This exercise is designed to test your comprehension of material presented in this issue of Focus as well as your ability to evaluate, diagnose, and manage clinical problems. Answer the questions below, to the best of your ability, on the information provided, making your decisions as you would with a real-life patient.
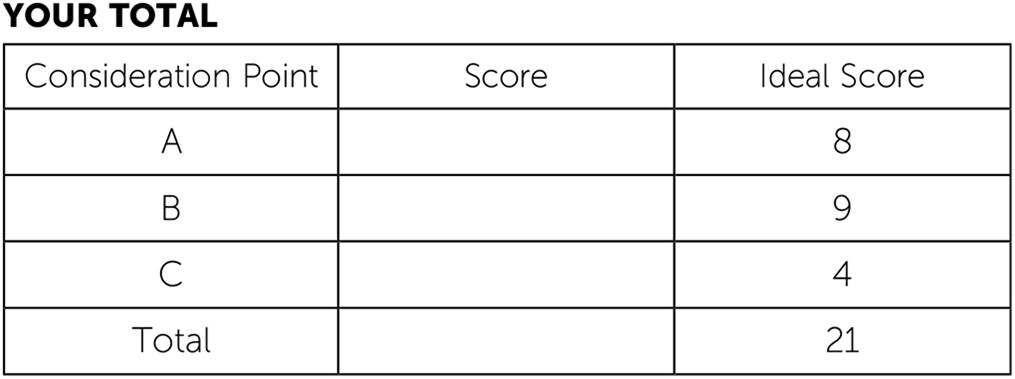
Questions are presented at “consideration points” that follow a section that gives information about the case. One or more choices may be correct for each question; make your choices on the basis of your clinical knowledge and the history provided. Read all of the options for each question before making any selections. You are given points on a graded scale for the best possible answer(s), and points are deducted for answers that would result in a poor outcome or delay your arriving at the right answer. Answers that have little or no impact receive zero points. At the end of the exercise, you will add up your points to obtain a total score.
Case Vignette
Peter Washington is a 68-year-old male veteran of the Vietnam War who was referred to you by his primary psychiatrist at the local Veterans Affairs (VA) health facility for a second opinion consultation regarding the management of a persistent irritability in the context of bipolar disorder and posttraumatic stress disorder (PTSD).
The documents that you were given to review report that he had his first manic episode while stationed overseas in the service; he had returned from a combat mission involving near capture by the enemy, several firefights, and many casualties, and then became energized and paranoid after several nights of sleep deprivation and ran naked through the base wearing only his hat and sidearm holster. At that time, he was treated emergently by the base medical staff and soon thereafter was returned to the United States and separated from the military, with service-connected disability benefits for bipolar disorder.
The patient’s medical records document multiple episodes of depression (including one bout of suicidal ideation necessitating hospitalization) and several episodes of mania in the 15 years after he returned to civilian life and his acknowledgment that he “did some pretty heavy drinking” during that period, although he denied using any other drugs of abuse.
The notes describe that he was eventually placed on a regimen of lithium and fluoxetine in the late 1980s. The records indicate that he then appeared to do reasonably well for many years: He got married, began to work as an electrician, and was able to hold a steady job, although he was in and out of Alcoholics Anonymous during that period for continued intermittent drinking problems. The notes also report that he becomes perturbed and agitated by fireworks at July 4th celebrations and avoids crowded places where points of egress are limited and that in the past he had been given a diagnosis of agoraphobia.
Case Vignette Continues
The chart elaborates that mood instability returned beginning in October 2001, followed by bouts of intoxication in 2002 and 2003 (never requiring hospitalization). At that point, the patient was switched to divalproex as his primary mood stabilizer; although his mood slipped occasionally into periods of depression, none of these required hospitalization, and he was generally able to maintain employment. After several years, he had a trial of aripiprazole when a prolonged bout of depression forced him to stop working, and eventually he was restabilized with lamotrigine and resumed employment. His mood has been generally stable on that medication since 2015, but since late 2016 he has found himself to be increasingly irritable, even when not depressed or manic.
When the patient came to your office for interviewing, he expanded on the remote history, noting that “most of the 1970s and early 1980s were a blur, with too much time drinking and blacking out.” He confirmed that, after many false starts in the 1970s marked by nonadherence to lithium, with sobriety he became consistent in taking lithium and then fluoxetine, which was added in 1989. He said, “With the help of my sponsor and my higher power, I turned my life around.” He confirmed that he had “straightened out,” gotten married to a woman he had known since high school, and had been gainfully employed as an electrician for many years. “I helped my union—the Brotherhood of Electrical Workers—organize our annual spring bowling tournament.” He confirmed that he had been trialed on divalproex and then aripiprazole before his current treatment with lamotrigine. He noted that “9/11 was hard on me” but did not elaborate further.
He confirmed that he had been doing well with lamotrigine until fall 2016. He acknowledged in retrospect that he had been bothered by the increasingly divisive rhetoric of the political campaigns even before then. He reported increasing levels of worry about how “everything is falling apart,” which he explained covered his worries ranging from the state of the environment to the geopolitical situation with U.S. military involvement in the Middle East and Asia. Concerns about the North Korean regime’s nuclear capabilities had begun to make it hard for him to sleep at night. He reported, “I haven’t told them about this at the VA, but sometimes I feel like I’m back in ’Nam . . . never knowing who’s friend or foe. I’ve gotta be on my toes all the time—back then, we never knew when the next attack might come, and it feels a lot like that today.”
He reported that he has been increasingly tense since early in 2017. He expressed his perspective on the reports of increased irritability by sharing, “I’ve got a short fuse these days . . . I’ll snap at my wife or yell at people at work. . . . At work they might deserve it a little, but my reactions are way out of proportion. My supervisor’s talked to me about it more than once.” He stated that he has occasional nightmares about narrowly avoiding being captured during combat, similar to experiences he had while in the military, although in his dreams his captors are wearing American police uniforms rather than those of the Viet Cong; he reported that he awakens “drenched in a cold sweat, with my heart racing.” He reported it may take an hour or more to fall back asleep.
On examination, the patient was pleasant and cooperative, casually attired and neatly groomed. Moderate psychomotor agitation was noted, with an excess of spontaneous movement. Eye contact was adequate, but his gaze occasionally shifted around the room. Speech was of normal volume, rate, and prosody. Affect was somewhat anxious and apprehensive. He characterized his mood as “irritable at times—mostly OK, and definitely not like when I’ve been depressed or manic before.” His thought process was of normal rate and organization, but he frequently returned to themes of “it’s a scary world” and of social injustice. His thought content was free of hallucinations or current suicidal or homicidal intent; he denied any intention or plan of suicide or other self-injurious behaviors. He did not endorse clear delusions but held as central ideas his fears that “Korea’s gonna drop nukes on us” or “we’re becoming a police state, like what we fought against in ’Nam.” Cognitively, he was awake, alert, and oriented to person, place, date, and circumstances. Memory registration was intact with three out of three stimuli, and recall after delay was three out of three items. He was able to spell world forward and backward accurately. He had no difficulty repeating the phrase “no ifs, ands, or buts.” His insight was intact, in that he recognized that he was easily frustrated and agitated, he needed treatment, and although his mood was stabilized with medications, he was still excessively irritable. His judgment was intact, in that he was seeking care, wished to return to wellness and be able to work, and was able to contemplate potential risks and side effects and anticipate benefits of additional treatments. No tremors or involuntary movements were noted. He had some mild swaying when standing with his eyes closed. His gait was unremarkable.