This exercise is designed to test your comprehension of material relevant to this issue of FOCUS as well as your ability to evaluate, diagnose, and manage clinical problems. Answer the questions below, to the best of your ability, on the information provided, making your decisions as you would with a real-life patient.
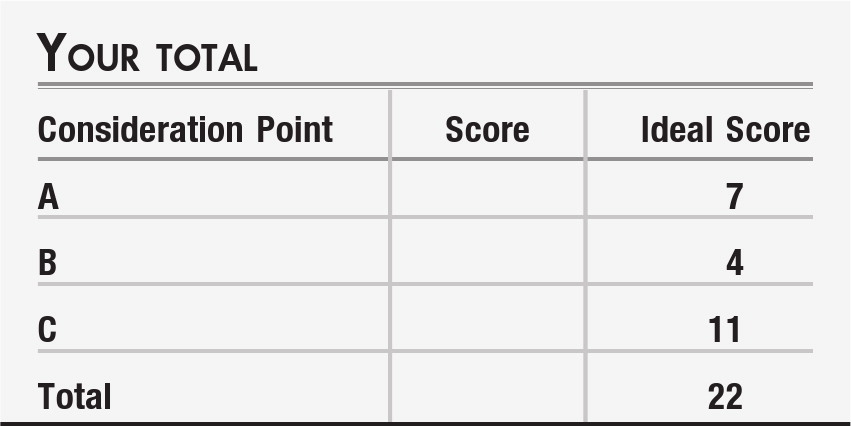
Questions are presented at “consideration points” that follow a section that gives information about the case. One or more choices may be correct for each question; make your choices on the basis of your clinical knowledge and the history provided. Read all of the options for each question before making any selections. You are given points on a graded scale for the best possible answer(s), and points are deducted for answers that would result in a poor outcome or delay your arriving at the right answer. Answers that have little or no impact receive zero points. At the end of the exercise, you will add up your points to obtain a total score.
Case vignette
Samantha is a 22-year-old woman who was brought in to see you by her twin sister, Marianne, who expressed concern about her sister's “blues” and changes in behavior. Marianne had set up the appointment and came along with Samantha, because Samantha had some ambivalence about seeking psychiatric help. Samantha stated that she wanted Marianne to be there for the visit, as Marianne was her “main strength” in facing her problems.
When the patient came in for her evaluation, she reported that she had been “feeling blue” a great deal of the time since being laid off from her job as an assembly line worker for a local automotive parts manufacturer about 10 months ago. She had married her high school sweetheart, Robert, 3 years ago, and both had been working while the patient's mother took care of their infant son, Tyler, born 2 years ago. With the layoff, her husband became the sole breadwinner for the family and, around that time, the patient's father had a stroke and so her mother could no longer help with caring for Tyler. In the context of all these psychosocial changes, the patient reluctantly became a stay-at-home mom, determined to “keep up appearances” in the small suburban town where they lived.
Marianne added that, over the past 8–10 months, her sister not only had been talking about feeling “blue” and “overwhelmed” but also had lost a lot of weight. As twins, they had always been about the same size, but now Samantha was about “three dress sizes smaller” by Marianne's estimation. Samantha noted that she was “just not interested in eating.” She endorsed irregular sleep, which she attributed to trying to take care of their toddler while her husband's work frequently put him on the “graveyard shift” at the local power company. She said that, generally, her energy was “barely hanging in there” and that she felt “exhausted” much of the day; this was the case even after sleeping a solid 9 hours on the weekend, when her husband could play with Tyler and let her “sleep in.” She denied any suicidal thoughts and said that, to the contrary, she was “doing all I can to be a Super Mom.” She endorsed psychomotor slowing, along with anxiety symptoms of excessive worry about the future when trying to fall asleep, sometimes keeping her awake for 2 or 3 hours after lights-out. She said this was the first period in her life that she had experienced this set of symptoms, and Marianne confirmed this. They also noted that no one else in the family had a history of mental health issues.
Marianne then shared that “there are also these other times when Samantha is ‘up’ for a day or two…she has a lot more energy, is flying around the house cleaning, and talks a blue streak.” Samantha looked down at the floor as her sister added this, but did not contradict her. She said “whenever I have more energy, I try to put it to good use, wouldn't anyone? Keeping the place the way we'd like it is hard. And it's so hard to try to be perfect when there's such a struggle around money, and when Tyler has a day with lots of tantrums, I'm just trying to do my best. Still, I feel exhausted and can't play with him the way I think I should … I just don't enjoy it much. Actually, I don't enjoy anything much anymore.”
Consideration Point A:
At this point in your evaluation, the diagnosis which seems most appropriate for this patient would be
| A1._____ | Major depressive disorder, single episode |
| A2._____ | Bipolar disorder, depressed phase |
| A3._____ | Adjustment disorder, related to financial and familial pressures |
| A4._____ | Substance-induced mood disorder |
| A5._____ | Schizophrenia, undifferentiated |
Vignette continues
As you inquired more about these higher-energy periods, Samantha became a bit guarded and defensive in what she said. Evidently these periods never last more than a day, come at seemingly random times, and have not apparently interfered with Samantha meeting her responsibilities at home. Both she and Marianne confirm that Samantha was the more “emotional” of the two of them when they were growing up, but that “moodiness” has not been a significant problem.
In reviewing her medical history, you learned that Samantha has no allergies or general medical conditions. Socially and developmentally, she had been a B student at the local high school and, unlike her sister, had been a cheerleader in high school. As a result, she also had socialized a lot with the football team, which is how she had met Robert, her husband. In response to your question about any injuries, she reported that she had been a restrained, back-seat passenger in a car accident at age 18, when she and friends had been driving home after a victory celebration party, marking a successful football season their senior year. The driver, another cheerleader, had been drinking and smoking marijuana and had hit a mailbox at the side of the road before ending up in a ditch. Airbags had not deployed, and others in the car managed to get the car back on the road and on their way before police arrived, so the event was never reported to authorities. Samantha herself was not physically injured beyond some minor bruising, but she swore off marijuana after that, although she still continues to smoke “a pack a week” of cigarettes and drink alcohol “once in a while.”
On examination, you noticed that, in addition to looking gaunt compared with her sister, her skin appeared “older” in terms of color, skin turgor, and fine wrinkles and that her dentition was poor. She blamed this on insurance issues: “I had dental coverage at my job, but Robert, his benefits only cover a dentist three towns over, and I can't get there easily, what with watching Tyler.” She looked sad and apathetic, with mild psychomotor slowing and some latency in her speech when responding to your questions.
Samantha appealed to you to help her, and she has seen enough direct-to-consumer ads for antidepressant medications to ask you to prescribe something. She and Marianne asked reasonable questions about pharmacotherapy.
Consideration Point B:
At this point, the treatment option that seems most appropriate for this patient would be
| B1._____ | Start a selective serotonin reuptake inhibitor (SSRI) antidepressant. |
| B2._____ | Start a mood stabilizer, such as lithium. |
| B3._____ | Initiate psychotherapy. |
| B4._____ | Offer reassurance that “anyone would feel bad” given her circumstances, and tell her she could follow up “as needed” if she is still feeling this way in another month. |
Vignette continues
After careful consideration, you decided to prescribe an antidepressant, as the patient said “I don't really want to talk about my problems … isn't there a pill that can help?” Because of some concern about a bipolar-spectrum disorder with an unusual presentation, you scheduled her to return in 1 week for an in-office visit, with explicit directions for Samantha or Marianne to call you with any concerns or questions that might come up sooner.
Samantha and Marianne returned the next week as planned. Samantha stated that she had been adherent with the medication, taking it daily as directed. She stated that she had experienced some nausea on the first 3 days after starting, but this had largely resolved by the visit date. She reported her mood was still depressed, and no other symptoms had changed.
Marianne then looked at Samantha and said “isn't there something else you need to tell the doctor?” Samantha looked evasively around the room, and Marianne handed you a small brown paper bag. “I found this in Samantha's car,” she noted. Inside were three small pieces of a clear, crystalline solid in a small plastic bag and a glass pipe.
“Yes yes yes, OK, yes, I've been smoking crystal,” Samantha confessed to you both. She then began to sob uncontrollably, “What am I going to do? How can I tell Robert? I'm the world's worst mother! I've been leading a double life.”
In between crying spells, Samantha elaborated that, after losing her job, she sometimes would go to a bar she used to frequent before she was married. There she met some acquaintances from high school who introduced her to crystal methamphetamine (MA) as a way to “help me feel not so bad” and to “give me energy.” Her use increased over the past 8 months, and she found herself trading [unprotected] sex for MA so that her husband wouldn't find out about excess spending for her drug habit.
Consideration Point C:
At this point, given the apparent role of MA in the patient's symptoms, what do you recommend?
| C1._____ | Switch from the SSRI to a serotonin-norepinephrine reuptake inhibitor (SNRI) |
| C2._____ | Referral to a 12-step program |
| C3._____ | Referral to a brief inpatient detoxification program followed by a partial hospital program |
| C4._____ | Referral to an inpatient 30-day program |
| C5._____ | Referral for medical care to test her for hepatitis and HIV infection |
| C6._____ | Referral for dental care |
Vignette concludes
Fortunately, you have the next hour open in your schedule to address Samantha's complex situation. Marianne called Robert, who was at home with Tyler at the time and asked him to come right over to your office. He arrived about 10 minutes later, and a brief but focused family meeting in your office created a safe place for Samantha to “come clean” with her husband about her MA use. A mixture of sympathy, shock, betrayal, and confusion permeated the family discussion. Robert reported that he had known “something was wrong, different” with Samantha, but that he was so fatigued from working a lot of double shifts “to make ends meet,” that he had not been observant about things. “So, 2 months ago, when I was worried about Tyler getting diaper rash that never went away, were you too high to remember to change his diapers?” “Yes,” replied a sobbing Samantha, “please don't hate me … please help me!”
Robert's benefits did not cover a 30-day inpatient program but did cover the inpatient detox admission and partial hospital program for an intensive psychoeducational program. Given Samantha's challenges in decision making, this appeared to be an appropriate next step. After she started the partial hospital program, Samantha began a 12-step program and had individual and group counseling; the objectives of these psychotherapy programs were to promote insight into the impact of MA use and to address the issues of feeling overwhelmed that were part of the initiation to MA use. She continued to take the SSRI you had started, with the dose titrated by the physician running the partial hospital program
You recognized that you were obligated to notify Social Services about the issue of child neglect. Based on other cases in your area, the most likely scenario is that Tyler will remain in the home provided that the patient's mother and sister can help take care of him when Robert is working.
Answers: scoring, relative weights, and comments
Consideration Point A:
| A1._____ | +3 Major depressive disorder, single episode. The patient has sufficient symptoms and duration to meet DSM criteria for major depressive disorder (1). |
| A2._____ | +1 Bipolar disorder, depressed phase. Although the patient has never apparently had a manic episode of sufficient duration and impairment to warrant a diagnosis of bipolar disorder type I, the possibility of bipolar disorder not otherwise specified cannot be excluded because of frequent but brief periods of excess energy and high productivity. The absence of a family history does not rule against this diagnosis but does not support it (1). |
| A3._____ | +2 Adjustment disorder, related to financial and familial pressures. This patient, like many, has experienced a set of stressful circumstances that occurred at the same time. It is possible that her coping skills have been maximally taxed and that many symptoms might resolve if she suddenly became employed again. The presence of neurovegetative symptoms, however, suggests that this is not simply a reaction to circumstances but has taken on a psychobiological life of its own (1). |
| A4._____ | +1 Substance-induced mood disorder. Overt or covert substance use can have an impact on mood, either in intoxicated or withdrawal states (e.g., psychostimulants or alcohol) (1). |
| A5._____ | −5 Schizophrenia. Although patients in the prodromal period before a first psychotic episode may complain of mood or anxiety issues, the historical data are not compatible with a diagnosis of schizophrenia (1). |
Consideration Point B:
| B1._____ | +2 Start an SSRI antidepressant. Evidence-based guidelines support the use of antidepressant medications as first-line treatments for major depressive disorder (2). |
| B2._____ | −1 Start a mood stabilizer, such as lithium. Without a clear diagnosis of a bipolar spectrum disorder, the introduction of a mood stabilizer such as lithium is unlikely to improve depressive symptoms yet carries a side effect burden (3). |
| B3._____ | +2 Initiate psychotherapy. Psychotherapy is a first-line evidence-based treatment for depression (1) although the neurovegetative symptoms should be monitored closely and consideration should be given to addition of pharmacotherapy if they persist. |
| B4._____ | −2 Only offer reassurance. Given the level of symptomatic distress and functional impairment, this is likely to be undertreatment and slow her access to more useful care. |
Consideration Point C:
| C1._____ | −2 Switch from the SSRI to an SNRI. There is little evidence that this switch will help with symptoms after only 1 week of treatment (2), and the focus on medication switching may delay the patient from engaging in more critical treatment steps. |
| C2._____ | +2 Referral to a 12-step program. Twelve-step programs are a useful component of treatment for substance use disorders, but this patient's usage pattern suggest that this may be insufficient as a sole intervention (4). |
| C3._____ | +3 Referral to a brief inpatient detoxification program followed by a partial hospital program. Evidence-based guidelines suggest that a moderately high level of intensity is indicated when a patient's use pattern and social supports are probably insufficient to lead to successful outcome solely through outpatient treatment (4). |
| C4._____ | +3 Referral to an inpatient 30-day program. Inpatient care can be helpful, but many benefits packages do not include this in the mental health/substance use “carve-out” and self-paying may be prohibitively expensive (4). |
| C5._____ | +2 Referral for medical care to test her and her family for hepatitis and HIV infection. Although this is not on the critical path to achieving abstinence from her MA use, her behavior during the past months has placed her and her family at risk for communicable diseases, which have the potential to be fatal (5). |
| C6._____ | +1 Referral for dental care. Again, this is not on her critical path to abstinence, but dental problems are common among MA users, and the visible reminder of her failings every time she looks in the mirror or interacts with others may slow her ability to recover fully (6, 7). |