There is a critical need to identify objective predictive markers of treatment response in major depressive disorder (MDD), given the high levels of illness morbidity and the fact that two-thirds of individuals with the disorder fail to remit after first-line antidepressant treatment (
1). The promise of neuroimaging techniques to identify neural markers of pathophysiological processes associated with MDD has led to an increasing number of studies over the past two decades employing neuroimaging methodologies to identify neural marker predictors of treatment response (
2). These studies have had some success, with activity predominantly in prefrontal cortical-centered neural networks predicting antidepressant treatment response (
3–
5), and some studies showing that patterns of neural activity predict differential antidepressant response (
6). That said, there are limitations in the use of unimodal neuroimaging techniques in these studies, as this approach will not capture the wider range of abnormalities in neural network function and structure that is facilitated by the use of multimodal neuroimaging techniques, and will result in small effect sizes for predictor-response relationships in treatment response. Furthermore, combining clinical and neuroimaging measures in these studies can identify clusters of multimodal measures that reflect underlying patterns of neural network–behavior relationships that predict treatment response more accurately and with greater effect sizes than single-modality measures (
7). Yet, few studies have done this.
In the study by Poirot et al. in this issue of the
Journal (
8), the aim was to determine, in a large sample of individuals with MDD, whether response to sertraline, a commonly used antidepressant in the treatment of MDD, could be predicted before treatment or 1 week after the start of treatment, using a combination of neuroimaging and clinical data. In a preregistered study, the authors performed secondary analysis of data collected in the Establishing Moderators and Biosignatures of Antidepressant Response in Clinical Care (EMBARC) study. EMBARC was a double-blind placebo-controlled randomized clinical trial that included 296 adult outpatients across multiple centers who were unmedicated and had a diagnosis of recurrent or chronic MDD, in whom multimodal neuroimaging and clinical data were acquired before and after 1 week of treatment (
2,
9). EMBARC comprised two 8-week phases. In the first phase, participants were randomized to receive either sertraline or placebo. In the second phase, placebo nonresponders were treated with sertraline. All imaging modalities apart from diffusion MRI data were acquired at both the baseline and 1-week assessments. In the present study, the authors hypothesized that prediction of response to sertraline treatment using a multimodal approach would be significantly better than for placebo treatment, but similar to sertraline-treated placebo nonresponders. Furthermore, the multimodal approach was hypothesized to predict sertraline response significantly more accurately than using unimodal approaches.
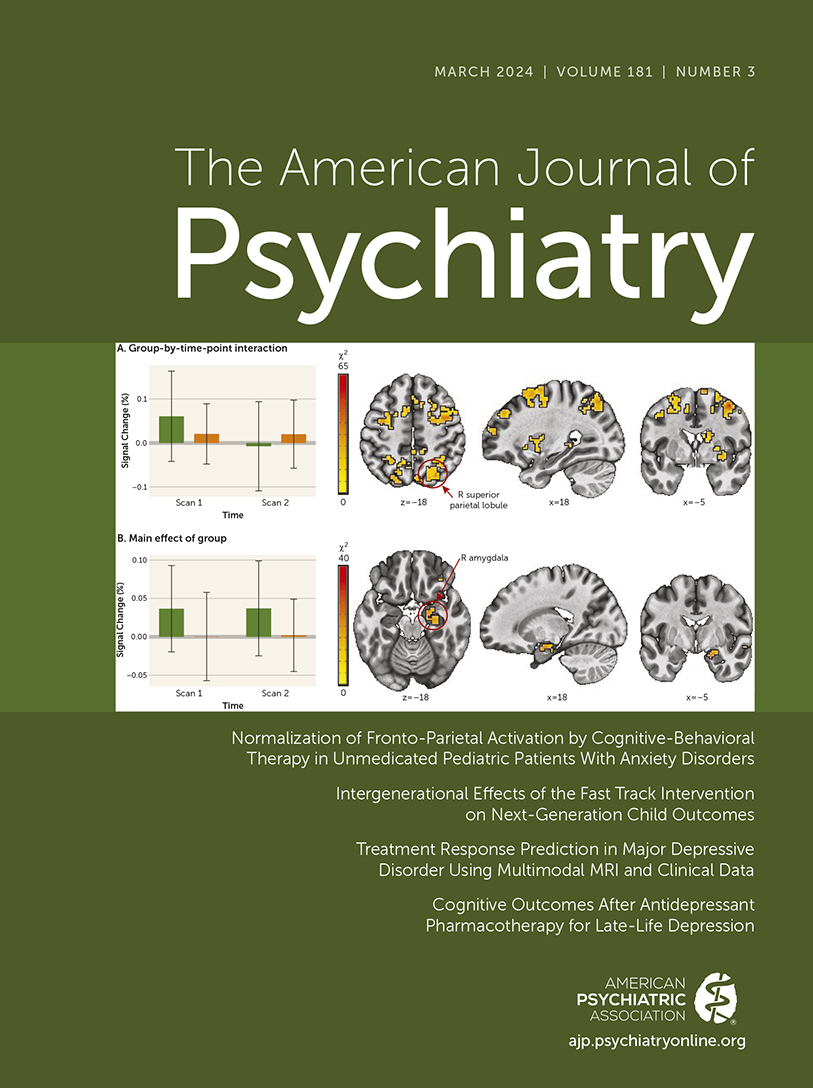
A total of 229 patients were included in the analyses (mean age, 38 years [SD=13]), of whom 151 (66%) were female. The authors employed machine learning with nested cross-validation to integrate multiple MRI modalities, including structural and diffusion MRI, resting-state MRI, and perfusion (arterial spin labeling) MRI, as well as clinical data. Treatment outcomes were treatment response, defined as a reduction ≥50% in depressive symptoms, measured using the Hamilton Depression Rating Scale (HAM-D) at 8 weeks, and remission, defined as a score ≤7 on the HAM-D at 8 weeks. MRI and clinical data were grouped into three tiers of predictors based on the evidence from meta-analyses and systematic reviews supporting the use of these measures as predictors. Here, tier 1 predictors included measures with the strongest evidence supporting their role as predictors of treatment response in depression. These were left and right hippocampal volumes, mean and standard deviation of frontal-limbic resting-state connectivity, and mean and standard deviation of regional cerebral blood flow in the anterior cingulate cortex, as well as age, sex, body mass index, illness chronicity, employment status, HAM-D score and relative HAM-D score reduction (from baseline to 1 week), anxiety and depressive scores on the Mood and Anxiety Symptom Questionnaire, and anhedonia severity as measured by the Snaith-Hamilton Pleasure Scale. Tier 2 predictors included 54 predictors across all modalities for which there was weaker evidence supporting their role as predictors of depression treatment response. Tier 3 predictors included all 240 predictors. In unimodal models, all predictors from other modalities were excluded from analyses. Mean balanced accuracy and area under the curve were the primary measures of analytic model performance in predicting treatment response and remission.
The authors found that of all the models, all tier 1 models best predicted sertraline treatment response, with treatment prediction better than chance, and that the best model performance was in the early-treatment prediction of response rather than in pretreatment prediction of treatment response. Interestingly, while cerebral perfusion measures were the best pretreatment predictors of treatment response, clinical measures were the best early-treatment predictors of treatment response, especially HAM-D symptom reduction from baseline to week 1, HAM-D symptom severity at week 1, and Mood and Anxiety Symptom Questionnaire anhedonic depression score at baseline. In support of the authors’ first hypothesis, models predicting sertraline treatment response largely performed significantly less accurately when predicting placebo response, although some models did perform well in placebo response prediction. Models predicting sertraline response in the first 8-week phase also predicted remission in the second 8-week phase among participants who were placebo nonresponders in the first 8-week phase and were subsequently treated with sertraline in the second 8-week phase. These models did less well in predicting sertraline response in the second 8-week phase in placebo nonresponders from the first 8-week phase, however. In support of the authors’ second hypothesis, multimodal models outperformed nearly all unimodal models.
Major strengths of the study were the inclusion of a large data set from an existing study, which was designed to allow comparison of predictors of sertraline response in participants initially treated with sertraline and participants initially treated with placebo who were subsequently switched to sertraline. There are some additional considerations for future studies aiming to adopt the approach used in this study, however, as the authors note. Clearly, replication of findings in independent samples is a necessary next step. There are also alternative approaches that could be used in treatment response prediction: for example, using continuous outcomes rather than cutoff clinical scores, focusing on patient subgroups defined by different dimensions of psychopathology in the context of MDD, and focusing more on treatment nonresponders in order to enhance our understanding of treatment-specific predictors. While the study used a large extant data set to identify combinations of measures that best predicted treatment response in MDD, the neuroimaging findings allow future studies to focus on the best neuroimaging predictors (i.e., some of the resting-state and cerebral perfusion measures) to examine in more detail the likely neural mechanisms underlying treatment response in MDD. A further consideration for such studies would be to use task-based neuroimaging data. In the present study, task-based data were excluded because of the practical challenges that acquiring such data poses to clinical application. Yet, it could also be argued that there are practical challenges in clinical practice in acquiring large amounts of neuroimaging data from participants, regardless of neuroimaging modality. Many functional MRI tasks are relatively straightforward to administer, and task-based data can provide important insights into context-dependent neural mechanisms that cannot be provided by structural, resting-state, and cerebral perfusion measures alone (
2). Lastly, it is intriguing that some models predicted placebo response and remission, suggesting that similar neural mechanisms may underlie response to SSRI antidepressants and placebo, as has been suggested by previous research (
10), although this needs further study.
The study makes a significant contribution to the literature by demonstrating that early sertraline treatment response is best predicted by a combination of neuroimaging and clinical measures rather than any single measure alone. Furthermore, these multimodal models predicted sertraline response more accurately than they did placebo response. As the authors point out, these multimodal findings can be used to help identify neuroimaging and clinical measures that can be used in clinical practice to identify individuals with MDD who are most likely to respond to sertraline, versus those who are less likely to respond to this treatment, and thereby advance the personalized medicine agenda in psychiatry.