Serious mental illness is an intriguing group of brain disorders, usually involving psychosis and often mania, where each conventional diagnosis has a weak knowledge base to support disease understanding and all have been highly resistant to disease discovery. While it is easy to say that we ought to base medication development on known neural defects, psychiatry has been very slow and clumsy at broadly implementing this strategy and, frankly, has not been effective enough at generating novel drugs for these disorders. There are beacons of hope, for sure, but too few. Furthermore, understanding the mechanisms of action of the medications we use in clinical care to treat people with poorly understood disorders is critical to physicians. The article in this issue by Moran et al. (
1) is one of those studies that teaches us new information important for conceptualizing serious mental illness and caring for individuals with these disorders. This paper teaches us things clinicians need to know to use amphetamines medicinally for attention deficit hyperactivity disorder (ADHD), autism, and depression—materially useful for clinical care and providing data potentially able to promote improved neural understanding to generate clinical leads. The paper reveals important outcomes that are jointly interesting for clinicians and researchers.
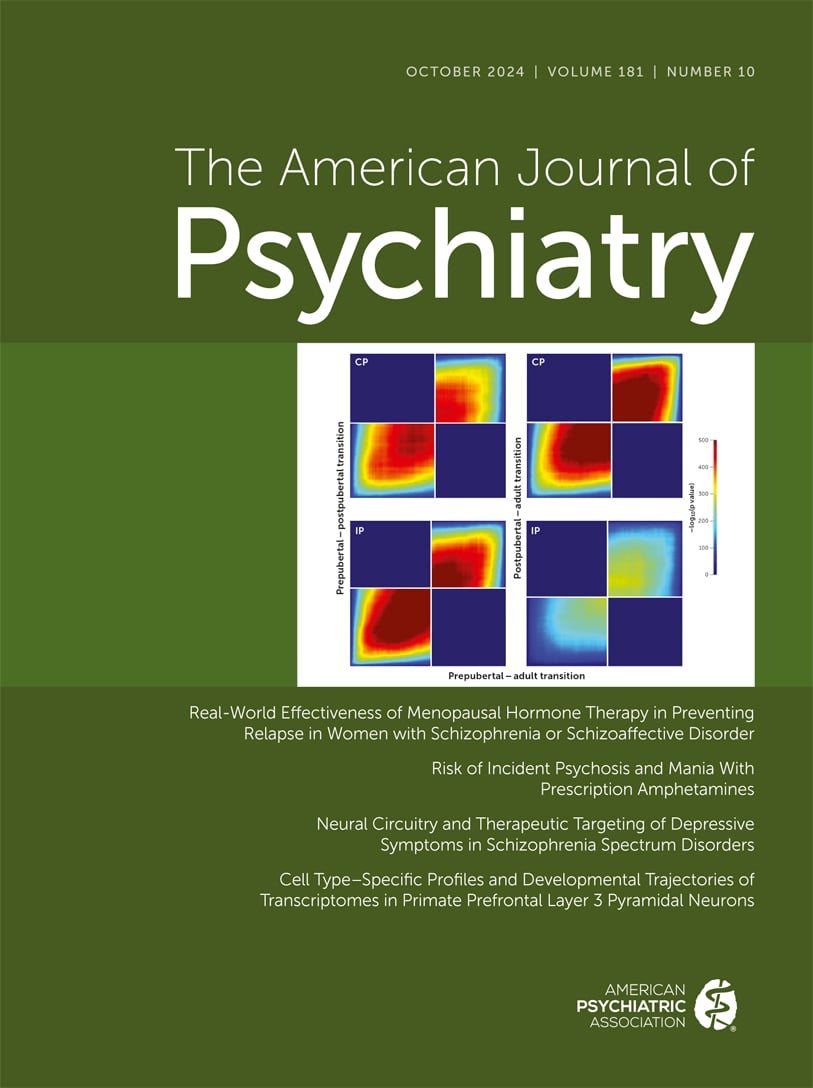
Moran et al. apply thoughtful methodologies to query the use of medicinal amphetamines in indicated disorders and to test what conditions result in psychosis and mania. They start by recognizing that the literature had already shown an increase in psychosis and mania with amphetamine treatment, but without dose threshold information for demonstrating risk. To answer the dose threshold question, they tapped the electronic medical record (EMR) database of the main admission unit at their hospital to gather pertinent clinical and disease targets queried at hospital admission. They were looking only for populations with first-time psychosis or mania who had prescriptions for amphetamine and had taken it in the month preceding hospital evaluation. The clinical evaluations were extensively similar and inclusive for all candidates in the admissions unit, done by the same work force, and with a similar focus. The authors specify their rules for the data collection and the decisions on cohort characteristics and EMR contents. The clinical information is wisely specified, with the data chosen related to the experimental questions of drug exposure (in workable dose ranges), the pertinent confounders for their question, risk calculations, and then the important considerations of missing data and of mitigating selection bias. The data analyses are clear and work through the characteristics of drug use important to interpretation. By the end of their process, the authors can support an answer to their questions to a remarkably strong degree, especially from data in an EMR database. And their answer is that the medicinal use of amphetamine has a significant effect on the generation of psychosis and mania, but they specify that this risk is most likely to occur if the dose is high (over 30 mg/day). These considerations help sharpen the answer to their question by pointing out how specific this relationship is, between amphetamine at a high dose and psychosis/mania outcomes. Doses under 30 mg/day can be used without a strong risk (i.e., only a small risk) of psychosis or mania; the authors are careful to say that this risk, although low, is significant because the loss of insight with psychosis makes its detection harder. Furthermore, methylphenidate use does not show any elevation of psychosis/mania in their hands, which is a critically important observation because of its widespread use in ADHD. Although dose levels are low in ADHD, long-term follow-up is uncommon. The authors calculate an attributable risk percentage of 81%, which suggests that if amphetamines do indeed have a causal relationship with psychosis/mania (which the authors acknowledge is only yet a mere association), stopping amphetamine use over 30 mg/day might well reduce these adverse outcomes by 81%. And amphetamine use here associated with psychosis and mania is not modified by other substance use, including cannabis and opioids. These analyses sharpen the final conclusion the authors articulate from their study, and they raise several additional questions, based on the data. Clinicians gain advantage by getting pithy and useful answers, allowing them to provide better care.
Research scientists are interested in the support these data provide for evaluation of the long-standing hypothesis that dopamine (and potentially other amine transmitters) is involved in generating clinical conditions like psychosis and mania. Of course, the concept that amphetamine has an adverse influence on psychosis/mania is a long-standing one with much support, including the dopamine hypothesis of schizophrenia (
2) and the role that dopamine antagonists have as the mainstay of psychosis/mania treatment (
3). Research studies document the release of dopamine with amphetamine from presynaptic elements in basal ganglia neurons (
4). While studies find significant associations with causality apparent, these studies do not show that all subjects have dopamine excess, nor have the same antipsychotic effects to usual dopamine antagonists. To reflect current broader etiological concepts of psychosis/mania, the confluence of increased dopamine release has been coupled with several additional putative risk factors, such as neurodevelopmental deviations and altered cortical excitatory/inhibitory firing in critical brain regions, which are being tested as etiologies (
5). Data show that multiple etiologies of serious mental illness provide plausible explanations for psychosis/mania outcomes, yet whether these multiple etiologies are cumulative within an individual, whether dopamine is an essential ingredient in generating psychosis/mania, or whether these putative etiologies are independent across populations are rarely ever discussed. These ideas taken together suggest a situation to which we do not give enough attention—that psychosis/mania appears to be etiologically heterogeneous and how this would happen. Can psychosis risk factors act independently within an individual to generate psychosis/mania? Can individuals with psychosis/mania have distinct etiological factors from each other? Are there common psychotomimetic risk factors which ought to define distinct psychotic disorders? There are biomarker studies that already show that biological measures can be used to cluster individuals into psychosis groups and can generate biologically homogeneous (clinically diverse) group characteristics (
6). Many studies in psychosis/mania look only for a unitary cause of schizophrenia or of bipolar disorder, not multiple features combined, nor multiple features spread out independently in individuals across a population. The heterogeneity of psychosis/mania outcomes begs for consideration that these and other serious mental illnesses represent syndromes that are etiologically diverse, perhaps resembling “fever.”
While the data reported here can clearly and extensively answer clinical questions, there are additional research questions that the data bring to the fore, which stimulate curiosity and suggest additional experiments. How can scientists follow up on the data reported here, focusing on these research questions? The kind of study done by Moran et al. suggests the value of going further in humans with a controlled prospective study using amphetamine at multiple dose levels to examine the psychosis/mania outcomes in control and affected patient groups. Such a study could further test the hypothesis that amphetamine generates an onset or a worsening of psychosis/mania symptoms, and identify in which subjects it might occur. This would test observational ideas from Moran et al. A study could construct the groups to represent the “potential confounders” analyzed in the study, using both symptomatic and biological outcomes. Such studies would certainly benefit from the use of sensitive methodologies currently available to the field in brain imaging, genetics, early abuse histories, and even detailed clinical features. Amphetamine is an old drug that never went through a full pharmacological characterization as a background for clinical application (
7). A focused pharmacological study based on the data from the Moran et al. study could suggest even more of its actions for clinical benefit and side effect mechanisms. Such studies could also help us understand the mechanisms not only of side effects but of treatments for its abuse potential as well.