Dissociation is a disconnection between a person’s thoughts, memories, feelings, actions, and sense of self (
1). Dissociative symptoms are associated with intrusions into awareness, cognition, and behavior, with accompanying deficits in continuity of subjective experience (
2). Multiple lines of evidence support a powerful relationship between dissociation and trauma, particularly early-life trauma and childhood maltreatment, and dissociation constitutes a distinct subtype of posttraumatic stress disorder (PTSD) (
3). Given the complexity of the underlying psychological phenomena, it has been a challenge to determine the neurobiological signatures of trauma-related dissociation.
A study reported in this issue by Lebois et al. (
4) has addressed this gap in our knowledge and uncovered a potential brain circuit mechanism underlying individual differences in dissociative symptoms in adults with early-life trauma and PTSD. Previous studies of trauma-related dissociation have focused on emotion centers in the brain and have reported that among patients with PTSD, individuals with dissociative symptoms exhibit greater amygdala functional connectivity (“synchronization”) with prefrontal cortex regions involved in emotion regulation, including the middle and medial frontal gyrus as well as the default mode network (DMN) (
5). A related study focusing on the periaqueductal gray, a brainstem nucleus involved in autonomic control and modulation of pain, found that dissociative, compared with nondissociative, PTSD patients exhibited greater functional connectivity with multiple parietal cortex regions (
6). Although the brain areas examined and the targets differ across the two studies, a common pattern that emerges here is one of hyperconnected subcortical-cortical pathways. While these studies capture dysfunction in emotion-related circuits associated with PTSD, what has been missing is a broader examination of brain networks associated with trauma-related dissociations.
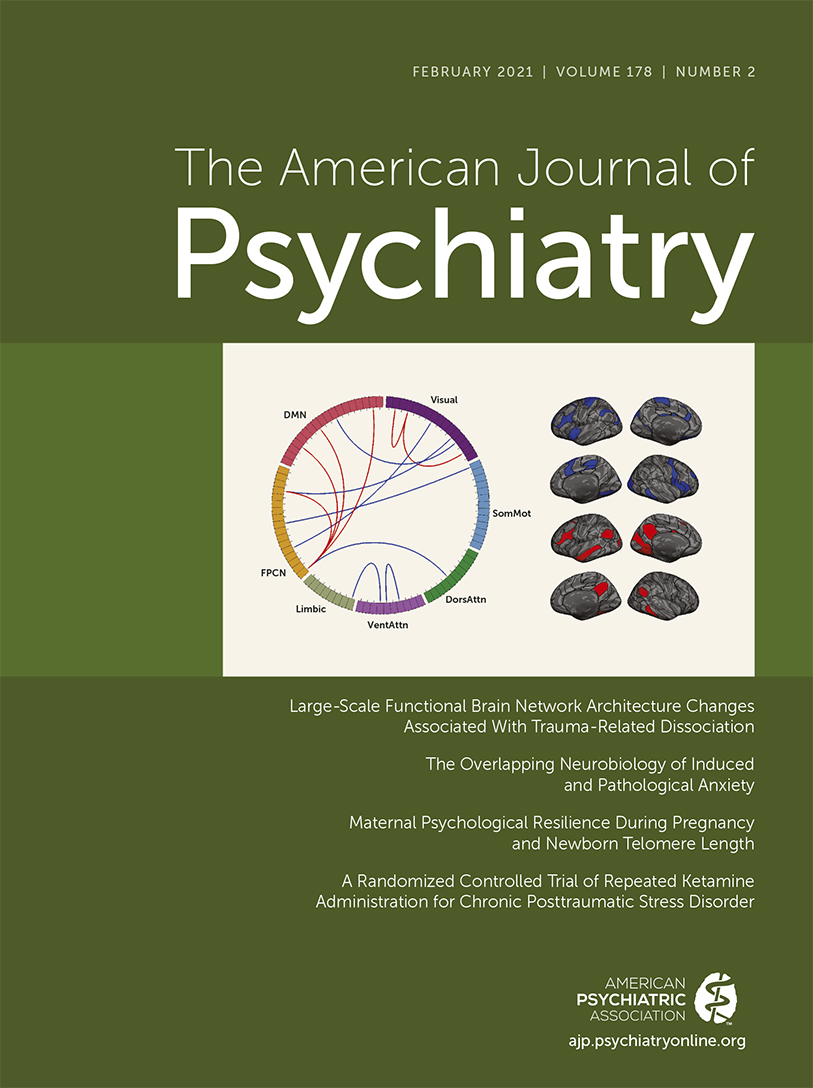
Lebois and colleagues used a dimensional approach to investigate continuous measures of trauma-related dissociation using the Multidimensional Inventory of Dissociation (
7) in a group of 65 women with histories of childhood abuse and current PTSD. Functional connectivity analysis was applied to resting-state functional MRI (fMRI) scans to investigate network dysfunction. The authors examined seven canonical brain networks, including the DMN, the fronto-parietal network (FPN), and the dorsal and ventral attention networks, and used connectivity measures with a cross-validation procedure to predict dissociation scores in a subset of individuals within the cohort. Internetwork connectivity measures predicted symptom scores reasonably well, with a correlation between predicted and actual scores of about 0.5. Connections that contributed most prominently to the estimation of dissociation scores involved the DMN and FPN. Furthermore, the most predictive links showed cross-network hyperconnectivity between the DMN and FPN, indicating that greater synchronization between these networks was associated with more severe dissociative symptoms.
The FPN and DMN serve different roles in human cognition. The FPN or “central executive” network, anchored in the dorsolateral prefrontal cortex and posterior parietal cortex, is critical for active maintenance and manipulation of information in working memory (
8). The DMN is anchored in anatomically distinct regions within the medial posterior cingulate cortex, ventromedial prefrontal cortex, medial temporal lobe, and angular gyrus (
8,
9). In contrast to the FPN, the DMN is typically suppressed during focused attention to external stimuli and is involved in cognitive processes that are internally focused, such as self-referential processing, recall of autobiographical events, rumination, and mind wandering. Both networks are fundamental to human cognition, and their dynamic interactions are critical for regulating adaptive goal-directed behaviors (
10). Moreover, tasks involving autobiographical planning coactivate the DMN and FPN, indicating a role in internally focused goal-directed cognition (
11). In this context, hyperconnectivity between the DMN and FPN in individuals with high levels of dissociation points to maladaptive integration and regulation of self-relevant internal mental processes.
An intriguing technical aspect of the Lebois et al. study is that the predictive signatures of trauma-related dissociations were significant only when homologous cortical regions were defined individually for each participant, but not when a canonical whole brain atlas was used. The authors employed a brain connectivity analysis approach in which cortical functional boundaries were defined at the individual level, prior to assessing connectivity between regions. This approach has demonstrated substantial improvements in the sensitivity and specificity of connectivity-based symptom prediction in other clinical domains, including schizophrenia (
12). Together, these studies suggest that incorporating individual-differences approaches to quantifying functional brain organization may be crucial for robust symptom prediction.
Despite the strength of the individual parcellation approach, the use of coarse brain network parcellations spanning just the cortical mantle is a limitation. At this scale, functional-anatomical precision is almost completely lacking, and thus an important avenue for future research will be to examine precise functional cortical and subcortical nodes associated with these networks and test theoretically informed models of psychopathology.
A clinical implication of Lebois and colleagues’ findings is that modification of aberrant hyperconnectivity between FPN and DMN may ameliorate dissociative symptoms. One possible mechanistic target for altering connectivity between these networks, suggested by the triple network model of psychopathology, involves the salience network (
13). The salience network, anchored in the anterior insula and anterior cingulate cortex, is crucial for “salience mapping,” that is, detecting salient external stimuli and internal mental events and facilitating engagement or disengagement of brain systems relevant for goal-relevant behaviors. The triple network model posits a central role for the salience network in modulating the degree of functional interactions between the FPN and DMN. Notably, the amygdala is a key subcortical node of the salience network, and hyperconnectivity of amygdala circuits has also been linked to the dissociation subtype of PTSD, as noted above. More targeted circuit analysis involving key nodes of the DMN, FPN, and salience networks, as well as the amygdala and hippocampus, rather than the gross cortical networks examined thus far, is required to determine precise targets for clinical treatment.
The findings of Lebois et al. are particularly relevant in the context of hypnosis, which is an effective adjunct to psychotherapy and pharmacological treatment of PTSD and dissociative disorders (
1). While hypnosis has proven clinical utility, the underlying circuit mechanisms are poorly understood. In healthy control subjects, hypnosis has been shown to reduce connectivity between the FPN and DMN and increase functional connectivity between the FPN and salience network (
14). Hypnosis may thus ameliorate the symptoms of trauma-related dissociations by reducing hyperconnectivity between the FPN and DMN. Restoring a balance in interactions between the FPN and DMN might contribute to diminution of the altered states of consciousness that characterize trauma-related dissociations (
15).
Remarkably, the authors’ findings are consistent with the view that trauma-related dissociations involve “recurrent, jarring, involuntary intrusions into executive functioning and sense of self” (
7). It appears to be paradoxical that hyperconnected brain networks may underlie the failure to adaptively integrate aspects of identity and consciousness. But perhaps it is not so paradoxical when we consider that what is rendered askew in dissociation is a stable balance between brain systems that encode different aspects of the human mental experience—the capacity for conscious control over thoughts and a system that engenders a sense of the self.
We are far from determining how the recurring mental thoughts arising from traumatic experiences intrude into executive functioning and self-referential systems. A challenge here, of course, is that resting-state fMRI does not directly capture the cognitive processes and functional events underlying circuit aberrations. Further studies with appropriate cognitive paradigms involving autobiographical planning, self-representations, psychological distance, and mind wandering, all of which engage the DMN, as well as paradigms tailored to individual experience, are needed to uncover trauma-related neurobiological processes. Conversely, the inability of the FPN to disengage from the DMN is a likely source of cognitive and executive function impairments in affected individuals, which can be probed using a wide range of tasks involving cognitive control (
16–
18).
Dissociation may be best conceptualized along a continuum from normal to pathological, with states of intense absorption, mind wandering, and severe dissociative disorders (
3). The dimensional approach used by Lebois et al. in trauma patients is broadly consistent with the National Institute of Mental Health’s Research Domain Criteria framework, although only a clinical cohort was used in their study. Further explorations along the dissociation continuum may explicate the generality of the findings and determine whether the neurobiological symptoms and dissociative symptoms are similar in other diagnostic groups. For example, the inability of the DMN to disconnect from the FPN and other cognitive control systems has been linked to positive symptoms in schizophrenia (
19) and more generally appears to be an emerging transdiagnostic theme in psychopathology (
20).
Finally, neurodevelopmental studies are needed to investigate the impact of early-life trauma, especially childhood maltreatment and sexual abuse, which are significant risk factors for dissociative disorders (
1–
3). Identification of aberrant functional circuits in childhood may contribute to the development of biomarkers that can serve as early treatment targets and reduce the negative lifetime consequences associated with a loss of a sense of self.