Stress and trauma are well known to be critical factors in the development and maintenance of psychopathology. In some stress-related disorders, such as anxiety and depression, stress can play an etiological role, whereas in other disorders like schizophrenia, stress can precipitate and exacerbate symptoms. Stress occurring early in life in the form of traumatic events is a transdiagnostic risk factor for developing psychopathology, whereas posttraumatic stress disorder (PTSD) is a disorder that is specifically defined as a maladaptive response to traumatic events. In the midst of the COVID-19 pandemic, and certainly to no one’s liking, we currently are involved in a naturalistic experiment linking stress to mental suffering and psychopathology.
Most of us have never experienced stressors of the magnitude and length associated with the global COVID-19 pandemic. Because the pandemic has been so prolonged, and in part as a way to cope, many of us have become inured to its catastrophic effects. It is mind boggling that we have begun to accept as commonplace the fact that 3,000 Americans per day are dying from COVID-19 or that the economic consequences are so dire that 16% of adults with children report not having sufficient food (
1). Although it may be obvious, it is important to enumerate why the COVID-19 pandemic represents the perfect storm of stressors and traumatic events:
1.
A long-term sense of uncertainty about the future coupled with a sense of uncontrollability.
2.
Concerns about contracting COVID-19, becoming gravely ill, and dying.
3.
Worries about losing loved ones and friends, and the grief associated with real losses.
4.
The trauma associated with being gravely ill with COVID-19.
5.
Prolonged physical separation and social isolation from family and friends.
6.
Disruption of regular routines, including work and school for children.
7.
Losses of jobs, business failures, and the profound economic consequences.
8.
Lack of trust in leadership to effectively deal with the crisis.
As mental health care providers, we are in the uniquely challenging position of both personally experiencing the disruptive influences of chronic stress associated with the pandemic and working with patients and other vulnerable individuals to mitigate the consequences of the stress and tragedies that they are experiencing. It is critical to underscore the need to provide additional resources to underprivileged and marginalized individuals, as they are particularly vulnerable to the direct and indirect consequences of the COVID-19 pandemic. For example, Black and Latino households are twice as likely as White households to experience food insufficiency during the pandemic.
The focus of this issue of the
Journal is highly relevant, as it provides new insights into the neural alterations associated with trauma, resilience, anxiety disorders, and PTSD as well as insights into new, promising treatment strategies. Dr. Yuval Neria, a PTSD expert from Columbia University, reviews neuroimaging findings in relation to PTSD and addresses how they may relate to the heterogeneity of PTSD symptom presentation and inform selective treatment approaches (
2). Dr. Yair Bar-Haim from Tel Aviv University and his colleagues present a thought-provoking commentary suggesting that symptoms associated with the intrusive reexperiencing of traumatic events should be prioritized as a focus of research efforts to elaborate mechanisms underlying responses to trauma and PTSD (
3). Dr. Dylan Gee and Paola Odriozola from Yale University coauthor a review that uses a translational neuroscience approach to discuss learning mechanisms relevant to the maladaptive regulation of fear and anxiety. In addition to considering conditioned fear learning and extinction, this review emphasizes the importance of safety signal learning, describes its underlying mechanisms, and speculates about the potential utility of using safety signal learning approaches in treating youths with anxiety disorders (
4).
Is Inducing Anxiety in Healthy Individuals a Valid Approach for Understanding Pathophysiological Processes in Patients With Anxiety Disorder?
Numerous studies in healthy individuals have used threat-related paradigms in combination with neuroimaging to characterize the neural correlates of adaptive anxiety responses. The findings from these studies have frequently been used to draw inferences about alterations in neural activation that are associated with maladaptive anxiety responses in individuals with anxiety disorders. Chavanne and Robinson focus on determining whether studying healthy individuals under conditions of threat is a valid approach for understanding brain processes relevant to psychopathology (
5). In their study, the authors first performed a meta-analysis on neuroimaging findings from studies in which patients with anxiety disorders were compared with control subjects when exposed to emotion-related paradigms. The results of this analysis were further compared with a meta-analysis of imaging findings assessing neural responses induced by unpredictable threat paradigms in healthy individuals. Across healthy individuals and those with anxiety disorders, increased activation was found in the insula, cingulate cortex, medial prefrontal cortex, and periaqueductal gray. There were also some differences between individuals with specific disorders and healthy control subjects. Similarities in neural activation between healthy individuals exposed to threat and individuals with anxiety disorders appeared to be greatest for individuals with specific phobias and were least similar for those with generalized anxiety disorder. In an editorial, Dr. Alexander Shackman from the University of Maryland and Dr. Andrew Fox from the University of California, Davis, discuss these findings in relation to the validity of using healthy subjects to understand pathophysiological processes in patients with anxiety disorders. They also point to additional work that needs to be done with animal models and humans to further develop an understanding of the mechanisms underlying pathological anxiety (
6).
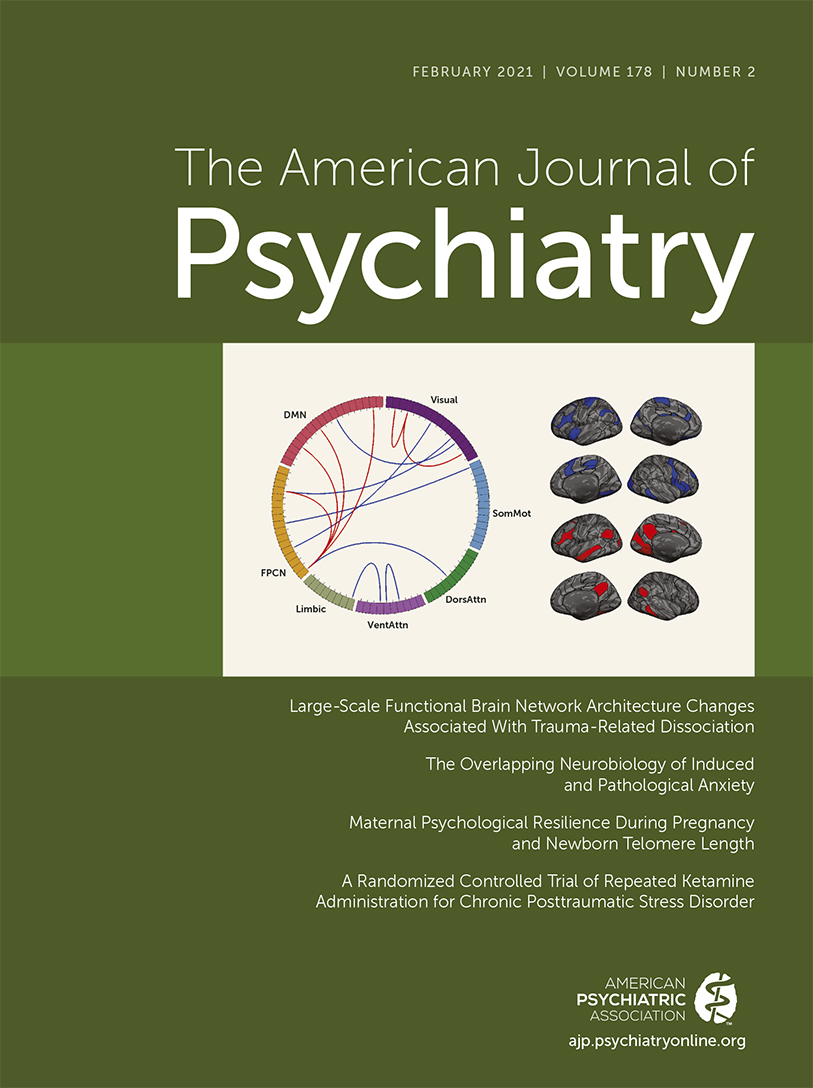
Using Brain Network Connectivity to Estimate the Severity of Dissociative Symptoms
Dissociative symptoms are a hallmark of PTSD and can be very disabling. The study by Lebois et al. (
7) presents data demonstrating the capacity to use machine learning with functional connectivity MRI data to modestly estimate individual differences in dissociative symptoms in women with PTSD. In their study involving 65 women, the authors demonstrated that they could estimate about 24% of the variance in an individual’s dissociative symptom severity by using the functional connectivity data. Hyperconnectivity between regions of the default mode network and the frontoparietal network appeared to contribute most to this prediction. Of importance, this brain network connectivity–based estimate controlled for childhood trauma and PTSD symptom severity, suggesting that the connectivity patterns identified to be associated with dissociative symptoms involved distinct neural alterations. In addition to providing a better understanding of the neural underpinnings of dissociative symptoms, the results of this study suggest that in the future it may be plausible to use brain-based neural connectivity measurements as an objective proxy for subjective reports of dissociative symptoms. In his insightful editorial, Dr. Vinod Menon from Stanford University discusses how the functions of the default mode network and frontoparietal network, and their interactions, may relate to the subjective experience of dissociation (
8). In addition, he suggests that interventions aimed at components of the salience network, such as the anterior cingulate cortex, may ameliorate dissociative symptoms by affecting interactions between the default mode and frontoparietal networks.
Patterns of Cortical Thinning Are Shared Across Individuals With Internalizing, Externalizing, and Thought Disorder–Related Symptoms
Brain structural alterations are commonly reported in patients across various psychiatric diagnoses. Romer and colleagues (
9) present data demonstrating overlapping patterns of reduced cortical thickness in individuals with internalizing symptoms (e.g., depression and anxiety), externalizing symptoms (e.g., substance abuse and antisocial behavior), and thought disorder–related symptoms (e.g., delusions and hallucinations). This study used structural imaging data to assess cortical thickness and cortical surface area from 45-year-old individuals who were part of the longitudinally studied Dunedin Cohort. In addition to demonstrating cortical thinning across diagnostic domains, patterns of cortical thinning were related to the general psychopathology dimensional score known as the
p factor. It is important to keep in mind that these relations do not address issues of causality. Based on these data, the authors argue that the transdiagnostic nature of pervasive cortical thinning further supports the value of a broad and general approach to study the relations between psychopathology and brain alterations.
Resilience During Pregnancy Is Associated With Increased Telomere Length in Newborns
Telomeres are strands of nucleotides at the ends of chromosomes that have various functions, including protecting the chromosome from degradation. In general, shortened telomeres have been associated with stress exposure, various illnesses, and aging. Verner and colleagues (
10) studied 656 mother-infant dyad pairs and, by using multiple behavioral measures collected during pregnancy, computed factors associated with stress and positivity. Telomere length was assessed in leukocytes collected from cord blood at birth. The findings demonstrate an association between individual differences in pregnant mothers’ stress factor and shorter telomere length in newborns. In contrast, individual differences in the positivity factor during pregnancy were associated with increased telomere length. By statistically accounting for the effects of positivity on stress, the authors derived what they considered to be a measure of resilience, and by using this measure, they demonstrate that maternal resilience is associated with increased telomere length in newborns. The findings from this study are exciting as they suggest that resilience during pregnancy has important implications at the cellular and molecular level for newborns and for their development. In her editorial, Dr. Stacy Drury from Tulane University further discusses the relevance of telomere length and function in relation to health and disease. She also presents possible mechanisms by which stress during pregnancy might affect offspring telomeres (
11).
Ketamine Treatment for PTSD
New and effective treatments are needed for patients with PTSD. Feder et al. (
12) report findings from a randomized clinical trial examining the effects of repeated intravenous ketamine infusions on symptoms in PTSD patients. Ketamine is an
N-methyl-
d-aspartate receptor antagonist with effects on numerous other systems, including opiate receptors, and when administered in subanesthetic doses, it is effective in rapidly decreasing depressive symptoms. The authors of the present study previously reported that a single dose of ketamine had positive short-term effects in PTSD patients, and they now extend this work by assessing the effects of repeated ketamine administration as a means to provide longer-term efficacy. In the study, 30 chronically ill PTSD patients were randomly assigned to receive, over a 2-week period, either six infusions of ketamine (0.5 mg/kg) or midazolam (0.045 mg/kg) as an active placebo. In the 29 individuals who completed the study, 15 received ketamine. The findings demonstrated rapid responses to ketamine. When assessed at 1 and 2 weeks, ketamine was significantly and robustly more effective in reducing symptoms compared with midazolam. It is important to note that although the repeated ketamine infusions were highly effective, the median time to the loss of the ketamine response was 27.5 days. In their editorial, Dr. Murray Stein from the University of California, San Diego, and Dr. Naomi Simon from New York University emphasize the need to develop more effective treatments for PTSD. They also comment on the renewed interest in psychedelic drugs as therapeutic agents and the possible mechanisms by which ketamine may work in relation to modifying the recall of traumatic memories associated with PTSD (
13).
Conclusions
The imperative to understand how stress and trauma increase the vulnerability to develop psychiatric illnesses could not be more relevant and timelier as the world’s population is experiencing unprecedented levels of stress, trauma, fear, anxiety, and grief. It is also extremely important to focus on, and understand, the factors that promote resilience, as we witness the remarkable capacities of individuals to endure, cope with, and overcome the adversity and challenges presented by the pandemic.
This issue of the Journal provides a comprehensive focus on new research findings relevant to these issues. Highlights from the reports in this issue include findings that there is evidence supporting the dimensionality of anxiety, as there is shared activation of anxiety-related neural circuitry between healthy individuals and those with anxiety disorders; that resilience during pregnancy is associated with greater “healthier” telomere length in newborns; that focusing on safety learning may be a fruitful treatment approach for anxiety disorders, especially for children; that machine learning methods can be employed with imaging data to predict the severity of dissociative symptoms in PTSD patients; and that repeated ketamine administration over a 2-week period robustly decreases PTSD symptoms.