Suicide prevention strategies have yet to comprehensively target structural racism as a mechanism that produces disparities in prevention and intervention pathways. Addressing how structural racism impacts youth suicide prevention is a critical priority, given that studies examining risk of suicide by age, gender, and race over time indicate suicide risk is highest earlier in life for ethnoracially minoritized populations (i.e., for youth of color [
1,
2]). Specifically, risk for suicide is highest in adolescence and young adulthood for Black, Asian/Pacific Islander, and American Indian individuals, in contrast to higher risk in middle age and later life for White individuals (
1,
2). At the same time, studies find lower rates of access to mental health services or delays in service access for youth of color at risk for suicidal thoughts and behaviors compared with their White peers (
3–
8).
The recent U.S. Surgeon General’s report on youth mental health includes “social and economic inequalities, discrimination, racism” as key factors shaping adolescent mental health. The report references research indicating that Black children ages 5–12 years old have nearly twice the rate of suicide as White youths the same age (
9,
10), which runs counter to the long-held perception that suicide rates are uniformly higher among White than Black individuals in the United States (
9). It should be noted that comparative estimates of suicide rates for children of this age are based on small sample sizes and therefore should be cautiously interpreted. Similar statements were made by the American Academy of Pediatrics and the American Foundation for Suicide Prevention in the recently released Blueprint for Youth Suicide Prevention which noted that “Youth have disparate opportunities and experiences in school and community settings, due to wide variation in social factors, community resources, and structural forces such as systemic racism and discrimination” (
11). Establishing a conceptual framework to organize the ways in which structural racism shapes the suicide prevention continuum may yield more effective approaches to address suicide risk among youth of color.
Variation by racial/ethnic group in youth suicide trends suggest that social, developmental, cultural, and ecological factors have an impact on suicide risk. Well-documented risk factors for suicide, which are typically utilized to identify targets for prevention, appear to be less reliable indicators among youth of color. For instance, only about a third of Black youth suicide decedents were in mental health treatment or had a documented mental health problem (
12)—considerably less than previous estimates showing that up to 90% of youth suicide decedents had a psychiatric disorder (
13)—which demonstrates a pattern that may extend to youths from other ethnoracially minoritized backgrounds (
14,
15). Among Black youth suicide decedents, behavioral disorders (not depression) were the most prevalent mental disorders, and hanging/suffocation (not firearms) was the most common method.
Rates of suicidal behaviors, the most reliable indicator of suicide risk, have also disproportionately increased among youth of color during the past two decades (
16,
17), although trends have also varied by subgroup. Latina girls have reported the highest rates of suicidal ideation and attempts for decades in the national Youth Risk Behavior Survey, while in the last two surveys the highest rates of attempts have been reported by Black girls (
18–
20). Although the majority of youth suicidal thoughts and behaviors are not fatal, they remain critical targets in suicide prevention. Considering that the majority of youth suicides occur in an initial attempt (
21), the window for prevention is narrow, thus highlighting the urgency in identification and early intervention among youth of color. Furthermore, an earlier onset age of suicidal thoughts and behaviors is prospectively associated with more severe psychopathology and poorer functioning across various domains in adulthood (
22).
These complexities emphasize the need to move from individual to structural explanations in suicide prevention efforts (
23,
24) and to account for dynamic interplays between systems and individuals over time. Youth are embedded in multiple ecological contexts (family, schools, neighborhoods), within which adverse conditions (e.g., family stress, reduced social support, economic disadvantage) can have an impact on risk for suicidal thoughts, behaviors, and deaths. Structural racism also fundamentally informs inequitable delivery of suicide prevention and intervention services that disproportionately harms youth of color. Thus, structural racism is a core mechanism producing adverse conditions that exacerbate subsequent group-level differences in both risk and resources to prevent risk.
Structural racism refers to racism that disadvantages people of color at the level of societal systems, which includes social structures, institutions, systems, ideologies, policies, and cultural forces that have an impact on both material opportunities and access to power (
25–
27). It is enacted via interconnected, mutually reinforcing systems and institutions with historical roots in the genocide and enslavement of Black and indigenous people (
28). As a result, micro-level interventions that address individual behavior in isolation, without addressing structural racism as a determinant of health, inevitably replicate systemic inequities (
26). Despite emerging attention to structural determinants of mental health, suicide prevention strategies have yet to comprehensively target structural racism as a mechanism producing disparities in suicide risk factors, protective factors, and intervention access and quality.
To this end, we propose a conceptual framework and overview of key, intersecting pathways by which structural racism causes and perpetuates disparities in suicide prevention for youth of color in the United States. In doing so, we note that the pathways and mechanisms we describe here are not an exhaustive overview of how structural racism impacts suicide risk and prevention. Rather, they are in-depth examples illustrating facets of the conceptual framework and an approach to understanding and analyzing how structural racism shapes the suicide prevention continuum. We also recognize that mental health and the suicide prevention continuum are shaped by multiple other structural inequities and experiences of marginalization based on gender, sexual orientation, ethnic/national identity, socioeconomic status, ability, and other aspects of social position. While these are not comprehensively addressed here, we view examination of these dimensions and their intersections to be essential future directions for the field. Our paper concludes with clinical, research, and organizational recommendations for antiracist suicide prevention.
The Structural Racism and Suicide Prevention Systems Framework
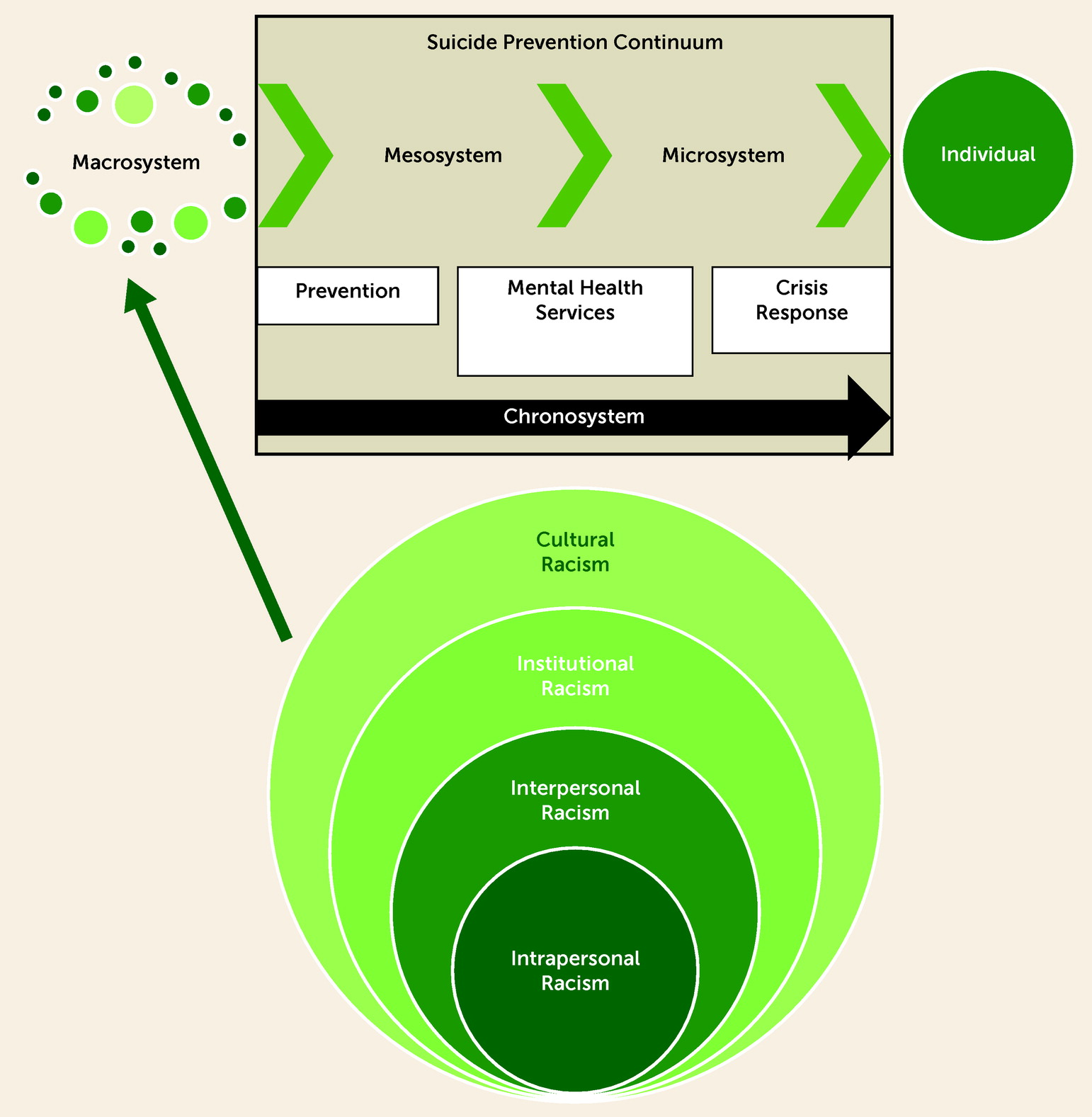
We propose a new framework, the Structural Racism and Suicide Prevention Systems Framework, depicting the impact of structural racism on the continuum of suicide prevention (see
Figure 1). This framework relies on an ecological systems perspective, which describes how individuals are embedded within social, political, and economic systems that shape behaviors and access to resources necessary to promote health (
23,
29). Within this framework, we argue that suicide prevention programming is affected by structural racism at multiple ecological levels. We provide examples to contextualize mechanisms by which structural racism 1) has an impact on mental health, including suicide risk; 2) circumscribes access to quality mental health services; and 3) has an impact on the continuum of suicide prevention.
We conceptualize structural racism in this framework as comprising the effects of racism occurring at four levels: cultural, institutional, interpersonal, and intrapersonal ([
27,
28,
30], see
Table 1 for definitions). Each level interacts with the others, from the broadest level of influence (i.e., cultural) to the narrowest (i.e., intrapersonal). We posit that together these four levels comprise the definition of structural racism as “the totality of ways in which societies foster [racial] discrimination” (
28,
31). Rooted in ecological systems theory (
29), we depict these four levels of racism as embedded in the macrosystem (i.e., broader society) in which we all live. The macrosystem structures institutions, allocates resources and opportunities, and carries out the effects of racism within the mesosystems (i.e., interrelations across settings) and microsystems (i.e., specific settings, such as families, schools, and neighborhoods). These systems interact with the chronosystem, which is the cumulative impact of the events, transitions, and circumstances over a person’s life. This dynamic interplay ultimately impacts an individual’s suicide-related risk factors, protective factors, and resources.
The ecological-developmental approach is consistent with theories of how racism impacts health, including mental health, via biological, social, and psychological pathways (including through racial inequality in socioeconomic status but also via multiple other independent mechanisms) (
32). Commonalities among these theories include focusing on ecological/structural perspectives, accounting for the impact of racism developmentally from the prenatal period through adulthood, and integrating stress and coping frameworks (
31,
33–
36). Recent studies also explicate the impact of race-based stress and trauma (i.e., traumatic stress reactions elicited by racial discrimination) on biopsychosocial outcomes among youth of color (
37–
39). Although the effects of racism culminate in adverse outcomes at the individual level, they cannot be explained or addressed via an individual-level focus alone.
Here we focus largely on the macrosystem level by interrogating how structural racism has an impact on the suicide prevention continuum (i.e., the processes of identification, referrals, treatment, and crisis response in the context of youth suicide). Structural racism not only has an impact on how services are delivered but is also codified into law, policy, and practices of policing and criminalization that affect suicide-related outcomes (
28,
40). Structural racism impacts health outcomes through multiple pathways, including residential segregation, health care access and quality, and discriminatory incarceration (
28). Youth suicide prevention takes place not only in health care settings but also in settings where youth services are provided (e.g., schools, child welfare, juvenile justice systems) and in systems of crisis response (e.g., police-led crisis intervention teams, hotlines, and psychiatric hospitalization). We highlight three key areas having an impact on suicide prevention, positing that critical attention must be paid to the intersections between mental health care services and broader suicide prevention programming. We focus on the intersections of systems, both to highlight where youth may be overlooked and to suggest intervention targets to mitigate the impact of structural racism at multiple levels.
Structural Racism at the Intersection of Systems
This section focuses on three key settings for suicide prevention in the United States, each of which is a critical opportunity to measure and mitigate structural racism: 1) outpatient mental health care services, or the primary site for suicide prevention; 2) schools, which present the best opportunity to reach the largest, most diverse proportion of youths; and 3) crisis response interventions, which typically involve the intersection of law enforcement, emergency services, and inpatient psychiatric settings. In
Table 1, we provide examples drawn from the following sections to illustrate how the Structural Racism and Suicide Prevention Systems Framework applies to each setting and how these examples in turn imply specific structural solutions.
Inequities in Service Pathways
Youth of color at risk for suicide are less likely to receive access to, or experience longer delays in accessing, mental health services than White youths (
3–
5), which can be explained by structural racism via mechanisms including income inequality and residential segregation. A key driver of disparities in mental health service access is the disproportionate shortage of child psychiatrists in low-income communities. Specifically, 70% of counties in the U.S., predominantly low-income communities, have no child psychiatrist (
41). This may result in limited opportunities for early prevention and intervention (i.e., before or immediately following the onset of suicidal thoughts and behaviors) that have better prognosis than late-stage intervention. Therefore, low-income families, who are disproportionately families of color, may need to rely on late-stage intervention in response to increased symptom severity. Indeed, a study examining racial and ethnic disparities in mental health and substance abuse care using a nationally representative data of medical expenditures from 2006 to 2012 found that youth of color, particularly those with internalizing problems, were less likely than White youths to receive mental health services via outpatient care, although no differences were detected in the use of inpatient or emergency psychiatric services (
42). This finding suggests that youth of color experience longer care delays and present with more severe symptoms, which makes them more vulnerable to coercive or punitive responses common in acute and crisis care. For instance, data from 11 emergency departments across the New England health care system from 2013 to 2020 indicated that visits for Black youths, compared with White youths, are more likely to result in physical restraint, a last resort measure used among youths at risk for harming themselves or others (
43). In a study of Medicaid-enrolled youths discharged from inpatient psychiatry care, Black youths were 0.82 times as likely as White youths to receive a 7-day follow-up, a key predictor of reduced risk of suicide in the first 6 months posthospitalization (
4).
Structural racism is also evident in the identification of mental health needs and subsequent treatment referrals for Black youths. Despite increased screening in primary care to address the underutilization of outpatient mental health services, a study of nearly 100,000 well visits shows that the likelihood of screening was higher among White adolescents as compared with Black and Asian adolescents, even though higher depression and suicidal thoughts and behaviors were observed among Black adolescents (
44). Compared with White youths, Black youths are less likely to be referred to mental health services within child welfare (
45) and juvenile justice systems (
46,
47). This information is especially concerning as Black youths and youths with psychiatric problems (
48), including suicidal behaviors (
49) are overrepresented in institutional settings. Referral disparities may reveal underlying racial biases among providers that may also coalesce in treatment decisions (e.g., use of physical restraint), although no research to date has examined this empirically. Nevertheless, a recent review of randomized control trials from 1963 to 2017 found associations between residing in a state with increased levels of cultural anti-Black racism and reduced psychotherapy efficacy for Black youths but not White youths (
50). These findings are striking and provide evidence that, even when accessing services, Black youths may not benefit equally in contexts with high cultural racism. Cultural racism is at the core of structural racism; it upholds racist ideologies that inform decisions, practices, and policies across multiple systems, including mental health care. Therefore, racial disparities create major barriers to quality care at every decision point along the suicide prevention continuum through which youth of color interface with potential gateways to mental health services. These barriers reflect structural racism and converge to increase vulnerability to suicide-related risk for youth of color.
School Discipline Pipelines and Practices
Efforts to expand mental health services in schools, including suicide risk screening tools developed for use in schools (
51), suicide prevention programs, and the expansion of school-based mental health clinics, could help address the unmet mental health needs of youth of color. However, structural racism limits the impact of school-based services, which, in turn, disproportionately disadvantages youth of color. To begin with, there is a critical shortage of mental health service professionals in schools. Although the National Association for School Psychologists recommends a ratio of one school psychologist per 500 students, the national average is 1:1,233, with some states reporting a ratio of 1:10,000 (
52,
53). This shortage creates a significant void in schools’ abilities to effectively respond to students’ emotional and behavioral needs. This void is compounded by the lack of diversity among school psychologists, since more than 80% are White, female, and monolingual (
52). This fact is especially concerning as behavioral problems are a robust indicator of youth suicide risk (
54,
55). At the same time, there has been a significant increase in police presence in schools with the expansion of school resource officer (SRO) programs tasked with violence prevention and safety promotion (
56). This change has translated into a “school-to-prison” pipeline whereby student behaviors are criminalized, resulting in increased arrests particularly among Black students (
57). SROs do not effectively reduce crime in schools (
58) and, instead, may increase stress for youth of color, who report feeling unsafe in schools where SROs are present (
59). These patterns are not surprising considering the racial disparities evident in community policing where people of color are disproportionately subjected to police violence (
60,
61).
Compounding the problem, Black students and students with disabilities (including mental disorders) are more likely to be suspended and expelled from school than White students or students without disabilities (
62), which leaves students of color with disabilities especially vulnerable. Other studies have demonstrated that 1) Black students received significantly more office disciplinary referrals than White students, even after controlling for teacher-rated behavior problems (
63), and 2) Black and American Indian youths received higher rates of punitive discipline than other racial/ethnic groups (
64). In fact, in a probability-based study of nearly 300 public middle and high schools nationwide, schools with a greater percentage of Black students were more likely to implement a zero-tolerance policy and more likely to use excessively punitive discipline techniques (
65). Racial bias may underlie these disparities, as a national study of 96,000 schools found that Black students were significantly more likely to be expelled, suspended, and arrested compared with White students in counties with greater anti-Black racial bias (
66). Such disruptions for Black youths limit their access to suicide prevention strategies available in schools (e.g., psychoeducation programs, gatekeeper training) (
67). Additionally, Black youths report lower school belongingness, less school equity, and greater adjustment problems in schools with greater racial disparities in disciplinary actions (
68). When youth of color with emotional and behavioral problems experience racial disparities in school disciplinary actions, there are at least two results: 1) they are disproportionately subjected to punitive disciplinary actions instead of compassion and care; and 2) they lose access to effective suicide prevention services that are available at schools. The barriers seen in schools replicate patterns observed in community-based suicide prevention services that yield delays or limit access to mental health care, which exacerbates symptoms and increases vulnerability to suicide-related risk. These outcomes are an example of how multiple systems interact to create inequities for ethnoracially minoritized youth.
The Crisis Care/Law Enforcement Interface
Another mechanism of structural racism in youth suicide prevention is our national reliance on carceral institutions (i.e., police, jail, involuntary hospitalization) as interventionist during times of acute suicidal crisis (
69). Law enforcement, emergency departments, and jails have become the de facto first line of response to youth suicidal behaviors (
70). Youths experiencing acute suicidal distress or their family members may call 911 during a crisis, or access other crisis supports (e.g., mobile crisis intervention, suicide prevention hotlines), which in turn, may involve law enforcement if there appears to be an imminent risk of suicide. Although some police departments have recently increased their number of training hours to intervene appropriately during emergency calls, a quarter of police-involved shooting deaths are related to mental health (
71). In police interventions that do not lead to death, people with mental illness are highly likely to be incarcerated at rates three to four times higher than the general population (
72).
In response to alarming rates of police violence against people with mental illness and people of color, police departments created specialty programs called crisis intervention teams (CITs). In over 2,700 jurisdictions in the United States, police are likely to respond to a psychiatric call by sending a CIT. Legacies of police violence against people with mental illness and people of color led to the creation of CITs in the late 1980s, through which officers attend a 40-hour training on mental health and are accompanied on psychiatric crisis calls by nonofficer mental health personnel (
70). The success of these programs led to the creation of youth CITs, adapted from the adult model to divert youths with mental illness from jails and refer them instead to psychiatric services and emergency departments (
73).
CITs have made a strong impact on police intervention. Officers trained in the CIT model are more likely to report verbal de-escalation or negotiation as their highest level of force utilization in response to mental health crises. CIT-trained officers are less likely to arrest people with mental illness (
74,
75) and more likely to transport individuals to psychiatric services rather than jail (
76,
77). Yet, three decades in, activists and scholars critique CITs as another carceral mechanism propagating harm against youth of color. The evidence is mixed as to whether CITs are effective at preventing police violence (
78,
79). The implicit concern about police intervention for youth of color at risk for suicide can be understood in the context of racial, age, and psychiatric disparities in police violence. Black men are 2.5 times as likely to be killed by police as White men (
80). Black women, American Indian/Alaska Native men and women, and Latino men all have a higher lifetime risk of being killed by police compared with their White peers (
80). Youths in a suicidal crisis are at increased risk since nearly 25% of people police killed in the last 7 years had a documented mental disorder (
81). As a result, youth of color, particularly those with mental health concerns, describe living in a “climate of fear” (
82), with police interactions potentially both a suicidal precipitant and a reason to avoid suicide crisis care.
Youth crisis interventions often lead to the youths in crisis engaging in either voluntary or involuntary emergency psychiatric services. Use of emergency services (i.e., psychiatric emergency department visits) have been steadily increasing in the last decade among youths, especially among youth of color. Between 2011 and 2015, for example, the United States saw a 28% overall increase from 31.3 to 40.2 youth per 1,000 interacting with emergency departments for psychiatric purposes (
83). The largest national increases were seen among Black (53%) and Latinx (91%) youths. In the same study, no significant changes in emergency department utilization were detected among White youths and only 37% of youths reporting a suicide attempt or self-injury were seen by a mental health professional during their visit (
83). This increase in emergency service utilization among youth of color suggests increased access to acute care yet also demonstrates overreliance on emergency services among youth of color. Involuntary intervention and hospitalization, while intended to save lives, creates a paradox for suicidal youths who report feeling criminalized, stigmatized, and marginalized when law enforcement initiate contact and transport them to hospitals (
84). In a study of youth encounters with police involvement in the emergency psychiatric setting, participants reported negative experiences of aggression, callousness, and nontherapeutic communication from officers (
85). Fear of crisis intervention, and thus inpatient hospitalization may be especially pronounced among youth of color. Indeed, Black adults who report negative interactions with police (
86) and Latinx youths who have experienced immigration raids and high rates of deportation in their communities (
87) are significantly more likely to report medical mistrust. Across studies, encounters with police during pathways to mental health care tend to be negative, with the most profoundly negative experiences among youth of color (
85). Given the disparities in use of force experienced by patients of color in involuntary psychiatry settings (
69), youth of color may endure suffering and manage suicidality on their own rather than engage with crisis responses that may lead to emergency/inpatient psychiatric care.
Implications for Antiracist Practice in Suicide Prevention
It is crucial to enact structural change to both reduce suicide rates among youth of color and to mitigate racial disparities in suicide prevention. Since structural racism in suicide prevention is enacted within and across systems, strategies for systemic change are therefore complex and multifaceted (
88). We propose that racial biases and prejudice must be addressed at all levels of these systems, with particular attention to multilevel interactions at which responsibility for maintaining the continuum of care belongs to more than one organizational entity. Suicide prevention often occurs in the interaction between entities. We utilize the Structural Racism and Suicide Prevention Systems Framework to illustrate strategies addressing racism at each of these macro, meso, and microsystem levels.
Structural Interventions to Address Structural Racism in Suicide and Suicide Prevention
Macro-level interventions range from shifting public policies to dismantling social and political determinants of suicide (
89). The need for such system-level approaches is reflected in documented associations between public policy and suicide rates by state in the United States (
90) as well as calls to measure and mitigate political determinants of suicide and racial disparities in suicide prevention (
89,
91). Mental health providers may view these efforts as outside the scope of their work but bring an important perspective to bear on system-level change. We argue that addressing problems as complex and societally rooted as structural racism and suicide prevention requires the integration of macro-level population health perspectives with expertise in microsystem-level mental health interventions.
Therefore, we propose that addressing structural racism in youth suicide prevention means advocating for reallocation in material resources to low-income communities and communities of color as a suicide prevention strategy. Relevant policy interventions include addressing residential segregation, narrowing the income gap, increasing entry to economic participation, and improving the quality of affordable health care (
92). Longitudinal data demonstrates lower state-level suicide rates between 1990 and 2000 for states with higher per capita public assistance expenditures (e.g., total transfer payments, medical benefits, and family assistance [
90]). These specific types of spending, and not overall state spending, were related to reducing suicide. To mitigate disparities and prevent deaths by suicide at a structural level, it is necessary to radically shift how material resources are allocated. Individual- and family-level interventions are crucial to reduce micro- and mesolevel disparities, yet even governmental bodies argue for the need to strengthen economic support (e.g., build household financial security, broaden medical coverage, and enact housing stabilization policies) to reduce national suicide rates (
93). Simply put, when we make life
materially livable for marginalized communities, youth of color may be less likely to die by suicide.
We emphasize that a key macro-level intervention to decrease disparities in the suicide prevention continuum is decoupling carceral systems from behavioral health care services. A major challenge ahead for the field of youth suicide prevention is to consider how to remake the crisis response systems such that the protection of youths’ lives is balanced with ethical considerations about how such systems have a disproportionate negative impact on marginalized youth. This challenge can be seen in the decision by telephone suicide hotlines as to whether to use or not use nonconsensual active rescue protocols (e.g., tracing callers’ Internet Protocol [IP] address or geolocation and sending police or psychiatric crisis response without a caller’s consent). Within the broader mental health field, options have been proposed for meaningful police-provider collaboration, including increased funding for youth CITs or mobile crisis response teams, minimizing the presence of armed officers at people’s homes after 911 calls, removing armed officers from hospital lobbies, and decreasing the use of force in psychiatric settings (
94,
95). Others have called for defunding, such as reappropriating police funds to community-led suicide crisis response, or abolition, such as ending force as a tool of psychiatric care. Youth safety must be central to any crisis response, yet systems must be changed to protect youth of color from criminalization and race-based trauma during times of crisis and recovery.
Research on Structural Inequity and Suicide Risk
In order to inform structural strategies, suicide research must take a structural perspective. Public health research, including suicide, has often overlooked the role of structural racism (
96,
97). The existing research, albeit scant, demonstrates that structural racism, as represented by economic inequity and residential segregation, is linked to suicide. Past studies have found evidence for higher suicide rates among young Black males in metropolitan areas where occupational and economic disparities between White and Black males were greater (
98) and in cities with the highest levels of disadvantage among Black males as measured by unemployment rate, education level, family income, and residential racial segregation (
99). Expanding research in this area, including identifying mechanisms of these effects, needs to be a key priority that can be informed by similar approaches to studying the influence of structural stigma among LGBTQ youths, who are at elevated risk for suicide and suicidal behaviors. Studies in this area have examined the impact of more supportive school climate and same-sex marriage policies in reducing suicidal ideation and attempts, thus demonstrating analytic strategies linking macro and mesolevel context to individual outcomes (
100–
102). An innovative recent study demonstrated that state-level structural racism and anti-LGBTQ policies, independently and jointly, were associated with suicide risk factors and suicidal behavior outcomes for Black but not White sexual minority youths (
103). Greater uptake and integration of sociological theory and methods into suicide research is necessary to address systems-level influences (
23,
24) as is developing innovative ways to measure structural racism and its correlates (
97).
Returning to our focus on the interactions between systems, we call for further research to understand how structural racism is enacted in these interactions, such as the pathway from school-based identification of suicide risk to the establishment of mental health services in the community, the gap between discharge from inpatient care and the establishment of outpatient mental health care, and the use of law enforcement as a referral network for emergency care. Within schools, we call for investigating the impact of SROs on suicide risk in youth of color, which may yield important information justifying the reallocating of funds from SROs to mental health providers. In terms of crisis care, given that police-led CITs are the national default in terms of crisis intervention, we recommend further mixed-methods investigations into how suicidal youth of color experience CITs. We also recommend examining how crisis response interventions in schools, at the community level, and within institutions of mental health care service provision (i.e., emergency department, inpatient psychiatry) can be enacted without law enforcement presence. Research characterizing service use disparities across the suicide prevention continuum is necessary to better plan both organizational and individual-level interventions as well as provide evidence for key mechanisms of these disparities.
At the level of mental health prevention and treatment research, we recommend building on advances in developing culturally and contextually grounded treatments (
104,
105), including testing the implementation of evidence-based practices within community mental health settings (
106) and centering community knowledge at the core of prevention research programs (
107,
108). Research in youth suicide is already a challenging endeavor in which few prevention and intervention strategies have demonstrated evidence of effectiveness. When the research is focused specifically on youth of color, these challenges are compounded by lack of diversity in the mental health field, the undervaluing of research approaches relevant to working with minoritized youths, and structural barriers limiting access to resources and funding (
109). These challenges are evidenced in the state of the youth suicide prevention literature, wherein randomized controlled trials for psychosocial treatments enroll majority White youths and rarely report on subgroup differences in treatment response (
110). As a result, major treatment gaps exist that can only be addressed by concurrent investment in research and implementation, balancing the urgency of preventing suicide with the importance of understanding what works and what approaches are preferred by individuals and communities. Identifying harmful or ineffective strategies for de-implementation should similarly be a focus of research.
Clinical Training and Interventions
Came and Griffith note that “systems are complex; but because they are people-made and people-run, they can be transformed” (
111). Thus, our next set of recommendations focuses on institutions and the people within them. We propose that suicide prevention initiatives should leverage the framework of structural competency, an approach to transforming systems, clinical care, and training focused on understanding individual health and mental health in the context of structural factors; intervening to address structural factors; and developing structural humility and connections to communities (
112–
114). In suicide prevention, this necessitates integration of public health, health equity, and medical perspectives.
It is also critical to train psychiatric providers to understand and intervene in the ways the field reifies structural racism. Although the impact of institutional racism on the field of psychiatry was broadly discussed over 50 years ago (
115–
117), it is only in recent years that formal published curricula addressing racism have been disseminated for psychiatry residency programs. These resources—one for psychiatry residents (
118) and one for child and adolescent psychiatry fellows (
119)—can be foundational resources for training along with an online continuing medical education program, Racism and Black Mental Health, disseminated via the American Psychiatric Association (
120).
Addressing Interpersonal Racism
Ultimately, only structural solutions can dismantle structural racism. Concurrently, addressing and mitigating the harms caused by racism is still necessary to improve the cultural responsiveness of youth suicide prevention and intervention strategies. Indeed, early indications of the role of structural racism on youth outcomes can be seen in studies examining racial discrimination. For instance, in community samples of adolescents, Black and Latinx youths report greater racial discrimination from adults than from peers (
121,
122). The former may reflect institutional-level racism as adults are positioned with greater power and authority over youths, while interactions with peers may reflect more interpersonal racism. Additionally, increased levels of interpersonal racial discrimination were associated with increases in suicidal ideation among Black and Latinx adolescents (
123,
124). This association is consistent with growing evidence showing the prospective relation between racial discrimination and mental health problems in youths, with earlier age of exposure and greater cumulative exposure associated with more symptom severity later in life (
125).
One strategy is to routinely address race-based stress and trauma among youth of color and their families as part of standard practice in clinical care. A family intervention grounded in racial socialization developed for use with Black families, whereby the caregiver-child dyad actively processes and prepares for racialized experiences, is one example (
126). The Radical Healing framework is another example in which communities of color are empowered to thrive in the face of structural racism by promoting collectivism, critical consciousness, radical hope, strength and resistance, and cultural authenticity and self-knowledge (
127). Gatekeeper models that are need-based, community-driven, and strength-oriented such as those involving the church and other faith-based communities offer an example of how existing suicide prevention strategies can be culturally and contextually adapted (
20,
128). Approaches developed to address racial stress and trauma could also be evaluated for crossover effects on prevention of suicidal behavior and suicide.
As the effects of structural racism are most evident on a collective level, so too should be the approach toward suicide prevention. Addressing structural racism in youth suicide prevention is a complex task that raises challenging questions about how systems and services are organized and how they can be reimagined. A broad analysis of structural racism at the intersection of systems demonstrates the necessity of identifying key pathways and mechanisms that produce inequality in suicide prevention and the urgency of advancing and testing solutions. Guiding principles for reimagining intersections between systems can include systems that are preventive, rather than reactive; restorative, rather than punitive; and community-driven, rather than externally imposed.