In the best of all worlds, pregnancy and the
postpartum period would be times of joy, contentment, and peace of mind. In the real world, pregnancy is not a protected state. Mild to moderate symptoms of depression are common. At any one time, 7.4%–11% of women are depressed in the first trimester, 8.9%–12.8% in the second trimester, and 8.5%–12% in the third (
1,
2). The prevalence of depression over the 40-week course of a pregnancy is 18.4% (12.7% for major depressive episodes) as opposed to 7%–9% in the general population (
2). In the postpartum period 10%–15% (
3) of women become depressed. One to 2 women per 1,000 develop a psychotic disorder. Indeed, the postpartum period is the time during which women are most likely be admitted for mental health problems.
Given these facts, most physicians will have to help a woman or couple decide how to manage a psychiatric disorder during pregnancy or the postpartum. The initial reaction will be to avoid any medication during these periods. If the depression is mild to moderate, it might be managed by psychotherapy (psychodynamic, interpersonal, or cognitive behavior therapy). In the case of more severe disorders, it is necessary to balance the risks of using medication with the risks of not treating the disorder. Depression, anxiety, or psychosis during pregnancy may result in failure to obtain prenatal care, poor eating, substance abuse, attempts to self-abort, or suicide attempts.
Pregnancy
Untreated depression or anxiety during pregnancy can have many negative consequences. In a controlled prospective investigation, Wisner et al. (
4) found a higher risk for preterm birth not only in infants exposed in utero to selective serotonin reuptake inhibitors (SSRIs) but also in those exposed to continuous untreated depression, thereby suggesting it is the depression that causes these problems rather than the medication. In a meta-analysis of studies of depression in pregnancy, Grote et al. (
5) found an increase in preterm birth (<37 weeks) and low birth weight (<2,500 g); the magnitude of the effects varied as a function of depression measurement, country location, and socioeconomic status. Therefore, depression in itself can result in lower birth weight and reduced length of gestation.
Acs et al. (
6) examined the presence of maternal panic disorder in cases of different congenital disorders compared with matched controls in the population-based Hungarian Case-Control Surveillance System of Congenital Abnormalities. They found a higher risk of cleft palate (with or without cleft lip) and multiple congenital abnormalities in untreated mothers who experienced panic disorder during the pregnancy. Hosseini et al. (
7) found that trait anxiety at the second and third trimesters predicted lower birth weight and shorter birth length. Anxiety reported in the third trimester predicted shortened gestational age. Therefore, untreated prenatal depression or anxiety is not beneficial for either the mother or baby.
Concerns about the effects of medication include whether they cause teratogenesis or a major congenital malformation (MCM), increase the risk of spontaneous abortion, interfere with labor, cause problems for the neonate, or create long-term problems for the child. Evaluating the risk of taking medication is not an easy task. To assess whether a medication taken during pregnancy is causing a problem, any defect must either have a distinctive pattern (such as the limb problems that occurred with thalidomide) or occur at a rate greater than 3%, the general rate of defects found in newborns. There are numerous studies of medication in pregnancy but many have a multitude of methodological problems. Owing to ethical issues, none meet the gold standard of randomized, placebo-controlled, double-blind, crossover trials. Many studies do not control for age of the patient, previous pregnancy loss, dosages or timing of administration, multiple drug use, or the use of street drugs. It is also difficult to differentiate between the effects of the medications versus the effects of the illness itself. Given these limitations, it is still necessary to make recommendations based on the accumulated information of the best available studies.
Risks of discontinuation of medication
This dilemma is further complicated by research into the risks of decompensation after discontinuation of medication to get pregnant. Cohen et al. (
8) found that women who continued psychotropic medication during pregnancy had a 26% chance of decompensating during pregnancy. Those women who discontinued medication had a 68% risk of becoming ill, 50% by the first trimester and 90% by the second trimester. Einarson et al. (
9) also found that 70.3% of women who discontinued their medication had adverse effects and one-third became suicidal. Viguera et al. (
10) looked at women who discontinued lithium. They found that rates of recurrence during the first 40 weeks for pregnant and nonpregnant women were similar (52% and 58%, respectively) versus 21% during the previous year while the women were still using the lithium. Of the pregnant women, 70% had a relapse postpartum versus 24% of the nonpregnant women during the corresponding time.
In contrast, Yonkers et al. (
11) found that failure to use or discontinue antidepressants during pregnancy did not attenuate the risk of a major depressive episode. Women with a history of four or more previous episodes were at higher risk independent of antidepressant use. Yonkers et al. noted that their subjects differed from those of Cohen et al. as these patients had characteristics suggestive of severe depressive illness. They also noted their study did not use blood testing to document antidepressant use. Both groups agreed that women with more severe depression should not discontinue antidepressant use during pregnancy.
Antidepressants
Studies have looked at a variety of antidepressants including tricyclic antidepressants (TCAs), SSRIs, serotonin-norepinephrine reuptake inhibitors (SNRIs), and monoamine oxidase inhibitors. This latter group is considered unsafe during pregnancy because of the risk of hypertensive crises. In addition, animal studies have shown an increased risk of teratogenesis.
Teratogenesis
TCAs are less often used in pregnancy because they may contribute to constipation and orthostatic hypotension. Kallen (
12) reviewed data from 1995 to 2007 on early gestational exposures and found an increased risk of cardiovascular problems with no pattern as well as a marginally increased odds ratio.
Einarson et al. (
13) prospectively collected information on 928 pregnant women taking antidepressants and 928 nonmedicated controls followed through pregnancy. Case subjects were taking a variety of medications including bupropion, citalopram, fluoxetine, paroxetine, escitalopram, mirtazapine, sertraline, venlafaxine, fluvoxamine, and nefazodone. They concluded that antidepressant use during the first trimester is not associated with an increased risk of teratogenesis. No specific drug was associated with an increased risk. This study supports earlier work that found no increase in MCMs with SSRIs (
14), venlafaxine (
15), trazodone (
16), or nefazodone (
16).
For newer antidepressants, less information is available. Bupropion has been associated with an increase in left outflow tract heart defects (
17). The observed risk in this study was very small, information from subjects was collected up to 2 years postpartum and exposure could not be verified (
18). Escitalopram does not appear to be associated with an increased risk of congenital defects (
19). There are no published studies of the safety of duloxetine in pregnancy.
Paroxetine deserves special mention. Studies such as those by Berard et al. (
20) and Bar-Oz et al. (
21), have associated its use with a significant increase in cardiac defects. Einarson et al. (
22) collected the outcome of 1,174 infants from eight services and found no increase in cardiac problems; they concluded that studies that show an increase are including minor, transient defects that resolve spontaneously. Malm et al. (
23) used national population-based registries in Finland to compare the offspring of women who were and were not prescribed antidepressants during pregnancy. They determined that use of paroxetine was associated with a 0.2% absolute risk increase in right ventricular outflow track defects. As a retrospective registry study, it was impossible to determine drug compliance or timing of exposure. The authors also noted a high rate of alcohol and smoking and use of other psychiatric drugs in pregnant women taking SSRIs. The large number of calculations performed and the small numbers in some of the groups being compared leaves room for the possibility that some of the associations are due to chance. Most importantly, because in the first year of life there is spontaneous resolution of 90% of ventricular septal defects, it is unclear whether this should be labeled as a MCM.
A very small study of use of St. John's wort showed no increased risk in pregnancy (
24). ω-3 fatty acids have well documented benefits for fetal and infant development. Studies of their use as antidepressants have yielded mixed results (
25). Of the three studies in postpartum women, two found the ω-3 fatty acids no better than placebo, but the third showed significant benefits with no harm to the woman or the fetus (
25). Because of these mixed results, although ω-fatty acids are safe in pregnancy, they cannot yet be recommended for treatment of perinatal depression.
S-Adenosyl-methionine has been found to be of benefit for major depressive disorders (
25). One study in postpartum women showed benefit over placebo, but there were methodological limitations (
25). There are no data on use in antenatal depression. There is no evidence of harm to the mother or the fetus. Further research is warranted.
Spontaneous abortion
There are conflicting reports of an increase in spontaneous abortion (SA) rates. A meta-analysis of studies of a wide variety of antidepressants found that women using antidepressants had a rate of 12.4% versus 8.7% in the controls (
26). This suggested a small but significant increase in rates. Einarson et al. (
27) prospectively compared two groups of women, one exposed and the other unexposed to antidepressants in utero. Rates of SA were 13% in the exposed group versus 8% in the control group. They concluded that antidepressant use in pregnancy resulted in a small but significant increase in SA risk. Women with a history of reproductive loss had an elevated risk.
Nakhai-Pour et al. (
28) used information from the Quebec Pregnancy Registry to study this connection. They found a rate of 5.5% in subjects using antidepressants versus 2.7% in controls. Their information about drug-taking during pregnancy was based only on the fact the subjects had filled at least one prescription; researchers were unable to confirm their use. It is also important to note that the general public rate of SA is said to be 12%–15%. No specific antidepressant has been found to have higher rates than others. It is not clear whether any perceived elevation in SA rates is due to the medication or the depression itself.
Labor
No difficulties during labor have been determined.
Effects on the neonate
Birth weight.
Ramos et al. (
29) reported an increase risk of small-for-gestational age (SGA) babies in women who took doses of venlafaxine lower than 150 mg/day; no effect was seen in women taking TCAs or SSRIs. Limitations of this study included the small number of women (only 5) who were taking venlafaxine and a failure to properly control for substance abuse and more severe illness. The fact that problems were found only with doses less than 150 mg suggests that the cause might be more severe or only partially treated depression. Suri et al. (
30) in a well-designed study did not find any adverse effect of antidepressant use during pregnancy on birth weight. Antidepressants used included SSRIs, SNRIs, nortriptyline, and bupropion. Einarson et al. (
31) also found a statistically significant increase in preterm births but no SGA.
Prematurity.
Suri et al. (
30) found that antidepressant use in pregnancy was associated with an increased risk of preterm birth. The effect also appeared to be dose-related. Although the differences from controls were statistically significant, the differences (38.5 weeks versus 39.4 weeks for depressed women not taking medication and 39.7 weeks for controls) were questionably of clinical significance.
Neonatal syndrome.
Moses-Kolko et al. (
32) reviewed the literature describing a syndrome that can be seen in the newborns of mothers who have taken antidepressants (SSRIs and SNRIs) during the third trimester. The overall risk ratio after exposure during the third trimester is 3.0. This syndrome, variously labeled as a “neonatal behavioral,” “neonatal adaptation,” or “neonatal withdrawal”, consists of increased muscle tone, tremulousness, jitteriness, and feeding and sleep problems as well as respiratory difficulties seen in 10%–30% of neonates. The majority of the infants experienced transient, mild effects that required only supportive care and spontaneously resolved by 2 weeks of age. A rare presentation includes seizures, dehydration, excessive weight loss, and hyperpyrexia. No deaths have been reported.
Warburton et al. (
33) used population health data to compare neonates born to women who did or did not take medication in the 2 weeks before their infant's birth. They concluded that if one controlled for maternal illness severity, reducing exposure to SSRIs in the 2 weeks before a delivery did not appear to have a significant clinical effect on improving neonatal health.
Persistent pulmonary hypertension of the newborn.
Chambers et al. (
34) identified an increase in the rate of persistent pulmonary hypertension of the newborn (PPHN), a serious but rare disorder, after third trimester use of SSRIs. Their study showed an odds ratio of 6.1. This study included only 14 case patient and 6 controls and relied on after-the-fact patient interviews and incomplete records. Of the case infants, 99.5% had no problems. Wilson et al. (
35) performed a case-control study of infants with PPHN from 2003 to 2009. They found that cesarean delivery before the onset of labor increased the risk for PPHN (odds ratio = 4.9), but there was no association with late-term use of SSRIs. In the four other studies that have looked at this condition, the case-control studies (
36,
37) found a small but significant increase, whereas the cohort studies did not (
38,
39). Occhiogrosso et al. (
40) reviewed the relationship between PPHN and SSRIs including PPHN pathophysiology, the role of serotonin and genetic risk factors, and the effects of SSRIs on pulmonary vasculature and concluded that is extremely difficult to differentiate the contribution of SSRIs from that of depression itself. Many of the risk factors for PPHN such as obesity, smoking, reduced length of gestation, and cesarean birth also are found more commonly in depressed women. At this time, evidence for an association between SSRI use in the last trimester and PPHN is very weak. This risk must be balanced against the known risks of untreated depression.
Long-term effects
In a methodologically sound prospective study, Nulman et al. (
41) followed mother-child pairs exposed throughout gestation to either tricyclic antidepressants or fluoxetine and a group of nondepressed pregnant women not taking any medication for up to 71 months postpartum. Neither medication affected the children's global IQ, language development, behavior IQ, or temperament during preschool and early school years. Maternal depression, however, did result in less cognitive and language achievement. Nulman et al. (
42) also reviewed other studies of the long-term cognitive effects on children whose mothers took antidepressants during pregnancy. Results on more than 1,000 children in different studies remain reassuring.
Croen et al. (
43) looked at the rates of autism in the children of mothers who had used antidepressants during pregnancy and found that exposure, especially during the first trimester, may modestly increase the risk of autism spectrum disorder. The actual number of cases found in women who had “exposure” to SSRIs during pregnancy was 15. “Exposure” was defined as having at least one prescription for an antidepressant in the year before the birth of a child. Usage was based on pharmacy records, and there was no verification that the mother had ever taken the medication. The study failed to control for prenatal maternal stress, burden of illness, or postpartum disorders, all of which might contribute to the risk of autism.
Children of mothers treated with bupropion during pregnancy have been said to have an increased risk of being diagnosed with attention deficit hyperactivity disorder (ADHD) (
18). This study is of questionable value because it required multiple statistical calculations and failed to find an association between ADHD and known risk factors.
Scenario 1
A 33-year-old married woman had a major depressive episode 3 months earlier. Sertraline 150 mg once daily was started, and she has felt well for 6 weeks. She continues to take this medication. She is thinking about getting pregnant again.
This woman is still in the recovery phase of her illness. It would be unwise to discontinue medication but, even if she continued her medication, she would be foolish to add the physiological and psychological stressors associated with pregnancy to her life at this time. Advise her to wait.
Scenario 2
A 33-year-old married woman experienced a major depressive episode 10 months ago. She responded well to sertraline 150 mg and has been symptom free for 8 ½ months. She wants to stop medication so she can get pregnant.
Given this information, one could consider discontinuing medication if•.
There was only one previous psychiatric illness.
•.
It occurred more than 9 months previously.
•.
It resolved quickly with medication.
•.
The patient has been functioning well for more than 6 months.
•.
There is no family history.
•.
There are no current stressors.
•.
The patient has good financial and emotional supports.
•.
The patient has good insight into her illness so she can recognize early signs of decompensation.
•.
The patient is cooperative with treatment and willing to restart medication if she becomes ill again.
Scenario 3
A woman with a history of recurrent depressions has been treated with SSRIs throughout pregnancy. As delivery comes closer, she wonders if she should discontinue her antidepressant medication to avoid problems for the neonate.
Advise against this. The neonatal adaptation syndrome that some babies experience tends to be mild and self-limiting. The neonatologist should be warned that the mother has been taking antidepressants to understand that supportive care may be necessary. The risks of PPHN are very small. Overall, the risk for the baby is much lower than the risk of the mother developing a postpartum illness if the medication is discontinued.
Antipsychotics
Of women with psychotic disorders, 60% become pregnant; often the pregnancy is unplanned or unwanted. Because women who are chronically psychotic are very vulnerable to sexual abuse, contraception should be discussed as part of good preventative health care.
Typical antipsychotics
Teratogenesis.
No increase in teratogenesis has been seen in women taking piperidyl phenothiazines (thioridazine), piperazines (fluphenazine and perphenazine), phenothiazines (chlorpromazine and promethazine), piperazine phenothiazines (trifluoperazine), butyrophenones (haloperidol), thioxanthenes (flupenthixol), dibenzoxazepines, or diphenylbutylpiperidines (
44).
Effects on the neonate.
Chlorpromazine, flupenthixol, and fluphenazine have all been associated with a risk of neonatal withdrawal and extrapyramidal signs that may last for weeks to months (
44). The use of promethazine in late pregnancy could induce respiratory distress in the newborn and impaired platelet aggregation in the mother and the newborn (
45). There have been some reports of drowsiness.
A perinatal syndrome has been described, consisting of respiratory distress, difficulty feeding, floppy infant syndrome, hypertonicity, sluggish primitive reflexes, extrapyramidal symptoms, tremor, abnormal movements, irritability, and agitation, rarely occurs, and generally resolves within days (
46).
Long-term effects.
IQs at age 4 were not found to be different in children exposed to antipsychotics during the first 4 months of pregnancy compared with those of children of controls (
47).
Atypical antipsychotics
Teratogenesis.
Limited information is available on clozapine, olanzapine, quetiapine, risperidone, aripiprazole, or ziprasidone. A study by the Motherisk Program found no increased risk of MCMs in women exposed to olanzapine, risperidone, quetiapine, and clozapine (
48). Aripiprazole and paliperidone (a metabolite of risperidone) are the newest atypical antipsychotics. Only a few case reports have been published but none of these have shown any MCMs.
There may, however, be an indirect risk; the use of atypical antipsychotics during pregnancy may lead to weight gain that, in turn, can increase the risk for neural tube defects, hypertension, and gestational diabetes (
49).
Effects on the neonate.
McKenna et al. (
48) found a rate of low birth weight of 10% of exposed babies as opposed to 2% of controls. Newport et al. (
50) found tendencies toward higher rates of low birth weight and neonatal intensive care admissions in infants exposed to olanzapine (
50). In contrast, Newham et al. (
51) found that infants exposed to atypical psychotics had a significantly higher risk of being large for gestational age than either controls or infants whose mothers had taken typical antipsychotics (
51). The weight gain and possible gestational diabetes induced by atypical antipsychotics increase the risk of macrosomia, hypoglycemia, shoulder dystocia, and associated birth injuries (
52).
Long-term effects.
None have been identified.
Scenario 4
A 28-year-old woman with a family history of schizophrenia develops a psychotic disorder at week 10 of gestation.
Psychosis puts the pregnant woman and fetus at particular risk because of the possibility of delusional beliefs. Use the lowest effective dose of an antipsychotic, given in divided doses. If an atypical antipsychotic is used, it is important to keep a close eye on weight gain and regularly assess glucose metabolism.
Mood stabilizers
Teratogenesis
Lithium.
Initial retrospective studies indicated that lithium use in pregnancy caused a 400-fold increase in Ebstein's anomaly, a tricuspid valve malformation (
53). Later analyses found a much lower rate of problems with a revised risk of 1 in 1,000 as opposed to 1 in 20,000 in the general population (
46). This risk is much lower than teratogenic risks from valproic acid. Lithium may be used in pregnancy. Because lithium completely equilibrates across the placenta, it is important to try to maintain the patient at the lowest effective dose and monitor levels throughout pregnancy. Doses should be lowered in the event of pregnancy complications such as preeclampsia or any abnormality in amniotic fluid volume that might predispose the fetus to lithium toxicity. Level II ultrasounds and fetal echocardiography should be done.
Valproic acid.
Valproic acid monotherapy during the first trimester (compared with women taking no antiepileptic medication) has been found to have a 2–7 times increased risk for atrial septal defect, hypospadias, cleft palate, polydactyly, and craniosynostosis and a 12–16 times risk for spina bifida (
54). These increases appear to be specific to valproic acid because, except for craniosynostosis, there is still a significant increase compared with that of women taking other antiepileptic drugs. Taking a high dose of folic acid before conception did not seem to lower the risk of these abnormalities (
55,
56), although it did seem to reduce the SA rate.
Lamotrigine.
Various pregnancy registries have concluded that the overall risk of MCMs associated with first trimester lamotrigine exposure is 2.2%, well within expected baseline rates (
57–
59). The North American Antiepileptic Drug Pregnancy Registry reported a relative risk for isolated oral clefts of 10.4 (
58). This finding was not confirmed in a survey of 3.9 million births from 19 registries (
60). Although the U.K. Registry reported an increase in MCMs at doses greater than 200 mg/day (
57), neither the International LTG Pregnancy Registry (
61) nor the Danish cohort study (
62) found a dose effect.
Carbamazepine.
Data from the EUROCAT Antiepileptic Study Database were examined. Jentink et al. (
63) found that overall the reported risk for MCM was 3.3%, only marginally higher than the normal 2%–3% risk in the general population. The risk of MCM is equal to or lower than that of any other antiepileptic drug (and considerably lower than valproic acid) so it can be used during pregnancy (
64).
Topiramate.
Data from the U.K. Epilepsy and Pregnancy Registry found that the risk of major congenital malformations was 5% in women exposed to topiramate monotherapy (
65). Risk of hypospadias was 5.1% and that of oral clefts was 2.2%. Risks of teratogenicity, prematurity, and SGA were not influenced by the dose of the medication. The North American Antiepileptic Drug Pregnancy Registry (
66) found that the relative risk of a major birth defect is 2.8 times higher than the risk for the population at large; this is higher than the risk for lamotrigine (1.3) but much lower than that for valproic acid.
Oxcarbazepine and gabapentin.
In the study by Molgaard-Nielsen and Hviid (
62), rates of MCMs were found to be only 2.8% with oxcarbazepine and 1.7% with gabapentin, although the analysis may have been underpowered.
Effects on the neonate
The North American Antiepileptic Drug Pregnancy Registry (
66) found that babies born to women who had taken lamotrigine or carbamazepine during pregnancy on average weighed 74 and 94 g less than controls. In contrast, the babies of women who had taken topiramate on average weighed 307 g less.
A review of the neonatal effects of carbamazepine (
67) found no increased risk of caesarian section, preeclampsia, or premature delivery.
The use of lithium in the third trimester has been associated with cardiac dysfunction, diabetes insipidus, hypothyroidism, low muscle tone, poor sucking, lethargy, hepatic abnormalities, and respiratory difficulties in the neonate (
68). These effects appear to be related to higher lithium concentrations at birth. All babies lose weight after birth, increasing the risk of toxicity. Suspending lithium therapy for 24–48 hours before delivery may prevent iatrogenic lithium toxicity and reduce the risk of complications.
Long-term effects
Lithium.
No long-term adverse physical or mental effects have been seen in children exposed to lithium in utero (
69).
Valproic acid.
Meador et al. (
70) also found a higher risk of impaired cognitive function in 3 year olds whose mothers had taken valproic acid when pregnant compared with those whose mothers took other antiepileptic drugs. The reduction in IQ points also appears to be dose dependent; a 700-mg increase in dosage was found to cause a 15.8 discrepancy in IQ (
71). Nadebaum et al. (
72) found that prenatal exposure was clinically and statistically related to significant language impairment in school-age children and higher doses in the first trimester correspond to lower language scores.
Carbamazepine.
Carbamazepine has not been found to impair IQ. Children exposed to in utero carbamazepine performed as well as nonexposed children (
71).
Lamotrigine.
No reduction in cognitive functioning has been found in 3 year olds who were exposed in utero (
70). An observational cohort study found no impairment of neurodevelopment in a lamotrigine-exposed group (
73).
Polytherapy.
In general, risks increase with the use of antiepileptic polytherapy versus monotherapy. Adolescents whose mothers had received polytherapy during pregnancy had significantly lower IQs and were 6 times more likely to have learning disabilities (
74). Hunt et al. (
65) found that when topiramate was combined with other antiepileptic drugs, especially valproic acid, the risks of MCM increase to 9% (
65). Holmes et al. (
75) concluded that the risk of malformation in children exposed to lamotrigine or carbamazepine as polytherapy only increased versus monotherapy when valproic acid was added (
75).
Scenario 5
A 28-year-old woman has a history of bipolar disorder with several episodes of both mania and depression. Her disorder has been well controlled for 2 years with valproic acid. She wishes advice on medication in pregnancy.
Valproic acid represents a real risk of teratogenesis during the pregnancy. If possible, the woman should be switched to lamotrigine, lithium, or carbamazepine. If it is impossible to stabilize her disorder on a new medication, give folic acid 4 mg/day beginning before conception and continuing through the delivery.
Minor tranquilizers
Teratogenesis
The use of benzodiazepines, especially diazepam, had been associated with an increase in cleft palate. A meta-analysis of 13 cohort studies found no association between fetal exposure and the occurrence of MCMs, whereas data from case-control studies did show an increase in major malformations, especially cleft lip (
76). The conclusion was that any increase was marginally significant and of uncertain reliability.
There is little human reproductive data on lorazepam. A small prospective study by Ornoy et al. (
77) found no increase in MCMs. Information on 542 case subjects collected prospectively found no association between in utero exposure to alprazolam and the occurrence of MCM (
78).
Clonazepam is similar to diazepam. In a large prospective study, no association was found between use in pregnancy and the occurrence of cleft palate (
79). Data on triazolam are limited to manufacturer's data and a retrospective study on 138 women exposed in the first trimester; neither showed any significant increase in malformations or pattern to these malformations (
80), although withdrawal symptoms have been noted (
81,
82). No increase in MCM has been found in one limited retrospective study of flurazepam.
During labor
Heavy doses of long-acting benzodiazepines may cause sedation in the newborn.
Effects on the neonate
Withdrawal syndromes may be seen after use of clonazepam, alprazolam, and lorazepam. Lorazepam used in late pregnancy may lead to respiratory distress, decreased Apgar scores, problems with temperature regulation, and poor feeding (
83).
Other psychotropic medications
Zopiclone
Zopiclone is a short-acting hypnotic. A prospective, observational cohort study of women who had taken this during pregnancy found no differences between case patients and controls in outcome of pregnancy, delivery mode, fetal distress, presence of meconium at birth, preterm deliveries, or neonatal intensive care admissions (
84).
Zolpidem
Wang et al. (
85) conducted a population-based study in Taiwan comparing rates of adverse pregnancy outcomes between mothers who received zolpidem during pregnancy and those who did not. The zolpidem-exposed women had higher rates of adverse pregnancy outcomes, including lower birth weight (adjusted odds ratio = 1.39), preterm delivery (odds ratio = 1.49), SGA babies (odds ratio = 1.34), and were more likely to have a cesarean section (odds ratio = 1.74). There was no observed increase in congenital anomalies in the exposed group. The risk of adverse pregnancy outcomes was the highest in women who took zolpidem for more than 90 days. The authors did not account for the effects of anxiety/depression during pregnancy or the severity of the insomnia.
Methylphenidate
Data on use of methylphenidate during pregnancy are very limited. The available data do not suggest teratogenicity, but caution should be used (
86).
Dextroamphetamine
Studies of illicit use of amphetamines have found low birth weight, prematurity, and maternal and fetal morbidity (
87). The effects, however, may be confounded by the use of alcohol and other drugs. A large cohort study that monitored 50,282 women with medication use during pregnancy found that the standardized risk was 1.08, indicating no increased risk of malformations (
88).
Food and Drug Administration rating system
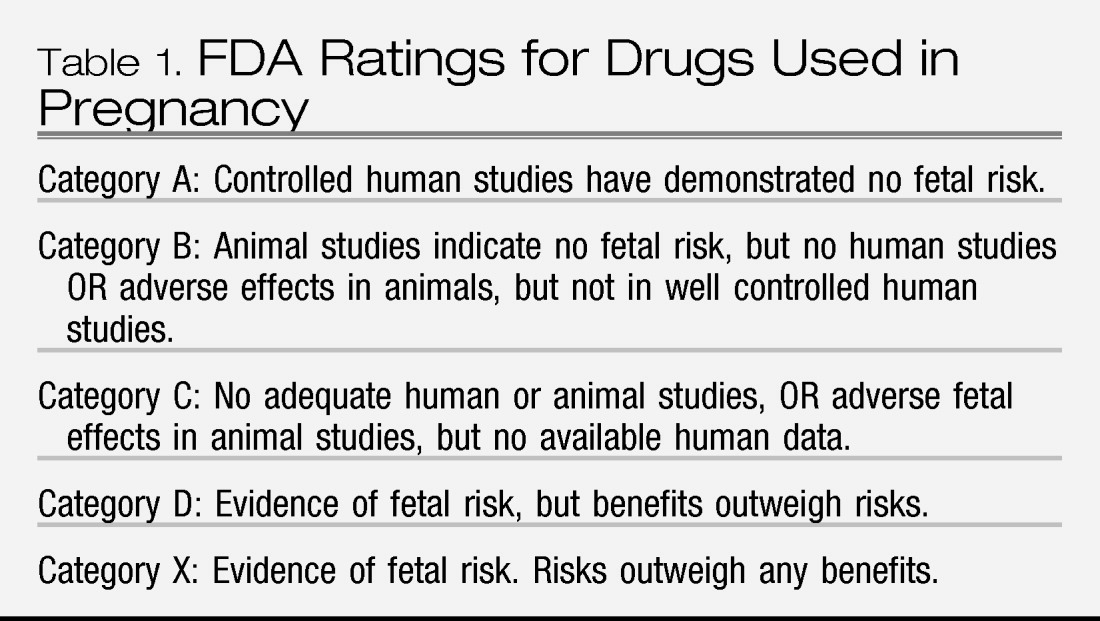
In 1979, the Food and Drug Administration (FDA) established a rating system to categorize the potential risk to the fetus of drugs taken during pregnancy (
Table 1). Fluoxetine, desipramine, phenelzine, sertraline, trazodone, nefazodone, venlafaxine, bupropion, and mirtazapine are classified in pregnancy category C, no adequate human or animal studies. Paroxetine, amitriptyline, imipramine, and nortriptyline are classified by the FDA in Category D with positive evidence of human fetal risk. The FDA is in the process of revising these guidelines because they are too simplistic and do not give any guidance to physicians faced with pregnant women with psychiatric diagnoses. New guidelines will give more information on these medications as well as help women and providers to make risk/benefit decisions (
89).
Principles of treatment during pregnancy
The therapist should first consider whether psychological interventions such as some type of psychotherapy would be effective. There is, unfortunately a dearth of good studies to document the effectiveness of psychotherapy to treat psychiatric illness during pregnancy (
90).
No one can say with absolute certainty that any medication is free of risk. Overall, taking psychotropic medication during pregnancy appears to be less risky for the baby than experiencing untreated mood disorders or psychoses is for the mother.
Most antidepressants appear to be safe to use during pregnancy. There is a small elevated risk of miscarriage and a slight statistically significant increase in prematurity that is likely not clinically significant.
Most typical antipsychotics appear to be safe during pregnancy. If atypical psychotics are used, watch for problems with glucose metabolism and excessive weight gain.
Valproic acid is particularly dangerous during pregnancy. Lamotrigine, lithium, and carbamazepine are safer. If discontinuation of valproic acid is impossible, folic acid 4 mg daily may offer some degree of protection.
If the patient continues to take medication, prescribe it in the lowest effective dose and give in divided doses. Dosages often need to be increased later in pregnancy when there are further changes in weight, metabolism, excretion, and lean/fat ratios (
91). The patient should avoid diuretics and low-salt diets.
Postpartum period
The main concern about taking medication in the postpartum period is the possible effect on the breastfeeding infant. All of these medications pass into breast milk but in amounts much lower than those in the mother. Drug excretion into the breast milk of less than 10% of the maternal dose is unlikely to lead to dose-related adverse events in the infant (
92). Mothers may assume that, to be perfectly safe, they should avoid taking medication until they finish breastfeeding. Once again, it is important to identify possible risks of not treating a major psychiatric illness during this time. These include poor infant care, rejection of the infant, poor parental relationships, suicide, infanticide, long-term failure to bond with the child, guilt, delayed infant development, and failure to thrive.
Research can determine immediate and possibly short-term consequences to the infant but, because of the multiple variables involved, would not be able to discover any long-term consequences.
Antipsychotics
Typical antipsychotics are excreted in breast milk at the rate of less than 3% of maternal levels (
93). Although there have been some reports of drowsiness and lethargy, there have been many reports indicating the absence of adverse events (
44). Less than 5% of atypical antipsychotics are found in breast milk (
93). Clozapine has been associated with sedation, decreased sucking reflex, restlessness and irritability, seizures, and cardiac instability in the breastfed infant (
94).
Antidepressants
Although data are limited, the majority of antidepressants appear in breast milk in very small to undetectable amounts (
44,
95). Although some concern has been expressed for fluoxetine, citalopram, and venlafaxine, if these are the drugs that best treat the mother's depression, they should be continued. Infants do not show any immediate or short-term problems.
Mood stabilizers
Valproic acid, lamotrigine, and carbamazepine all appear to be safe to use during breastfeeding. Lithium may be used, but the infant is vulnerable to developing toxic levels if he or she vomits or has diarrhea. To breastfeed while taking lithium, the mother has to be observant for any signs of toxicity and have quick access to services where the baby's lithium level can be checked.
Principles of treatment during breastfeeding
Psychosocial and psychological interventions may be effective treatment options for mothers with postpartum depression. However, the lack of well-designed investigations makes it impossible to draw definitive conclusions. In addition, therapies such as cognitive behavior therapy and interpersonal therapy are time consuming, and trained therapists are hard to find and may be costly (
96).
It is possible for women to take psychotropic medication while breastfeeding. Although some mothers may want to defer treatment for 6–9 months, their worsening depression, inability to function well, problems enjoying time with the baby, and delays in bonding are not beneficial to the woman, her child, or the other parent. The potential harms of not treating far outweigh any concerns about taking medication.
Several scientific groups have developed guidelines regarding the use of antidepressants during breastfeeding (
97,
98):
•.
The choice of treatment should derive from a personalized risk/benefit analysis.
•.
Provide complete information to allow the patient to make an informed decision.
•.
Consider psychotherapy as first line treatment for mild to moderate depression.
•.
Consider antidepressants for severe depressions or lack of response to psychotherapy.
•.
The choice of antidepressants should be based on previous efficacious treatments.
•.
Start at the lowest effective dose and increase gradually.
•.
Monotherapy is preferred.
•.
Monitor the infant's condition, particularly for sick or low-birth-weight babies.
•.
Routine infant serum levels are not recommended.
Scenario 6
A 36-year-old woman has increasing sleep difficulties postpartum. She feels exhausted, her appetite is poor, and she has little energy. She has been feeling like a very bad mother because she finds looking after the baby is overwhelming and longs for her freedom. She is breastfeeding.
First, ensure that the woman wants to breastfeed and is not being pressured to do so because it is good for the baby. Breastfeeding may be very arduous for a depressed mothers, but she may find it difficult to tell others she wants to stop. If a mother with a mental health problem continues to breastfeed, she should consider supplementing feeding with a bottle so it will be possible for others to do some feedings, allowing her to get some uninterrupted sleep. The amount of drug ingested by the baby may be reduced if the mother feeds the baby previously pumped milk for the first few hours after taking her medication (99).
Women with bipolar disorder must be especially cautious postpartum because manic episodes can occur as soon as 3 days postpartum. It is important for a woman to be taking a mood stabilizer to prevent this. The administration of lithium immediately after delivery has been shown to decrease the rate of recurrence of a manic episode from 50% to 10% (100).
Scenario 7
A 28-year-old woman with a diagnosis of bipolar disorder with manic and depressive episodes increased her lithium dose over the course of her pregnancy. She was able to remain stable throughout the pregnancy.
If the woman has been increasing her dosage during the pregnancy, it may be wise to decrease the dose of lithium slightly before delivery to decrease the risk of lithium toxicity in the mother and neonate. If the woman has discontinued her mood stabilizer during the pregnancy, medication should be restarted immediately postpartum.
Summary
Psychiatric illness can occur during pregnancy and the postpartum period. Not only will the mother feel distressed but also these illnesses can cause direct and indirect harm to the baby as well as create long-term negative consequences for the mother and the couple. Research on the effects of psychotropic drugs on the fetus and on breastfeeding is limited by the inability to establish gold standard trials. Research that is published must also be viewed critically as poor methodologies can lead to unwarranted and alarming conclusions. The clinician must use the evidence available to make risk/benefit analyses about the best course of action. The clinician must be sensitive to the fact that mothers must make difficult choices based on evidence that may be limited. Educating the mother about what information is available assists her in making decisions that will be of most benefit to her and her baby.