For decades, the heritability of common and debilitating psychiatric conditions, such as schizophrenia and bipolar spectrum illnesses, has been appreciated not just as evidence that there are specific molecular foundations of clinical neurobehavioral phenomena, but also as a promise that were these foundations to be identified and mechanistically understood, novel and life-changing targeted therapeutics would follow (
1). Increasingly large-scale genome-wide association efforts to identify common risk polymorphisms have made it clear that the clinical intricacies of psychiatric diagnoses are paralleled by genetic architectures that are complex, and despite accelerating innovation and accumulating findings, much of the path from genes to illness remains unknown. When available, a “genotype-first” approach (
2) can offer an important alternative with which to understand these complexities where molecular causality may be more easily inferred. In this approach, a selected study population might harbor a rare, well-characterized, and well-bounded genetic variant with an associated large phenotypic risk, such as is the case of many clinically apparent copy number variants (CNVs). A CNV is a type of genetic alteration in which an individual has fewer (i.e., deletion) or more (e.g., duplication, triplication, etc.) copies of a gene or set of genes as a result of nonallelic homologous recombination events introducing errors across a stretch of DNA during cell division.
One important example is the case of 22q11.2 deletion syndrome (22q11DS), a CNV associated with a host of multiorgan manifestations, where current efforts in this vein are largely rooted in a clinical observation nearly 30 years ago of markedly increased risk of schizophrenia (
3). This finding, later buttressed by larger-scale quantification (
4), has seeded field-wide interest and encouraged the growth of vigorous, multifaceted research initiatives aimed at understanding how hemideletion at this site on the long arm of chromosome 22 might confer neuropsychiatric disability. Advances along these lines from pooled neuroimaging data sets have begun to afford the field a more detailed view of the 22q11DS neurostructural landscape than previously available (
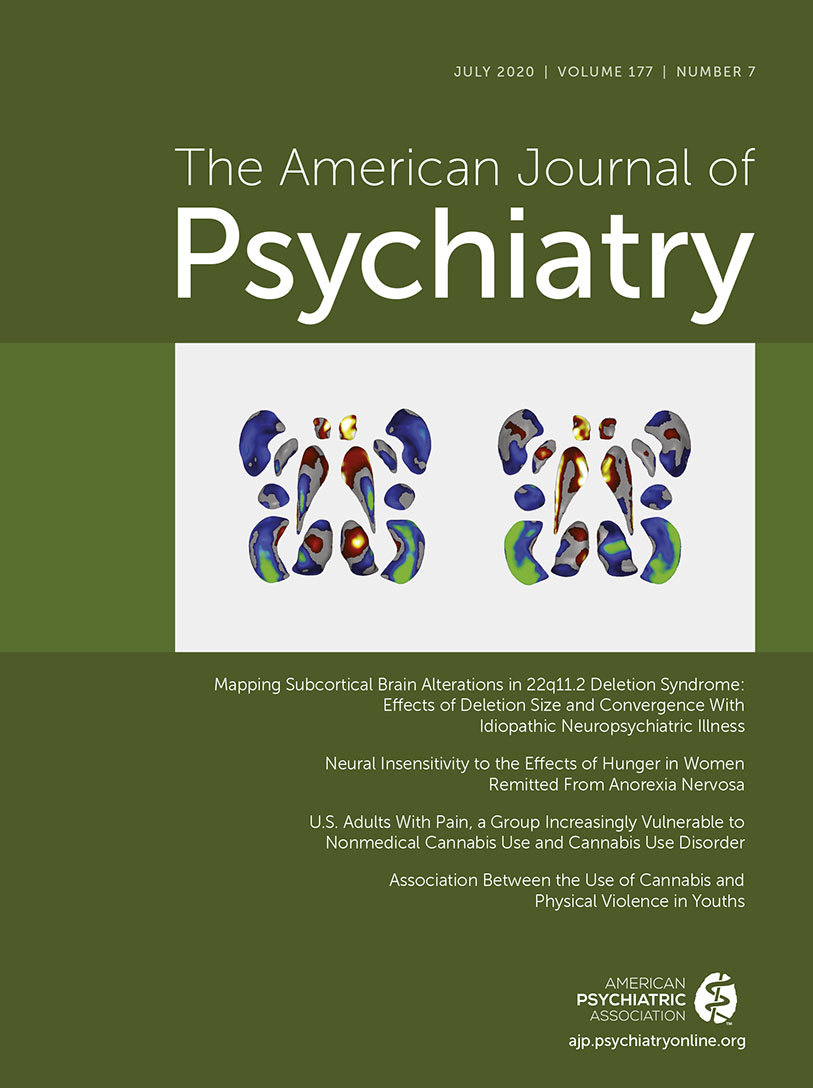
5,
6). Drawing from the largest 22q11DS multisite neuroimaging cohort assembled to date, in this issue of the
Journal Ching and colleagues (
6) illustrate this well by identifying robust subcortical structural patterns present in individuals with the deletion and by additionally reporting on within-cohort effects of psychosis and deletion size subgroups. This work offers important new insights and raises intriguing questions about the neurogenetic mechanisms underlying neuropsychiatric disease states both within and outside of copy number variation contexts.
In this study, reduced intracranial, thalamus, putamen, hippocampus, and amygdala volumes, along with increased lateral ventricle, caudate, and accumbens volumes, were identified in 22q11DS, with generally consistent but more complex (e.g., an anterior-posterior shift in local caudate thickness) shape analysis findings. Whereas overall lateral ventricle, thalamus, and medial temporal lobe structure findings align quite well with observations reported in idiopathic schizophrenia, the striatal findings differ. Because the typical 22q11.2 deletion includes multiple CNS-expressed genes and results in multiple neuropsychiatric outcomes aside from schizophrenia, this CNV would not necessarily be expected to result in a neuroanatomical profile identical to that found in non-CNV-associated schizophrenia. On the other hand, a framework for establishing the circumstances under which any phenotype concordances reflect meaningful shared mechanisms between 22q11DS psychosis and non-22q11DS psychosis merits explicit articulation. Because discovery of shared mechanisms is a fundamental goal of this brand of “genotype-first” molecular medicine approach, such a framework is critical, particularly when the studied genetic variation is incompletely penetrant or pleiotropic in its sequelae, as in the case of 22q11DS. In the special situation of characterizing the biology of such a variant and making homology inferences about the relevance of that biology when observed in other contexts (i.e., idiopathic illness), several principles merit consideration.
1. Phenotypic congruence.
The strength of such an inference may depend on how closely comparable the phenotype measurement is in the variant and idiopathic contexts. In this regard, the work of Ching et al. benefits from the technical similarities in structural data acquisition strategy and analytic approach between their 22q11DS investigation and that of previous Enhancing Neuroimaging Genetics Through Meta-Analysis (ENIGMA) schizophrenia working group studies. These consistencies in phenotype quantification bolster confidence in the ability to draw comparisons across these two distinct genetic settings. For composite measurements (e.g., multiple subcortical structural measurements) thought to represent a singular latent process, the degree of phenotype overlap (e.g., the portion of structural measurements showing concordant phenotypes) may be an important modifier.
2. Phenotypic specificity.
The degree to which an observed biological outcome is unlikely to occur by chance in other contexts may help support the plausibility of the inference. If the same phenotype is seen in multiple other diagnostic settings, then the occurrence of this same phenotype in the variant-of-interest population becomes less specific and less probative of a meaningful mechanistic homology. Toward this end, in reference to the work of Ching et al., the degree to which the pattern of subcortical structural abnormalities in schizophrenia constitutes a fingerprint-like profile becomes an important consideration. A review of ENIGMA findings across several diagnoses presented in the article suggests that although several entities, such as autism spectrum disorder and attention deficit hyperactivity disorder, show quite distinct phenotypes, there is some transdiagnostic overlap in the rank pattern of abnormalities in schizophrenia with selected other diagnoses, such as obsessive-compulsive disorder and major depressive disorder. Notably, however, the effect size of these patterns remains greatest in schizophrenia.
3. Phenotypic centrality.
The greater the proximity of the phenotype to the hypothesized core biology of the idiopathic disorder, the stronger the homology inference may be. Conversely, ensuring that the phenotype is not likely to be an epiphenomenon (i.e., the phenotype is not likely to be a secondary effect that is not related to the core biology) in either the variant or idiopathic contexts also provides greater inferential support. With respect to the former consideration, while much remains unknown about the core biology of psychosis, the brain regions found by Ching et al. to have altered macrostructure in 22q11DS are well known in the schizophrenia research literature. With respect to the latter consideration, Ching et al. take care to provide corroborative secondary analyses by controlling for antipsychotic medications, which previously have shown effects on subcortical volumes (
7). Notably, this endeavor can become complex in the case of multifaceted neurogenetic syndromes like 22q11DS, in which syndrome-associated systemic illness, such as congenital cardiac disease, can secondarily affect a studied phenotype (
8), potentially playing a confounding or, alternatively, mechanistically important role.
4. Phenotypic internal consistency.
If within the “genetics-first” variant cohort, the phenotype correlates with the expression of the illness trait of interest, this may provide additional substantiation for the homology inference. Notably, when Ching et al. examined differences between 22q11DS participants with and without psychosis, they found that, relative to the non-psychosis subgroup, the psychosis subgroup showed a profile of subcortical volumetric reductions (i.e., the hippocampus showing the greatest decrement, with the lateral ventricle, already enlarged in the overall cohort, and the pallidum showing the least) that closely mirrored the profile seen in idiopathic schizophrenia. This observation of phenotype internal consistency lends support to the contention that some elements of the biological correlates of psychosis in 22q11DS and idiopathic schizophrenia may be shared.
5. Shared phenotype correlates.
Inference is strengthened by corroborative ancillary biological data that show correspondence to observations in both variant and idiopathic contexts. For instance, a relevant biochemical or functional assay known to be associated with the phenotype in idiopathic illness might also show association with the given phenotype in the variant cohort, supporting the inference that the mechanisms underlying the common phenotype observation are comparable in both settings.
Although not exhaustive, the dimensions enumerated above provide a framework with which to examine whether phenotype-level evidence is suggestive of shared mechanisms of illness between the “genotype-first” cohort and idiopathic setting. Clearly, viewed through this lens, the report by Ching et al. has advanced the field’s knowledge of schizophrenia-relevant subcortical neurobiology in 22q11DS, and in so doing, it has introduced even more challenging questions for investigation. Future studies must identify and assess the biological predecessors of statistically robust neurostructural patterns in 22q11DS to ultimately develop meaningful biomarkers of illness and, potentially, treatment response. In part, this calls for longitudinal investigations to learn not only at what point in development these patterns might arise but also to what degree they are predictive of or follow psychosis progression. Additionally, further studies of individuals with 22q11DS are needed to examine how these patterns may be fueled by molecular factors within the typically deleted region (as suggested by the deletion length analyses in the Ching et al. study) or across the wider genome (as suggested by recent work linking cumulative polygenic idiopathic schizophrenia risk burden to the development of psychosis in 22q11DS [
9]). Integrated study of functional and cellular correlates of these findings as well as gene dosage effects through comparisons with individuals harboring 22q11.2 duplications may also refine our knowledge in this arena.
While it is clear that any opportunity to better understand the relevant neurobiology of individuals living with neuropsychiatric disease–associated rare genetic variants is invaluable, experimentation identifying risk mechanisms shared with idiopathic illness in these conditions can offer a uniquely privileged view into the complex neurobiology of common mental disorders such as schizophrenia.