tobacco use disorder and PTSD (
Figure 1). Bisexual men had a significantly higher prevalence of all psychiatric comorbidities compared with heterosexual men. Gay men had a significantly higher prevalence of all psychiatric comorbidities compared with heterosexual men, except for comorbid tobacco use disorder and PTSD.
Alcohol Use Disorder and Psychiatric Comorbidities
Among those meeting criteria for a past-year alcohol use disorder (N=5,133), 34.0% also met criteria for an anxiety disorder, mood disorder, or PTSD (see Figure S1 in the online supplement). Psychiatric comorbidities were more prevalent among bisexual (55.2%) and gay or lesbian (51.2%) individuals compared with heterosexual individuals (32.9%).
Among men, 25.8% of heterosexual men who met criteria for a past-year alcohol use disorder had a psychiatric comorbidity (anxiety disorder, mood disorder, or PTSD), compared with 42.8% of bisexual individuals who met criteria for a past-year alcohol use disorder and 66.1% of gay men who met criteria for a past-year alcohol use disorder. The difference was significant only for gay and heterosexual men. Bisexual men who met criteria for an alcohol use disorder were significantly more likely to have a comorbid anxiety disorder (29.7%) compared with heterosexual men (13.8%). Gay men who met criteria for a past-year alcohol use disorder were more likely to have a comorbid anxiety disorder, mood disorder, and PTSD; the estimated prevalence for each psychiatric comorbidity was more than double that of heterosexual men.
Overall estimates for psychiatric comorbidities (mood disorders, anxiety disorders, PTSD) of alcohol use disorder were higher among women who met criteria for an alcohol use disorder than among men. Among women, almost half (44.6%) of heterosexual women who met criteria for a past-year alcohol use disorder had a psychiatric comorbidity (mood disorder, anxiety disorder, PTSD). A majority of bisexual women who met criteria for a past-year alcohol use disorder had a psychiatric comorbidity (60.5%), and 43.2% had a comorbid mood disorder, significantly more than heterosexual women (28.5%). More than one-quarter of bisexual women who met criteria for a past-year alcohol use disorder also had PTSD (28.3%). Gay or lesbian women who met criteria for a past-year alcohol use disorder had a similar prevalence of psychiatric comorbidities overall (42.5%) and for each individual psychiatric comorbidity, compared with heterosexual women.
Tobacco Use Disorder and Psychiatric Comorbidities
Among those who met criteria for a past-year tobacco use disorder (N=7,303), 35.6% had a psychiatric comorbidity (mood, anxiety, or PTSD) (see Figure S2 in the online supplement). Psychiatric comorbidity prevalence was significantly higher for bisexual individuals (55.6%) than heterosexual individuals (34.9%) who met criteria for a past-year tobacco use disorder; this was true for each specific psychiatric comorbidity. Anxiety disorders were more prevalent among gay or lesbian individuals (28.3%) who met criteria for a past-year tobacco use disorder than among heterosexual individuals (20.4%).
Among men, about one-quarter (26.6%) of heterosexual individuals who met criteria for a past-year tobacco use disorder had a psychiatric comorbidity. There was a considerably higher prevalence of psychiatric comorbidities among bisexual men (39.9%) and gay men (44.1%) who met criteria for a past-year tobacco use disorder, but only significantly so for gay men. Anxiety disorders and mood disorders were significantly higher among gay men (28.0% and 29.5%, respectively) who met criteria for a past-year tobacco use disorder, while anxiety disorders and PTSD were higher among bisexual men (29.9% and 18.8%, respectively) compared with heterosexual men (14.5% and 5.6%, respectively) who met criteria for a past-year tobacco use disorder.
Among women, 45.7% of heterosexuals who met criteria for a past-year tobacco use disorder had a psychiatric comorbidity. Comorbidity prevalence for gay or lesbian women was similar (45.1%). Bisexual women had a significantly higher prevalence of psychiatric comorbidities (62.7%). Almost half of bisexual women who met criteria for a past-year tobacco use disorder had a mood disorder (45.1%), significantly more than heterosexual women (28.9%). Among those who met criteria for a past-year tobacco use disorder, bisexual women were also more likely to have PTSD (30.9%) compared with heterosexual women (13.2%).
Stress-Related Correlates of Past-Year Alcohol Use Disorder, Tobacco Use Disorder, and Psychiatric Comorbidities Among the Full Sample
We examined whether stress-related factors were associated with greater odds of each type of comorbidity while controlling for sociodemographic characteristics (
Table 2). We found that a greater number of stressful life events was associated with greater odds of each of the six types of comorbidities examined (adjusted odds ratios ranged from 1.30 to 1.43). Adverse childhood experiences were associated with all six types of comorbidities (adjusted odds ratios ranged from 1.08 to 1.19). Greater social support was associated with lower odds of five of the six comorbidities (adjusted odds ratios ranged from 0.96 to 0.98). Social support was not significantly associated with odds of alcohol use disorder and PTSD. We also tested for potential interactions of social support with stressful life events and with adverse childhood experiences and found minimal evidence that social support was a significant moderator (results not shown). Only one interaction was significant, such that for those with a greater number of stressful life events, social support was less protective than for those with fewer stressful life events (p=0.003).
Stress-Related Correlates of Past-Year Alcohol Use Disorder, Tobacco Use Disorder, and Psychiatric Comorbidities Among Sexual Minorities
Among sexual minorities (N=3,203), we examined whether stress-related factors were associated with greater odds of each type of psychiatric comorbidity while controlling for other sociodemographic characteristics (
Table 3). This included examining the additional stress-related factor of sexual orientation discrimination that was assessed only among sexual minorities. Greater frequency of sexual orientation discrimination was associated with greater odds of many psychiatric comorbidities examined, including alcohol use disorder and anxiety disorders (adjusted odds ratio=1.08; 95% CI=1.01, 1.15), alcohol use disorder and PTSD (adjusted odds ratio=1.10; 95% CI=1.03, 1.17), tobacco use disorder and anxiety disorders (adjusted odds ratio=1.09; 95% CI=1.02, 1.17), and tobacco use disorder and mood disorders (adjusted odds ratio=1.08; 95% CI=1.01, 1.15). A higher number of stressful life events in the past year was also positively associated with all comorbidities examined (significant adjusted odds ratios ranged from 1.25 to 1.43). A greater number of adverse childhood experiences was associated with all comorbidities except comorbid alcohol use disorder and anxiety (significant adjusted odds ratio=1.04–1.18). Greater social support was inversely associated only with tobacco use disorder and anxiety disorders (adjusted odds ratio=0.97; 95% CI=0.95, 0.99) and tobacco use disorder and mood disorders (adjusted odds ratio=0.96; 95% CI=0.94, 0.98).
Discussion
This study provides important information about alcohol use disorder, tobacco use disorder, and their psychiatric comorbidities among sexual minority populations. We found that sexual minorities have a higher prevalence of alcohol use disorder and tobacco use disorder psychiatric comorbidities than heterosexual individuals, a finding similar to that in work examining alcohol use disorder and PTSD (
9). Importantly, this finding was not simply driven by higher rates of alcohol use disorder and tobacco use disorder. Consistent with previous research, we found higher prevalences of psychiatric disorders among those who met criteria for a past-year alcohol use disorder and past-year tobacco use disorder, respectively. In addition, among sexual minority men and women who met criteria for an alcohol use disorder and tobacco use disorder, we found a greater co-occurrence of psychiatric disorders than among heterosexual individuals who met criteria for an alcohol use disorder and for a tobacco use disorder.
Consistent with research examining single disorders (
14,
29), we found variation in risk among sexual minorities by sexual identity and sex. Risk for psychiatric comorbidities was particularly high for bisexual women. In fact, well over half of bisexual women who met criteria for an alcohol or tobacco use disorder had a psychiatric comorbidity. Thus, it is important for clinicians to know that psychiatric comorbidities are more often present than not among sexual minorities who present with an alcohol or tobacco use disorder. Mental health screening is important for all individuals who present with an alcohol or tobacco use disorder, as different treatment strategies may be more effective for individuals with comorbid psychiatric disorders; mental health screening is particularly imperative for sexual minority individuals. We found the prevalence of PTSD among bisexual women with an alcohol or tobacco use disorder to be particularly high, which may point to underlying stressful and traumatic life events being important factors that drive higher comorbidity among sexual minorities overall and among bisexual women in particular.
In fact, our findings examining correlates suggest that experiences of sexual orientation discrimination and victimization have robust associations with comorbidities among sexual minorities. Sexual orientation discrimination, adverse childhood experiences, and recent stressful life events were each independently predictive of many alcohol use disorder and tobacco use disorder comorbidities. This is consistent with previous research that has shown these factors to be associated with single disorders. This finding also lends additional support to the minority stress model and highlights the importance of structural change that is needed to reduce discrimination and stressful experiences among sexual minorities to mitigate their health disparities (
26). Clinicians should be cognizant of the challenges faced by sexual minorities and should consider these factors as part of their initial assessment and treatment. Importantly, treatment environments should be affirming of sexual minority status. Clinicians should examine their policies and practices to ensure that they are not engaging in discriminatory practices.
Our study found that social support was protective, which is also consistent with the minority stress model (
33). More research is needed to identify the types and sources of social support that are most beneficial and how they can be incorporated into treatment, as this may be an important tool for building resilience. In addition, these results suggest that earlier prevention strategies for sexual minorities that incorporate social support may help reduce substance use and psychiatric disparities. We found minimal evidence that social support served as a buffer in the association of stressors and comorbidities; additional research that examines these associations longitudinally and using larger samples of sexual minorities is needed.
This study has some limitations. Because it was cross-sectional, we were not able to determine temporal ordering regarding minority stress correlates and the presence of substance use and psychiatric disorders. Longitudinal data would further elucidate the complex relationships between stress-related factors and comorbidities. The NESARC-III, which provided the data for this study, was conducted in 2012–2013. Given cultural and policy changes in the United States regarding sexual minorities, it is possible that more recent data could yield different results. However, recent studies among youths have shown that disparities related to substance use have persisted for sexual minorities through at least 2015 (
40). Still, it is critical to monitor these potential changes. This study may provide important baseline data with which to assess whether substance use and other psychiatric disorder disparities are improving or persisting for sexual minorities in the United States. Another limitation is the small sample size of sexual minorities, which did not allow for the examination of how these associations varied by sex and sexual identity. National studies that oversample sexual minorities, allowing for a more detailed look at risk and protective factors among this heterogeneous population, are needed. Finally, the NESARC-III data do not include information regarding gender identity, and thus we could not examine or control for this in our analysis.
In sum, we found that sexual minorities experience greater comorbidities compared with their heterosexual counterparts. Stressors are associated with greater comorbidities among all individuals, and stressors specific to sexual minority status, including sexual orientation discrimination, may contribute to comorbidities among sexual minorities. These additional stressors should be considered in the assessment and treatment of sexual minorities with substance use and other psychiatric disorders, as these comorbidities may pose heightened challenges in assessment, diagnosis, and treatment.