Smoking and Mental Illness: Strategies to Increase Screening, Assessment, and Treatment
Abstract
Clinical Context for Assessing and Treating Tobacco Use Disorders
| Disorder and treatment group | Epidemiology and Data | Tips for Treatment |
|---|---|---|
| Disorder | ||
| Schizophrenia | Smoke at nearly 3 times the rate of the general population (90% prevalence) (27–29) | Monitor medication levels when possible (i.e., clozapine), because quitting smoking can affect dosing needs. |
| Smoking behavior is reinforced by a subjective sense of improving psychiatric symptoms or cognitive functioning; also may have less neuroleptic-induced parkinsonism (30, 31) | May need higher doses of NRT, because people in this group have higher nicotine levels when they smoke | |
| Efficiently smoke cigarettes, smoking filters and discarded butts that are high in nicotine (32, 33) | ||
| Medication levels may be affected and can be a life-threatening consequence (see the pharmacotherapy section) | ||
| Those taking atypical antipsychotics such as risperidone, clozapine, or olanzapine were approximately 3 times more successful in quitting and reducing cigarette smoking than those treated with the older, first-generation antipsychotics (34) | ||
| Depression | Depression is twice as common in smokers as in nonsmokers and is 4 times as common in heavy smokers (35) | May need more medications to aid in attempt |
| Depressive symptoms can make early abstinence difficult | Consider bupropion to treat tobacco dependence | |
| People who are predisposed to nicotine dependence may also be predisposed to depression | Even subclinical depression can make a quit attempt more difficult, so monitor mood | |
| Cigarette smoke has MAOI activity that may lead to reinforcing effects of smoking (because there is increased action of the neurotransmitters norepinephrine, serotonin, and dopamine) | Discuss weight and weight gain (5 lb [2.25 kg]) | |
| Weight gain (5 lb [2.25 kg] on average) that occurs with quitting smoking may be important to this group, especially as it relates to affect and antidepressants | Relapse prevention therapy may be integrated with CBT treatments of depression | |
| Smokers with comorbid depression smoke more heavily than the average smoker (36) | ||
| Anxiety | Smoking is a risk factor for the onset of panic disorder. Although smoking can lead to panic attacks, the reverse relationship (that panic attacks lead to smoking) is unlikely and is not supported by research findings (37) | Withdrawal may be difficult for smokers with anxiety, especially in early quit periods; NRT may help ease this |
| PTSD is also associated with rates of smoking, at roughly 60% (38). In heavy smokers with PTSD, there are more total PTSD symptoms as well as increased cluster C (avoidance and numbing) and cluster D (hyperarousal) symptoms (39) | ||
| Patients may report subjectively that smoking reduces anxiety, but studies show that chronic nicotine use is related to increased anxiety (40, 41) | ||
| Substance use | Smokers have a 2–3 times greater risk for alcohol dependence compared with nonsmokers (42), and those with alcohol dependence have dramatically increased rates of smoking (43) | Integrating smoking cessation into the quit plan can take advantage of the same behavioral techniques used in their substance use disorder |
| Smoking rates are 3 times higher and quit rates 4 times lower than the U.S. population (44) | ||
| There is worsened combined morbidity and mortality from concurrent smoking and alcohol dependence; although notably, more alcoholics die from smoking-related diseases than from alcohol-related diseases | ||
| Treating tobacco dependence does not worsen other substance use and may even improve sobriety | ||
| Treatment group | ||
| Adolescents | Adolescent tobacco users are twice as likely to have a history of a mental illness or a substance use problem compared with those who do not use tobacco | Need parental consent for pharmacotherapy |
| Common psychiatric problems are disruptive behavior disorders (especially oppositional defiant disorder, conduct disorder, and, to a lesser extent, attention-deficit hyperactivity disorder), major depressive disorder, and substance use disorders | ||
| Adolescent tobacco smokers are 4 times as likely to also use alcohol, 8 times more likely to use marijuana, and 22 times more likely to use cocaine | ||
| Inpatients | Among hospitalized smokers with mental illness, 65% were interested in quitting (26) | Start NRT in the hospital to help reduce withdrawal; this can also reduce hospital anxiety and agitation |
| Many psychiatric facilities are nonsmoking areas; this is the perfect opportunity to allow the smoker to get through the most difficult symptoms and period of withdrawal | On discharge, prescribe NRT for continuity |
Treatment Strategies and Evidence
The Five A’s
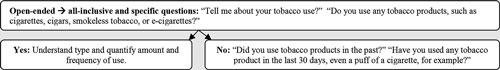
Ask about tobacco use (first A).
| Nicotine Amount | Format of Packaging and Use | Common Brands | ||
|---|---|---|---|---|
| Product | Total Nicotine Content | Blood Plasma Nicotine Yield | ||
| Smoked | ||||
| Cigars, little cigars, and cigarillos | Because of the wide range of sizes in which cigars are offered, there is a large variance in the amount of nicotine that one might contain. Cigars typically contain around 100–200 mg but can contain as much as 444 mg (51–53) | The amount of nicotine absorbed through cigar smoking greatly varies and is contingent on a number of factors, including the duration of time and the number of puffs the smoker takes to smoke the entire cigar and whether the smoker inhales. Proportional to the total nicotine amount and yield of cigarettes, it can be estimated that cigars yield anywhere from 9 to 68 mg of nicotine | Tobacco leaves are rolled and tightly packed with dried and fermented tobacco, forming a cylindrical shape for smoking. A little cigar is the smallest version and is equivalent to the size of a standard cigarette. A cigarillo is a slightly larger and narrower version. The largest variety of cigars can measure ≥7 inches in length (52) | Swisher Sweets, Dutch Masters, Phillies, Cheyenne, Derringer (large cigars and cigarillos); Universal, Bodyshot (little cigars) (50) |
| Waterpipe or hookah | Nicotine content can range from 1.8 to 6.3 mg per gram of tobacco (54) | Exposure is suggested to be comparable to that of a cigarette (55). However, there is strong variance in nicotine exposure influenced by a variety of determinants, including the burning temperature, type of tobacco, individual smoking patterns, and duration of smoking session (a 1-hour hookah session equates to approximately 200 puffs or 10 cigarettes, an estimate yield of roughly 10–20 mg of nicotine per 1-hour session) (57) | This is a device used for smoking tobacco that delivers cooled charcoal tobacco smoke, which passes through water before it is inhaled | Al Fakher, Al Waha, Nakhla, Romman, Fumari, Sahara Smoke Company (56) |
| Nontobacco | ||||
| Electronic cigarettes (e-cigarettes; also referred to as electronic nicotine delivery systems) | The amount of nicotine in the e-liquid ranges in strengths of 6–24 mg/mL (1 cartridge) (58) | On average, 50%–60% of nicotine in a cartridge is inhaled as vapor by the user (i.e., approximately 0.25–0.77 mg of nicotine per 15 puffs). Most cartridges deliver up to 150 puffs (i.e., roughly 2.5–7.7 mg per cartridge) (59) | This is a battery-powered device designed to mimic a cigarette, supplying nicotine in an e-liquid cartridge that is inhaled as vapor, rather than by burning tobacco, and it is offered in flavored options | V2 Cigs, Vapor Fi, Halo Cigs, Apollo, South Beach Smoke (56) |
| Smokeless | ||||
| Chewing tobacco and snuff | One dip or pouch is equivalent to 5 cigarettes, whereas 1 can, containing 144 mg of nicotine, equates to smoking 4 packs of cigarettes (60) | Typically, the nicotine yield can range from 3.6 to 4.5 mg. Of note, compared with the 7 seconds it takes for the brain to respond to nicotine from a drag of a cigarette, the same effect can be delayed to up to 30 minutes for chew or snuff users, although it is continuously delivered for up to 60 minutes after use, whereas nicotine delivery ceases immediately after the last puff of a cigarette (63) | Chew is a more finely ground form of tobacco packaged in a tin can and is directly placed as a wad between the gum and the cheek to allow nicotine to be absorbed by the mouth tissue. Snuff is provided in the form of loose leaves and is encapsulated in a porous pouch. Both products are spit out after use | Chew: Red Man, Chattanooga Chew; snuff: Bruton, Copenhagen, Skoal, Grizzly, Kodiak (61, 62) |
| Dissolvable products | The total amount of nicotine content in these products ranges from 3.90 to 4.09 mg (64) | Per piece, these products can deliver a range of 0.6–3.1 mg of nicotine (65) | These products are provided in candy-like shapes and sizes that melt away in the mouth, which includes lozenges, orbs, pellets, strips, or sticks, where the juices are swallowed and often have a sweet or minty flavor | Ariva, Stonewall, Camel (62) |
Advise the patient to quit (second A).
Assess the patient’s desire to quit (third A).
Assist patients (fourth A).
Arrange follow-up (fifth A)
Strategies for Lower-Motivated Patients
Strategies for Higher-Motivated Patients
Community Resources and Peer Support Options
Pharmacotherapy to Treat Tobacco Use Disorders
| Product | Initial Prescription | Patient Education Issues | Precautions | Side Effects | Approximate Costs |
|---|---|---|---|---|---|
| Nicotine patch (OTC) | Apply 21-mg patch for 4–6 weeks; taper to mid-dose (14 mg) for an additional 2–4 weeks and can use lower dose (7 mg) for another 2 weeks; start at lower dose for lighter smokers | Apply each day to clean, dry, hairless skin, using tape if needed; rotate patch site daily to minimize skin irritation | Caution against using within 2–6 weeks of myocardial infarction or with arrhythmias | Skin reaction/rash (50% of patients), usually mild, treat with 1% hydrocortisone cream or 0.05% triamcinolone cream); vivid dreams or sleep disturbances can occur if worn overnight | $45 per 2-week supply (generics available and effective); $3 per day |
| Nicotine gum (OTC) | 2 mg; 4 mg dose if smoking ≥25 cpd); chew every 1–2 hours as needed; usual range is 9–16 pieces per day | “Chew and park”; avoid coffee and other acidic beverages 15 minutes before/during use | Dentures | Jaw pain, hiccups, mouth irritation; nausea if swallowing saliva | $50 per 2-week supply; (generics available and effective); $3 per day |
| Nicotine lozenge (OTC) | 2 mg; 4 mg (if smoke within 30 minutes of waking); dissolve (do not chew) in mouth; use 9–20 per day for 6 weeks, then taper over 6–12 weeks | Avoid food, coffee, and acidic drinks 15 minutes before/during use | N/A | Hiccups, nausea, heartburn | $43 for 72 lozenges ($0.60 per lozenge); approximately $6 per day, average |
| Nicotine inhaler | Puff as needed; use up to 16 cartridges per day; cartridge has 4 mg of nicotine over 80 inhalations; less may be needed if using combination therapy | Avoid food, coffee, and acidic drinks 15 minutes before/during use; orally absorbed; no need to inhale deeply | Do not use with severe reactive airway disease | Cough, throat irritation (40%) in first 2 days, usually mild and reduces at 3 weeks | $150 per 168 cartridges (approximately $1 per cartridge); prescription is for 168 cartridges (1-month supply) |
| Nicotine nasal spray | One dose is 2 sprays (1 in each nostril); maximum 5 doses per hour; maximum 40 doses per day; use 3–6 months | Spray into nose away from nasal septum with head tilted back; do not sniff | Caution with asthma, rhinitis, sinusitis, nasal polyps | Nasal irritation (80%–90%); possible dependence | $45 per bottle; cost per day varies with use (approximately $5 per day, average) |
| Bupropion SR (Zyban) | 150 mg each morning for 3–7 days, then 150 mg b.i.d., at least 8 hours apart | Start 1–2 weeks before quit date; take second pill in early evening to reduce insomnia | Do not use with seizure disorders, current use of bupropion or MAOIs, electrolyte abnormalities, or eating disorders; monitor blood pressure | Insomnia (40%), dry mouth, headache, anxiety, rash; reduced side effects with 150 mg/day | $90 for 1-month supply; $3 per day; generic forms less expensive |
| Varenicline (Chantix) | “Starter” pack and then “continuation” packs: days 1–3, 0.5 mg every morning; days 4–7, 0.5 mg b.i.d.; weeks 2–12, 1 mg b.i.d.; duration, 12 weeks to 6 months | Quit smoking when starting 1-mg dose; take with full glass of water and after eating | Adjust dosage for renal impairment; black box warnings for neuropsychiatric symptoms (depressed mood, agitation, behavior changes, suicidal ideation or suicide) and cardiovascular adverse events in people with cardiovascular disease | Nausea (take with food); trouble sleeping, abnormal dreams (take second dose earlier in the evening); may also affect the ability to drive or operate heavy machinery | $120 for maintenance dose ($8 per day for 2 tablets) |
Medication algorithm considerations.
NRT.
Bupropion.
Varenicline.
Combination medications.
Effect of Tobacco Use and Cessation on Psychiatric Medications
Effect of Tobacco Abstinence on Mental Illness and Addiction Recovery
Costs of Treatment and Medications for Tobacco Use Disorders
Questions and Controversies
Self-Medication or Tobacco Withdrawal?
Individual Rights to Smoke Versus Group Rights for Tobacco-Free Campuses?
The Tobacco Industry and Mental Illness
Multiple NRT Use and Use While Smoking
E-Cigarettes and Emerging Tobacco Products: New Dangerous Products or Less Harmful and Helpful?
Recommendations
Footnote
References
Information & Authors
Information
Published In
History
Authors
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).