Augmenting Cognitive Behaviour Therapy for Post-Traumatic Stress Disorder with Emotion Tolerance Training: A Randomized Controlled Trial
Abstract
Background
Method
Results
Conclusions
Introduction
Method
Patients
Study Entry Criteria
| Support/CBT (n = 34) | Skills/CBT (n = 36) | Test | |
|---|---|---|---|
| Mean age, years (s.d.) | 41.15 (12.92) | 37.86 (12.70) | t68 = 1.10, p = 0.29 |
| Mean time since trauma, months (s.d.) | 52.42 (117.00) | 45.56 (83.73) | t68 = 0.28, p = 0.78 |
| White ethnicity, n (%) | 29 (85) | 29 (81) | χ2 = 0.28, p = 0.78 |
| Gender, n (%) | |||
| Male | 17 (50) | 15 (42) | χ2 = 0.49, p = 0.48 |
| Female | 17 (50) | 21 (58) | |
| Employed, n (%) | 25 (76) | 27 (77) | χ2 = 0.20, p = 0.89 |
| Trauma type, n (%) | |||
| MVA | 15 (44) | 15 (42) | χ2 = 0.04, p = 0.84 |
| Assault | 19 (56) | 21 (58) | |
| Co-morbid MDD, n (%) | 18 (60) | 22 (67) | χ2 = 0.30, p = 0.58 |
| Co-morbid anxiety disorder, n (%) | 9 (33) | 12 (35) | χ2 = 0.03, p = 0.87 |
| Co-morbid substance use disorder, n (%) | 3 (10) | 4 (12) | χ2 = 0.05, p = 0.82 |
| Mean logic rating (s.d.) | 7.69 (1.54) | 7.75 (1.14) | t68 = 0.18, p = 0.86 |
| Mean expectancy rating (s.d.) | 7.52 (1.68) | 7.66 (1.54) | t68 = −0.34, p = 0.74 |
Design
Treatment Conditions
Support/CBT.
Skills/CBT.
Measures
Diagnostic interview.
Self-report measures.
Treatment fidelity.
Data Analysis
Results
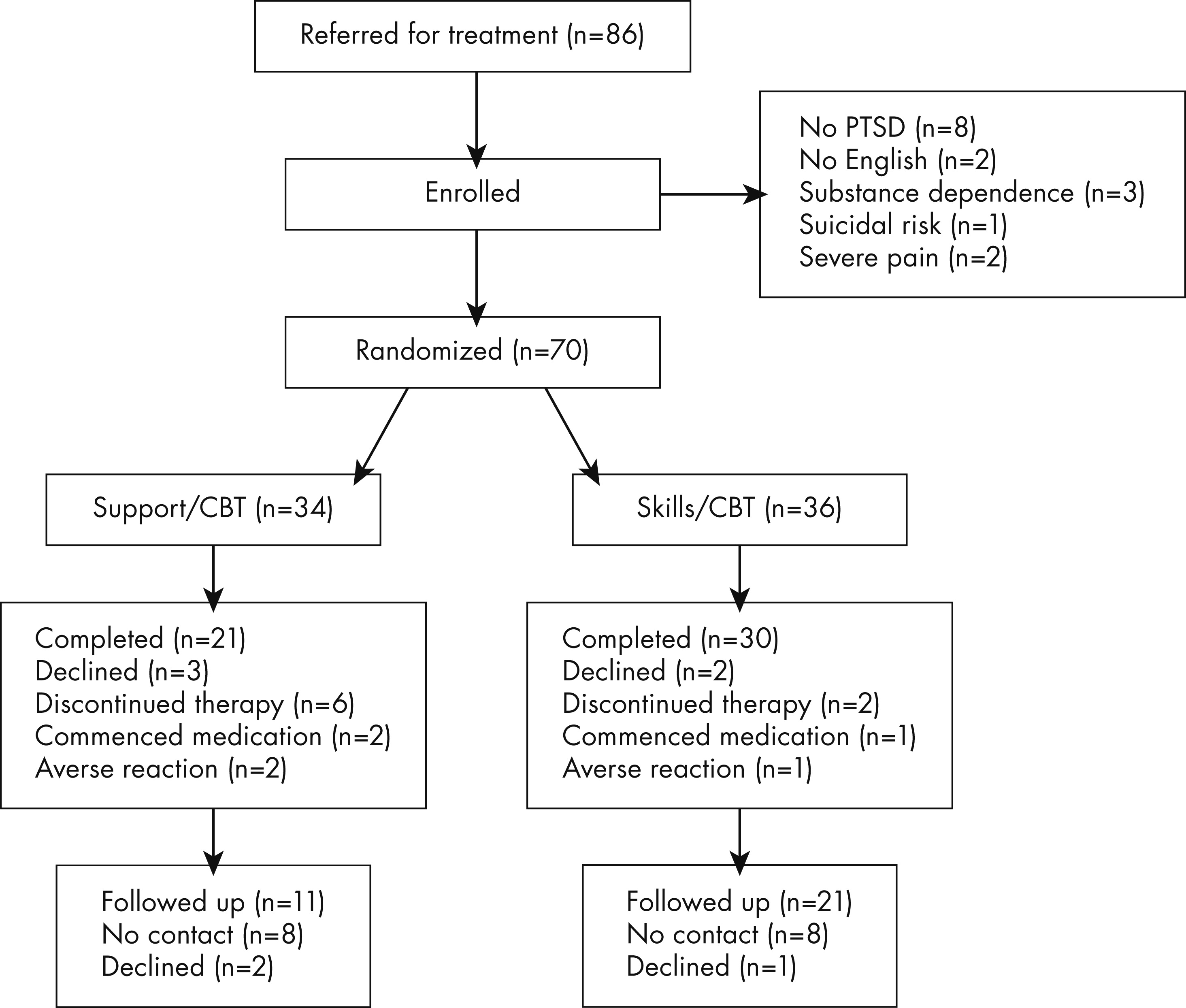
Patient Flow
Primary Outcomes
| Support/CBT (n = 34) | Skills/CBT (n = 36) | F | p | ή | Between-condition effect size | |
|---|---|---|---|---|---|---|
| Pre-treatment | ||||||
| CAPS | 67.69 (16.26) | 73.75 (17.79) | 2.18 | 0.14 | 0.03 | −0.38 (95% CI −0.86 to 0.09) |
| IES-Intrusions | 28.10 (6.12) | 26.05 (6.86) | 1.73 | 0.19 | 0.03 | 0.32 (95% CI −0.15 to 0.79) |
| IES-Avoidance | 25.91 (8.74) | 24.61 (7.89) | 0.43 | 0.51 | 0.01 | 0.15 (95% CI −0.31 to 0.62) |
| BDI-II | 28.10 (6.12) | 26.06 (6.85) | 2.15 | 0.15 | 0.03 | −0.30 (95% CI −0.76 to 0.18) |
| BAI | 27.67 (14.57) | 27.94 (13.75) | 0.01 | 0.94 | 0.00 | 0.02 (95% CI −0.49 to 0.45) |
| PTCI-Self | 4.08 (1.29) | 4.41 (1.18) | 1.25 | 0.27 | 0.02 | −0.32 (95% CI −0.79 to 0.15) |
| PTCI-World | 5.34 (1.06) | 5.60 (0.68) | 1.56 | 0.22 | 0.02 | −0.05 (95% CI −0.52 to 0.42) |
| PTCI-Blame | 2.75 (1.46) | 2.82 (1.52) | 0.04 | 0.84 | 0.00 | −0.03 (95% CI −0.50 to 0.44) |
| Post-treatment | ||||||
| CAPS | 38.76 (20.81) | 32.43 (21.61) | 0.75 | 0.39 | 0.01 | 0.29 (95% CI −0.17 to 0.76) |
| IES-Intrusions | 11.99 (7.46) | 8.89 (6.27) | 3.01 | 0.09 | 0.04 | 0.44 (95% CI −0.03 to 0.92) |
| IES-Avoidance | 11.96 (8.73) | 9.21 (8.19) | 1.23 | 0.27 | 0.02 | 0.33 (95% CI −0.14 to 0.80) |
| BDI-II | 18.21 (7.86) | 17.08 (11.54) | 1.63 | 0.21 | 0.03 | 0.12 (95% CI −0.35 to 0.59) |
| BAI | 15.97 (10.27) | 16.28 (11.71) | 0.03 | 0.86 | 0.00 | −0.02 (95% CI −0.49 to 0.45) |
| PTCI-Self | 2.56 (1.07) | 2.83 (1.38) | 0.06 | 0.80 | 0.00 | −0.16 (95% CI −0.63 to 0.31) |
| PTCI-World | 3.96 (1.02) | 4.61 (1.23) | 3.82 | 0.06 | 0.06 | −0.63 (95% CI −1.10 to −0.14) |
| PTCI-Blame | 2.28 (0.79) | 2.22 (0.92) | 0.47 | 0.49 | 0.01 | 0.12 (95% CI −0.35 to 0.56) |
| Follow-up | ||||||
| CAPS | 47.54 (22.45) | 37.47 (23.49) | 27.44 | 0.00 | 0.30 | 0.43 (95% CI −0.04 to 0.90) |
| IES-Intrusions | 17.09 (8.18) | 11.36 (6.28) | 9.61 | 0.003 | 0.13 | 0.77 (95% CI −0.23 to 1.26) |
| IES-Avoidance | 15.96 (8.86) | 15.44 (8.78) | 0.05 | 0.82 | 0.00 | 0.07 (95% CI −0.40 to 0.54) |
| BDI-II | 22.11 (9.78) | 19.80 (11.33) | 2.16 | 0.15 | 0.03 | 0.22 (95% CI −0.25 to 0.69) |
| BAI | 18.55 (9.54) | 14.17 (8.35) | 6.37 | 0.01 | 0.09 | 0.38 (95% CI −0.09 to 0.85) |
| PTCI-Self | 2.92 (0.69) | 3.21 (1.19) | 0.37 | 0.54 | 0.01 | −0.30 (95% CI −0.77 to 0.17) |
| PTCI-World | 5.07 (1.48) | 4.83 (1.30) | 8.98 | 0.004 | 0.12 | 0.19 (95% CI −0.28 to 0.66) |
| PTCI-Blame | 2.60 (0.67) | 2.45 (1.16) | 0.95 | 0.33 | 0.02 | 0.20 (95% CI −0.27 to 0.67) |
Secondary Outcomes
Effect Sizes
Between-Session Distress Ratings
| Support/CBT | Skills/CBT | |
|---|---|---|
| Session 1 | 61.17 (25.88) | 65.75 (20.02) |
| Session 2 | 65.00 (23.39) | 63.09 (17.54) |
| Session 3 | 68.52 (24.75) | 66.91 (27.01) |
| Session 4 | 69.42 (24.79) | 70.97 (24.25) |
| Session 5 | 67.36 (27.45) | 65.97 (30.75) |
| Session 6b | 65.01 (26.87) | 72.01 (32.17) |
| Session 7 | 68.53 (24.61) | 49.22 (19.31) |
| Session 8 | 70.88 (25.36) | 55.74 (21.18) |
| Session 9 | 51.07 (22.90) | 49.55 (18.75) |
| Session 10 | 57.09 (22.16) | 60.17 (35.50) |
| Session 11 | 53.53 (21.87) | 46.45 (20.34) |
| Session 12 | 50.00 (22.02) | 35.89 (18.09) |
Treatment Completer Analyses
Discussion
Efficacy and Mechanisms
Methodological Limitations
Clinical Implications
References
Information & Authors
Information
Published In
History
Authors
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBGet Access
Login options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).

