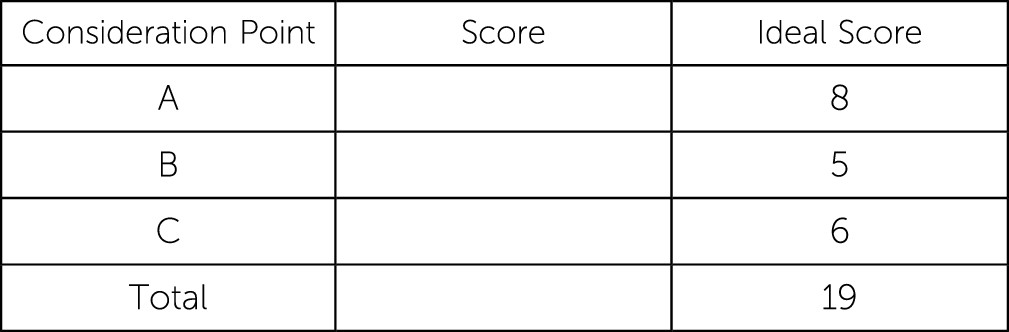
This exercise is designed to test your comprehension of material relevant to this issue of Focus as well as your ability to evaluate, diagnose, and manage clinical problems. Answer the questions below to the best of your ability with the information provided, making your decisions as if the individual were one of your patients.
Questions are presented at “consideration points” that follow a section that gives information about the case. One or more choices may be correct for each question; make your choices on the basis of your clinical knowledge and the history provided. Read all of the options for each question before making any selections. You are given points on a graded scale for the best possible answer(s), and points are deducted for answers that would result in a poor outcome or delay your arriving at the right answer. Answers that have little or no impact receive zero points. At the end of the exercise, you will add up your points to obtain a total score.
The following vignette is designed to test the reader’s comprehension of the subject of this issue of Focus as well as enhance the reader’s ability to incorporate culturally relevant issues into the diagnostic and treatment plan.
Case Vignette
Dr. M, a Caucasian physician, has been providing mental health services in a small college town for the past 20 years. He leads psychiatric rounds at the local hospital and treats outpatients in the school. Dr. M has been asked to evaluate Anil, an 18-year-old Indian-American college freshman, at an initial visit. Anil was referred to the clinic after an incident in which he appeared to be confused in class. The leading diagnosis was substance intoxication.
During the initial visit, Anil presents as a nervous-looking young man who appears uncomfortable in the clinical setting. He reports that he is unsure why his psychiatric evaluation was recommended. Dr. M notes that Anil is reticent and not forthcoming when talking about himself. Anil reports that he was born in Virginia to first-generation immigrant parents from India. His father is an ophthalmologist and his mother is a homemaker. His parents currently live in his hometown, which is about two hours away from college. The patient is the youngest of three children and was raised in a strict Hindu sect, where indulgence in alcohol or other substances is considered inappropriate and unseemly behavior. Anil describes his parents as supportive and says that he had a good childhood. There is no history of abuse by his family; Anil states he was lucky to be born into such a loving family. He notes with pride that his older sister works as an economist at the World Bank and his brother had recently been accepted into medical school. Anil reports his parents always stressed the value of hard work and the importance of setting career goals. During the interview, Anil becomes tearful and has difficulty speaking. With Dr. M’s encouragement and support, Anil says that unlike other members of his family, he is a failure and has always known that he was not as smart as his siblings. Whereas they have always been straight-A students, he has had to work hard to match their performance. He had to forgo extracurricular activities such as art to focus on grades. He was taking standard, not advanced-level, classes in high school and, ultimately, Anil graduated with “only” a 3.4 grade point average. Unlike his siblings, he was not accepted into an Ivy League college. He feels that he has disappointed his parents, particularly his father. His father expects his sons to join his practice one day. Of note, when Anil was a young child, he secretly nurtured a desire to pursue a career as an interior decorator, but he has never expressed this wish to his family.
Anil reports that for the past two years, he has experienced worry and an inability to relax during stressful situations such as test taking. In addition, he complains of headaches and diarrhea. All of these symptoms have worsened since coming to college seven months ago.
Later in the interview, Anil endorses worries about his grades, difficulty concentrating, restlessness, and low energy. Sometimes, he finds himself worrying about random issues, such as his parents’ health, even when there is no reason for concern. Anil admits to insomnia mostly stemming from racing thoughts. In addition, he describes depressed mood, anhedonia, and low motivation. He has not experienced changes in appetite or weight. Anil denies having any thoughts of self-harm. Although Anil has not had any panic attacks in recent months, he states that he has had them in the past. Anil’s last panic attack occurred a year ago while he was waiting for his college acceptance letters.
Anil reports that in the past month, he started smoking marijuana two to three times a week and in the past week he has used it daily. He also states that he has consumed a few beers occasionally when using marijuana. He reports that marijuana makes him feel less anxious. He denies experiencing blackouts and withdrawal symptoms from alcohol. He feels guilty about using these substances because he thinks he is letting his family down.
At the end of the interview, Dr. M determines Anil is not acutely at risk to himself or others. In addition, Anil has no history of suicide attempts; no family history of suicide or mental illnesses; no access to weapons; and no recent or past risky or dangerous behaviors, threats, or acts. Dr. M also has recent lab work from Anil’s primary care physician (PCP), which is noncontributory to the case.
Consideration Point A.
Initial diagnostic considerations should include which of the following?
A.1
Cannabis-induced anxiety disorder
A.2
Generalized anxiety disorder (GAD)
A.3
Major depressive disorder
A.5
Attention-deficit hyperactivity disorder
Case Vignette Continues
Upon further evaluation, Dr. M concludes that Anil has GAD comorbid with mild depression. He prescribes escitalopram 10 mg once daily and recommends cognitive-behavioral therapy. In addition, Dr. M engages the patient in motivational interviewing and psychoeducation for cannabis misuse, even though Anil does not meet criteria for a substance use disorder. Two weeks later, Anil returns to report that he is less ruminative, his sleep has improved, and he has abstained from alcohol and marijuana. He continues to feel guilty that he has disappointed his parents and experiences a sense of worthlessness at not having lived up to their expectations. He also reveals that since middle school, he has known that he is not attracted to women. A few months ago, when he first came to college, he had an intimate relationship with another male. He confided in his sister who, although supportive, had expressed fear of their parents’ reaction to the news. Subsequently, Anil broke off the relationship. In addition, he is worried about how his sexual orientation will affect his relationships within the Indian community. In this subsequent appointment, he tearfully asks, “Why am I like this? Am I being punished for what I did?”
Consideration Point B.
What is the most important next step that should be considered in the treatment formulation at this point?
B.1
Asking culturally sensitive questions
B.2
Increasing the dose of escitalopram
B.3
Acknowledging cultural differences between the psychiatrist and the patient