Craving is a subjective experience characterized by intense desire or longing for something. Most people report having experienced a craving of some kind, be it for drugs or alcohol, specific foods such as chocolate, activities such as using smartphones or gaming, and even social interaction. Although craving can be a mobilizing force for achieving desired outcomes, it is also a central feature of disordered substance use and appetitive behavior, or collectively, addictive behavior. The clinical significance of craving cannot be overstated (
1). In recognition of its importance to the etiology and maintenance of addictive behavior, “craving” was added as a diagnostic criterion in DSM-5 for substance-related and addictive disorders. Further, the most recent meta-analytic data suggest large effect size associations prospectively linking craving to substance use and relapse (
2) and to eating and weight gain (
3), prompting the suggestion that craving should be assessed as early as in primary care for health prevention.
Despite the pervasive nature of craving and its clinical importance, craving remains poorly understood. Specifically, it is unclear how the phenomenology of craving may vary along the spectrum from “healthy” cravings to those experienced in the context of addictive behaviors. This limited understanding stems from a paucity of knowledge about the neural basis of the subjective experience of craving. While the neurobiology of craving has been studied for decades, with some notable exceptions (
4,
5), few studies have had the requisite sample sizes and methods needed to identify neural processes that reliably and generalizably relate to the experience of craving—that is, that are not only associated with but
predictive of this experience (
6). Statistical associations show how changes in one variable relate to changes in another in a given data set, but prediction requires that the association hold in new data that were not used to fit the model. Demonstrating predictive relationships, confirmed by cross-validation, is essential to establish clinical utility, prevent effect size inflation, and increase the generalizability of an identified model to novel individuals and settings. Such measurable and predictive neurobiological markers of craving could help inform treatments to mitigate craving, monitor treatment efficacy, and significantly advance theoretical understanding; they may be particularly valuable for individuals with low insight into their experiences, as well as for craving research in model systems where subjective experience is not accessible.
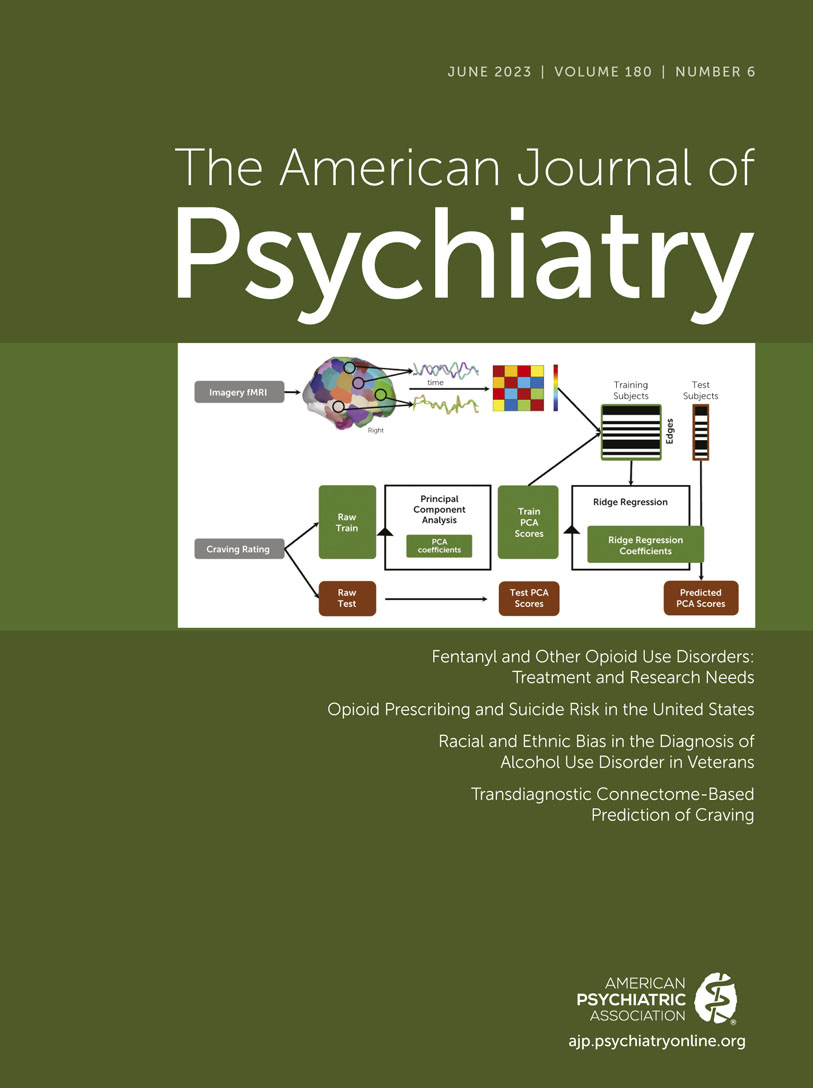
In this issue of the
Journal, Garrison and colleagues (
7) take a fresh approach to advancing this goal and derive a generalizable neural marker—a brain-based connectome predictive model (CPM)—that reliably captures subjective craving reports across individuals. Building on previous foundational work applying this state-of-the-science machine learning approach in addictive behaviors to predict abstinence (
8,
9), the study also shows the utility of CPM for subjective clinical phenomena, namely, craving. The authors pooled data from 274 adolescents and adults with varying health profiles (i.e., generally healthy, or using substances or prenatally exposed to substances, or obese) who underwent a functional MRI experiment designed to induce craving, stress, or a neutral-relaxing state. Personalized scripts were used to induce drug craving for people who used substances, or favorite-food craving for those who did not, allowing the authors to test for shared and unique CPMs between the two types of craving and based on disease relevance. Also unique to this study, the authors could evaluate specificity in the derived CPMs to craving versus other affective states, such as stress/anxiety. This is an important test, as one way that craving has been suggested to differ along the healthy to disordered spectrum is by its close interplay with negative affect. Using this rich data set, the authors built several predictive models (CPMs) from functional connectivity measured during the three experimental conditions. This involved first parcellating the brain into hundreds of nodes and computing the functional connectivity across those nodes. These connections (“edges”) were then combined in different ways to find those that together reliably related to subjective craving in different subsets of subjects (training “folds”) and that—across multiple model performance metrics and permutation testing—generalized to predict craving in testing (“held-out”) subjects using 10-fold cross-validation. The authors then went a step further to assess the generalizability of the best-performing CPMs. They tested their models not only in held-out data from their data set but also against an independent data set (
10) that employed a different craving provocation procedure (fasting and picture-cue viewing) and that had never been used to train the model. This provides a rigorous control to protect against the possibility of overfitting the CPMs to the specific experimental paradigm and setting of the present study.
Several intriguing findings emerged. First, the best-performing CPM could predict a person’s average craving with a correlation (r) of ∼0.4. While this represents a moderate effect size, the robustness and external validity of the identified relationships is noteworthy. There was no meaningful performance decrement when accounting for multiple nuisance variables, such as motion and physiological artifacts, and theoretically relevant ones, including gender, diagnosis, and anxiety. Age was an exception, in that controlling for age reduced model performance, but did not render it nonsignificant. Most remarkably, the derived CPM could predict craving with similar success in the independent data set that used a different stimulus and rating scale. These results are consistent with other recent findings using alternative models of craving based on patterns of brain activity rather than connectivity (
4), and they indicate that a person’s craving experience can be reliably inferred from a measurable biological process—here a complex pattern of functional connections—with moderate accuracy.
Second, drug craving reports in people who used substances could be cross-predicted from neural patterns of connectivity (i.e., CPMs) derived from models fitted to craving reports for favorite foods in the other groups, and vice versa (with r values ∼0.2–0.3); in turn, these models were specific to craving, as they could not predict an individual’s anxiety level. These data suggest that the neural signature of craving in people who use substances shares similarities with other types of craving, such as craving for favorite foods. Detailed dissection of the models indeed confirmed this by revealing high overlap in the nodes and edges contributing to the best-performing CPMs. These included the posterior cingulate cortex and hippocampus, which are part of the canonical default mode network, primary sensory cortices, and a subcortical network. However, the models derived were complex, comprising many thousands of edges, and perturbation of any of the networks that the most contributing edges belonged to, through virtual lesioning, did not eliminate the ability of the remaining edges and networks to predict craving. Thus, the identified “craving network” was highly distributed, and determining how it furthers our neurobiological understanding of craving may necessitate unpacking in future complementary experiments.
Third, in spite of the experiment inducing changes in craving reports, attempts to derive a model of these changes in craving were unsuccessful. By contrast, average craving (or the first principal component of craving ratings) could be predicted equally well by brain connectivity measured during any of the three conditions (craving, stress, neutral), albeit with some differences in the composition of the best-performing CPMs. Models derived from the stress condition had a stronger contribution of subcortical networks than those from the other two conditions. The finding that craving could be predicted from brain connectivity patterns measured in the absence of direct provocation may not be entirely surprising, given that the baseline organization of brain connections can prime and constrain responses evoked by a stimulus, including, in this case, cue exposure. Nevertheless, these data are particularly intriguing because they suggest that the derived CPMs capture stable person-level patterns, rather than within-person (state-dependent) patterns, which may contribute to their generalizability and value for predicting future craving outside the lab—which remains to be tested, as in other prospective studies (
8,
9)—but could possibly limit their applicability in tracking craving intensity and over time in individual subjects.
The study by Garrison and colleagues is a significant step in understanding how craving works in the brain, and it complements existing efforts leveraging other brain features and models (
4). Nonetheless, there remain some outstanding questions. Although there is much value to a generalizable model of craving across drug and favorite-food craving, there is also clear impetus to identify models specific to different types of craving when considering the potential clinical applicability of these models. For example, to better understand how treatments work, we need to know how well a treatment targets drug cravings while still allowing for other motivated behavior, such as cravings for food. Similarly, it will be informative to identify both differences and similarities between “healthy” cravings and pathological ones. The approach by Garrison and colleagues to study adolescents and people of diverse health behavior profiles is notable in this regard, but more work is warranted, as group membership effects could not be disentangled in the present study from effects of craving type. Second, although craving is by definition a time-limited experience, methods to identify mechanisms of craving remain cross-sectional and, to date, have not identified predictors of
changes in craving, including in the Garrison et al. study. Such models can complement population-level clinical studies by providing a means to track within-person craving over time, thus enhancing the ability to monitor treatment response and disease progression. Lastly, although cue reactivity is the current gold standard for studying the clinical neurobiology of craving, it is a limited depiction of the most clinically relevant aspects of craving, such as the “behavioral intent” component of craving. Thus, future studies may benefit not only from innovative analytic methods like CPM but also from complementary types of data and experimental designs that probe additional mechanisms of craving (e.g.,
11,
12).
This innovative study moves us closer to identifying objective, reliable, and generalizable brain bases underlying the subjective experience of craving. This has important implications for our understanding of craving and its treatment. Building on these findings, research examining the composition and functional relevance of the identified brain-based connectome model will be important for more precise neurobiological understanding of craving. Moreover, applying this model in the context of longitudinal research and more comprehensive interrogation of specific craving states will be key to determining its clinical utility. This new approach has the potential to revolutionize prevention and intervention efforts for addictive behaviors.