This exercise is designed to test your comprehension of material relevant to this issue of Focus as well as your ability to evaluate, diagnose, and manage clinical problems. Answer the questions below, to the best of your ability, based on the information provided, making your decisions as you would with a real-life patient.
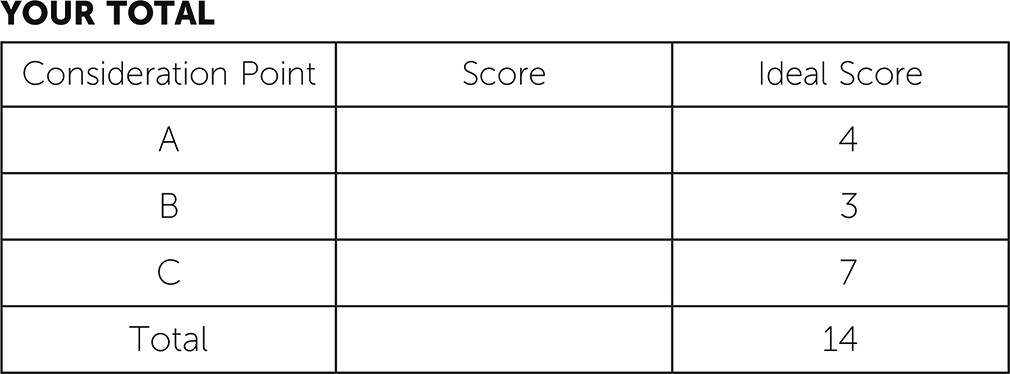
Questions are presented at “consideration points” that follow a section that gives information about the case. One or more choices may be correct for each question; make your choices on the basis of your clinical knowledge and the history provided. Read all of the options for each question before making any selections. You are given points on a graded scale for the best possible answer(s), and points are deducted for answers that would result in a poor outcome or delay your arriving at the right answer. Answers that have little or no impact receive zero points. At the end of the exercise, you will add up your points to obtain a total score.
Case Vignette
You are the only Spanish-speaking psychiatrist at your clinic and receive a referral to see a 17-year-old Hispanic young man with a history of attention-deficit hyperactivity disorder (ADHD). In the past, he had been a patient in the clinic for symptoms of ADHD and behavioral problems but had been lost to follow-up for several months. Previous records indicate that his mother moved to the United States when he was 3 years old and he was left under the care of his maternal grandmother. There, he presented with hyperactivity, impulsivity, and disruptive behavior that reportedly began at age 8 years. Because of such behaviors, he was sent back and forth between his biological father’s home and his maternal grandmother’s care. While under the care of his father, he was physically abused and neglected. As the severity of his behaviors increased, his mother arranged for him to cross the border 2 years ago with his cousin and the help of a “coyote” (a person who smuggles people illegally across borders).
During the patient’s journey, he was detained by immigration officers and was taken into custody for 4 months. While in custody, he was hospitalized twice because of suicidal gestures. He was prescribed 54 mg methylphenidate, 15 mg escitalopram, and 0.25 mg risperidone every morning and 0.75 mg risperidone every night at bedtime while hospitalized. He reunited with his mother, younger half-brother, and mother’s partner. His mother brought him to the clinic at that time because of his disruptive behaviors, exaggerated angry responses, destruction of property, and hyperactivity. His previous provider added 27 mg methylphenidate in the afternoon before he was enrolled in school. While attending a bilingual school, with mostly Spanish-speaking peers, he continued to be disruptive and was not completing his schoolwork. He was subsequently suspended from school. The mother’s boyfriend left the home because of difficulties encountered with managing the patient’s behaviors. The risperidone was increased, his behavior improved, he made great progress academically, and he mastered English as a second language. He was transferred to a different school with primarily English-speaking peers. The patient was lost to follow-up and stopped taking some of his medications before presenting to your office. The referral indicates worsening hyperactivity, irritability, and a question whether he inappropriately touched his half-brother. His mother called the Department of Children and Families, which became involved with the family.
The patient was brought to the clinic by his maternal grandfather. During your interview, the patient endorsed having difficulties falling asleep, worrying about “getting in trouble,” and having nightmares of unclear content. He endorsed sometimes feeling like he is being watched but quickly dismissed his statement. He denied molesting his brother and claimed it was a misunderstanding. He denied having depressed mood, irritability, and auditory or visual hallucinations. He also denied having problems at school or difficulties completing schoolwork. He felt somewhat more comfortable speaking English and stated that he used to misbehave in the previous school because he could speak Spanish to peers and “joke around.” In his new school, he did not have Latino friends and he described that new scenario as helping him focus on schoolwork. His sister had also immigrated to the United States and was now living with him and attending the same school. The patient denied having a history of trauma, except for his father hitting both him and his sister to discipline them. He denied having flashbacks, nightmares, or avoidance related to this type of treatment and described that corporal punishment was the “normal” way to discipline children in his country. He admitted thinking about his journey across the border occasionally but could not explain further.
Consideration Point A
At this point in your evaluation, the diagnosis that seems most appropriate for this patient would be:
A.1
Major depressive disorder
A.2
Posttraumatic stress disorder
A.3
Adjustment disorder with mixed disturbance of emotions and conduct
A.4
Psychotic disorder, not otherwise specified
Vignette Continues
The patient’s grandfather, who accompanied him, could not provide information other than confirming that there were no major behavioral issues at home.
When you call the patient’s mother, she explains that she works full-time and is not able to make it to the clinic during your assigned hours for psychopharmacological follow-up. She really would prefer to continue treatment with you, because she prefers a Spanish-speaking psychiatrist, given her language limitations. However, she cannot afford to miss work, because she is the breadwinner for her three children and the family back in her country.
Consideration Point B
What recommendation do you offer the patient at this point?
B.1
Transfer care to an English-speaking provider whose schedule may be a better fit for the patient’s mother.
B.2
Arrange for a meeting with the patient’s mother to obtain further collateral information and discuss treatment options.
B.3
Discuss the possibility of having the patient’s Spanish-speaking primary care provider prescribe the medications for him.
Vignette Concludes
You arrange a separate meeting with the patient’s mother on a day that works for her schedule to gather collateral information. She reports that her son has made remarkable progress and has earned the “student of the month” award. However, if he misses his medication, he is disruptive and difficult to manage both at home and at school. The mother believes that her son is having difficulties falling asleep because he worries about his immigration status and the involvement of the Department of Children and Families. She provided more historical information and stated that her son was forced by gang members in his country to steal from his grandmother and likely use drugs. She reports that these gang members threatened him with physical harm or death if he did not comply, and she wonders about sexual abuse. Because of his behaviors and stealing, he was sent to live with his father, where he was physically abused. Her son has denied gang-related trauma, but she is “convinced” that this is what happened to him because she “knows how things are back there.” She also reports that the patient’s paternal uncle was a sexual offender and attacked his family with a machete, but receipt of any past diagnosis was unclear to her. The mother shared her worries about her youngest boy’s safety because of the recent events and family history. She shared how these events with her son had triggered her own symptoms of depression and posttraumatic stress disorder because of her own personal history. She also expressed feelings of guilt for having left her son for so many years and how that affected their relationship when he came to live with her.
Consideration Point C
After meeting with the patient’s mother, what cultural issues should you consider, if any?
C.1
Ethnopharmacological factors that could affect the patient’s response to medications
C.2
Cultural beliefs about the patient’s illness and treatment
C.3
Immigration history of the family, including circumstances that led to migration, trauma exposure, acculturation issues, and current supports for all family members
C.4
No cultural factors pertinent for this case
Answers: Scoring, Relative Weights, and Comments
Consideration Point A
A.1
(−1) Major depressive disorder. The patient denies having depressed mood and it is not clear whether he is anhedonic. Depressed mood or anhedonia in addition to other symptoms is requisite to meet criteria for major depressive disorder.
A.2
(+3) Posttraumatic stress disorder. Criteria include exposure or experience of trauma or a traumatic event. The patient was abused by his father; in addition, he suffered detention (and subsequent separation from family) during immigration. He endorsed nightmares and thoughts about his journey across the border. He experiences negative alterations in cognition and mood. This young boy also presents with alterations in arousal and reactivity.
A.3
(−2) Adjustment disorder with mixed disturbance of emotions and conduct. There is no correlation of symptoms with one event; also, his symptoms do not correlate with the length of time for this disorder.
A.4
(−2) Psychotic disorder, not otherwise specified. There is no evidence of psychosis or psychotic behaviors including hallucinations, delusions, or disordered thought processes.
A.5
(+1) ADHD. This is a likely comorbid disorder but does not fully explain all of the current symptoms.
Consideration Point B
B.1
(−2) Transfer care to an English-speaking provider whose schedule may be a better fit for the mother. This option would fail the principles of culturally competent care of children and adolescents.
B.2
(+3) Arrange for a meeting with the patient’s mother to obtain further collateral information and discuss treatment options. He is still an adolescent and not an adult, so this is mandatory and it is a best practice.
B.3
(−2) Discuss the possibility of having the patient’s Spanish-speaking primary care provider prescribe the medications for him. This family would benefit from receiving care at a psychiatric clinic, given the complexity of related factors and the need for coordination of services.
Consideration Point C
C.1
(+1) Ethnopharmacological factors that could affect the patient’s response to medications. Ethnopharmacological factors are important considerations when prescribing medications but should not be the only consideration.
C.2
(+1) Cultural beliefs about the patient’s illness and treatment. Similarly, assessing the family’s beliefs and attitudes toward illness and treatment is an important part of the clinician-patient encounter, but further considerations should be taken into account.
C.3
(+2) Immigration history of the family, including circumstances that led to migration, trauma exposure, acculturation issues, and current supports for all family members. A comprehensive evaluation and understanding of the role of the immigration process in the family’s current functioning, in addition to other issues, would be necessary.
C.4
(−3) No cultural factors pertinent for this case. Cultural, racial, and religious aspects should be explored during all clinical encounters as part of a good practice.
C.5
(+3) C.1, C.2, and C.3. All three options include factors that should be evaluated and included in the clinical assessment.
Conclusions
In 1999, a supplement to
Mental Health: A Report of the Surgeon General emphasized the existence of striking disparities for minorities in mental health services and the role that cultural factors play in mental health (
1). APA and other organizations have highlighted these issues and the importance of providing culturally sensitive mental health care to our patients.
DSM-5 includes cultural aspects throughout the manual as well as the Cultural Formulation Interview, which aims to help clinicians explore cultural and religious factors in their patient encounters and when conceptualizing the presentation of symptoms. According to the American Academy of Child and Adolescent Psychiatry’s Practice Parameter for Cultural Competency in Child and Adolescent Psychiatric Practice, providers caring for children and adolescents from diverse populations should pay special attention and give consideration to cultural and racial factors relating to mental illness and emotional disturbances (
2,
3).
The vignette presented above illustrates some of the American Academy of Child and Adolescent Psychiatry’s principles of cultural competence and the importance of information included in the Cultural Formulation Interview in DSM-5. Special considerations when treating diverse populations and immigrants include assessing the impact of dual-language competence, immigration-related trauma, and issues of acculturation of the patient and family, among others. The American Academy of Child and Adolescent Psychiatry recommends that providers make special efforts to include family members in the evaluation and conduct evaluation in the language in which they are proficient. The assessment of the family is essential for optimal treatment of children and families. Historical elements and family history should be gathered from caretakers. Furthermore, an evaluation of family communication, dynamics, and factors that could be precipitating and perpetuating symptom presentation is essential. In the case above, generational trauma, disruption of attachment, and family dynamics must be evaluated and assessed to provide adequate care to the family.