Virtual reality (VR) technology has undergone a transition in the last 20 years that has taken it from the realm of “expensive toy” into that of functional technology. These advances stand to offer new opportunities for clinical research, assessment, and intervention in the field of psychiatry. Since the mid-1990s, clinicians and researchers have developed VR-based testing, training, teaching, and treatment approaches that would be difficult, if not impossible, to deliver with traditional methods.
During this time, a large (but still maturing) scientific literature has evolved regarding the outcomes and effects from the use of what we now refer to as clinical VR. Such VR simulation systems have targeted the assessment and treatment of cognitive, psychological, motor, and functional impairments across a wide range of clinical health conditions. Moreover, continuing advances in the underlying enabling technologies for creating and delivering VR applications have resulted in its widespread availability as a consumer product, sometimes at a very low cost.
This article provides an introductory definition of the technology, charts its historical development generally and as a clinical tool, provides a detailed use case for VR in the treatment of anxiety disorders and posttraumatic stress disorder (PTSD), and discusses the issues for its use in psychiatry. We do not review the growing literature across all the areas of clinical implementation but instead cite the major papers that review that work. Our intention is to provide a road map for those interested in learning more about this emerging and potentially transformative technology.
What Is VR?
The concept and definition of VR have been subject to debate by scientists and clinicians over the years. VR has been very generally defined as a way for humans to visualize, manipulate, and interact with computers and extremely complex data (
1). From this baseline perspective, VR can be seen as an advanced form of human-computer interaction (
2) that allows a user to more naturally interact with computers beyond what is typically afforded by standard mouse-and-keyboard interface devices. Moreover, some VR formats enable users to become immersed in synthetic computer-generated virtual environments.
However, VR is not defined or limited by any one technological approach or hardware set-up. An engaged VR user experience can be created through combinations of a wide variety of interaction devices, sensory display systems, and content presented in the virtual environment. Thus, there are three common variations for how VR can be created and used.
Nonimmersive VR is the most basic format and is similar to the experience of playing a modern computer or console video game. Content is delivered on a standard flat-screen computer monitor or TV, with no occlusion of the outside world. Users interact with 3D computer graphics variously using a game pad, joystick, basic mouse and keyboard, or specialized interface devices (e.g., treadmills, data gloves, and even handheld devices—e.g., the Nintendo Wii remote). Modern computer games that support user interaction and navigation within such 3D worlds, even though presented on a flat-screen display, can be technically referred to as VR environments.
Immersive VR can be produced by the integration of computers, head-mounted displays (HMDs), body-tracking sensors, specialized interface devices, and 3D graphics. These set-ups allow users to operate within a computer-generated simulated world that changes in a natural or intuitive way on the basis of a user’s motion and interaction. An HMD occludes the user’s view of the outside world while using head- and body-tracking technology to sense the user’s position and movement. It simultaneously sends that information to a computing system, which then uses those data to update the sensory stimuli presented to the user. The contingent tracking of user activity and nearly real-time updating of the 3D content is said to create an immersive virtual experience. This serves to create the illusion of being immersed in a virtual space, in which users can interact. When users are immersed in computer-generated visual imagery and sounds of a simulated virtual scene, their interaction produces an experience that corresponds to what they would see and hear if the scene were real.
Another, less-common method for producing immersive VR experiences uses stereoscopic projection screens arrayed around a user in various configurations. In one approach, six-walled projection rooms known as cave automatic virtual environments (
3,
4) allow for interaction in a less-encumbered, wide-field-of-view simulated environment for multiple concurrent users. However, such systems are more costly and complex and are typically beyond the practical resources of most clinical service providers and basic researchers.
Regardless of the technical approach, the key aim of these immersive systems is to perceptually replace the outside world with the virtual world to psychologically engage users with simulated digital content designed to create a specific user experience. Immersive VR (most commonly delivered in an HMD) is typically the choice for applications for which a controlled stimulus environment is desirable for constraining a user’s perceptual experience within a specific synthetic world. This format has been often used in clinical VR applications for anxiety disorder exposure therapy, as analgesic distraction for patients undergoing acutely painful medical procedures, and in the cognitive assessment of users to measure performance under a range of systematically delivered challenges and distractions.
A Brief History of Clinical VR
VR has recently captured the public’s imagination as the next big thing in media. However, the technology for creating VR experiences and VR’s clinical use has existed for at least two decades. During the 1990s, the growing availability and rapid evolution of personal computing drove the global adoption of innovative digital technologies for the purposes of productivity enhancement, communication, and social interaction. At the same time, the advances in modern computing power required to automate processes and to store and analyze vast quantities of data did not go unnoticed by clinical researchers and providers, who imagined and prototyped novel behavioral health-care applications. Primordial efforts from this period can be seen in developments that aimed to use personal computers to enhance productivity in patient documentation and record keeping, automate the administration and scoring of psychometric tests, and allow for computer delivery of cognitive training and rehabilitation activities (
5). As well, with the rapid improvements in Internet connectivity seen during the 1990s, researchers and clinicians explored the idea of enhancing access to care through Internet-based teletherapy (
6–
9) and self-help cognitive-behavioral programs (
10,
11).
Since that time, the impact of computer and information technology on society has grown dramatically. This can be seen in the current adoption of and growing demand for mobile devices, high-speed network access, smart televisions, social media sites, photorealistic digital games, wearable behavioral-sensing devices, and now the “second coming of VR.” Such consumer-driven technologies, although thought of as visionary just ten years ago, have now become increasingly common and essential fixtures in the digital landscape of modern society.
The idea of using VR for clinical purposes was first recognized in the early- to mid-1990s with initial efforts to design VR simulations to deliver exposure therapy for specific phobias (e.g., fear of heights, flying, spiders, and public speaking) (
12,
13) and for cognitive assessment and rehabilitation (
14–
17). The compelling feature that drove this innovation was the idea that VR could leverage computing beyond its cardinal purpose—the automation of processes—to instead use computers to produce and deliver sensory stimuli for the creation of embodied, interactive, and immersive user experiences. This was recognized early in the visionary article “The Experience Society” by VR pioneer Myron Krueger (
18), in his prophetic statement that “Virtual Reality arrives at a moment when computer technology in general is moving from automating the paradigms of the past, to creating new ones for the future” (p. 163). Viewed from this perspective, VR affords the opportunity to create highly realistic, interactive, and systematically controllable stimulus environments that users can be immersed in and interact with for human performance measurement and training as well as for clinical assessment and intervention. Clinicians and scientists who were drawn to the idea of VR during this time were often guided by the belief that its core features and assets could support the development of innovative clinical approaches that were not possible with existing traditional methodologies.
The added value for such VR systems can be seen in the technology’s capacity to create systematic human testing, training, teaching, and treatment environments that allow for the precise control of complex, multisensory, dynamic 3D stimulus presentations. Within such simulations, sophisticated behavioral interaction is possible, and researchers can precisely track, record, and analyze such physical activity to study human performance and behavior. Much like an aircraft simulator serves to test and train piloting ability under a wide variety of controlled conditions, VR can be used to create relevant simulated environments in which the assessment and treatment of cognitive, emotional, and sensorimotor processes can take place under stimulus conditions that are not easily deliverable and controllable in the physical world.
When combining VR’s stimulus control features with the ability to immerse users in functional and ecologically relevant virtual environments, early clinical VR scientists envisioned a fundamental advancement in how human assessment and intervention could be addressed. One could conjecture that this “ultimate Skinner box” perspective was what human experimental researchers and clinicians had always strived for, but they were limited by the constraints imposed by the laws of physics that govern physical reality. This “vision” drove the enthusiasm and innovative efforts seen in the fledgling area of clinical VR in the 1990s.
Unfortunately, many technical challenges needed to be overcome before this vision of clinical VR could be achieved. When discussion of the potential use of VR for human research and clinical intervention first emerged in the 1990s, the technology needed to deliver on this vision was not sufficiently mature. Consequently, during these early years, VR suffered from a somewhat imbalanced “expectation-to-delivery” ratio, as most who explored VR systems during that time will attest. Computers were too slow; 3D graphics were primitive; and user-interface devices were awkward, requiring more effort than users were willing to expend to learn how to operate them effectively. Moreover, VR HMDs were costly and bulky, and they had limited tracking speed, resolution, and field of view. As a consequence, VR commenced its “nuclear winter” period in 1995, as the public became disenchanted with the quality of a typical VR experience and generally viewed it as a failed technology. Thus, VR languished for many years in what the Gartner Group has termed “the trough of disillusionment,” the stage in technology adoption that often follows the “peak of inflated expectations” period, as described in their regularly updated “Hype Cycle for Emerging Technologies” (
19).
Regardless of these technical challenges, the core vision of clinical VR was sound, and VR “enthusiasts” continued to pursue the research and development needed to advance the technology and document its added clinical value. Over the last 23 years, the technology for creating VR systems gradually caught up with the vision of creating compelling, usable, and effective clinical VR applications. This has been possible in large part because of the gradual but continuous advances in the underlying VR-enabling technologies and methods (e.g., computational speed, computer graphics, panoramic and spherical video, audio-visual-haptic displays, 3D-user interfaces, tracking sensors, speech and language processing, artificial intelligence, virtual human agents, authoring software).
Such advances have resulted in the technical capability needed to support the creation of low-cost yet sophisticated immersive and interactive VR systems capable of running on commodity-level computing devices. In part driven by the digital gaming and entertainment sectors, as well as by a nearly insatiable global demand for mobile and interactive networked consumer products, these advances in technological “prowess” and accessibility have provided the hardware and software platforms needed to produce more adaptable and high-fidelity clinical VR scenarios. This has created a state of affairs in which clinical VR applications can now usefully leverage the interactive and immersive assets that VR affords as the technology continues to get faster, better, and cheaper moving forward into the 21st century.
Moreover, since the 1990s, a significant scientific literature has evolved, almost under the radar, reporting many positive outcomes across a range of clinical applications that have leveraged the assets provided by VR (
20–
32). A short list of the areas in which clinical VR has been usefully applied includes fear reduction among persons with specific phobias (
26,
33–
35); treatment for PTSD, depression, and paranoid delusions (
20,
27,
30,
36–
46); addiction treatment (
47); discomfort reduction among cancer patients undergoing chemotherapy (
48,
49); acute pain reduction during wound care and physical therapy with burn patients (
23) and in other painful procedures (
50–
53); improvement of body image disturbances among patients with eating disorders (
54); navigation and spatial training for children and adults with motor impairments (
55–
57); functional skill training and motor rehabilitation for patients with central nervous system dysfunction (e.g., stroke, traumatic brain injury, spinal cord injury, cerebral palsy, multiple sclerosis) (
24,
58–
63); and the assessment and rehabilitation of attention, memory, spatial skills, and other cognitive functions in both clinical and unimpaired populations (
14,
16,
17,
31,
64–
71).
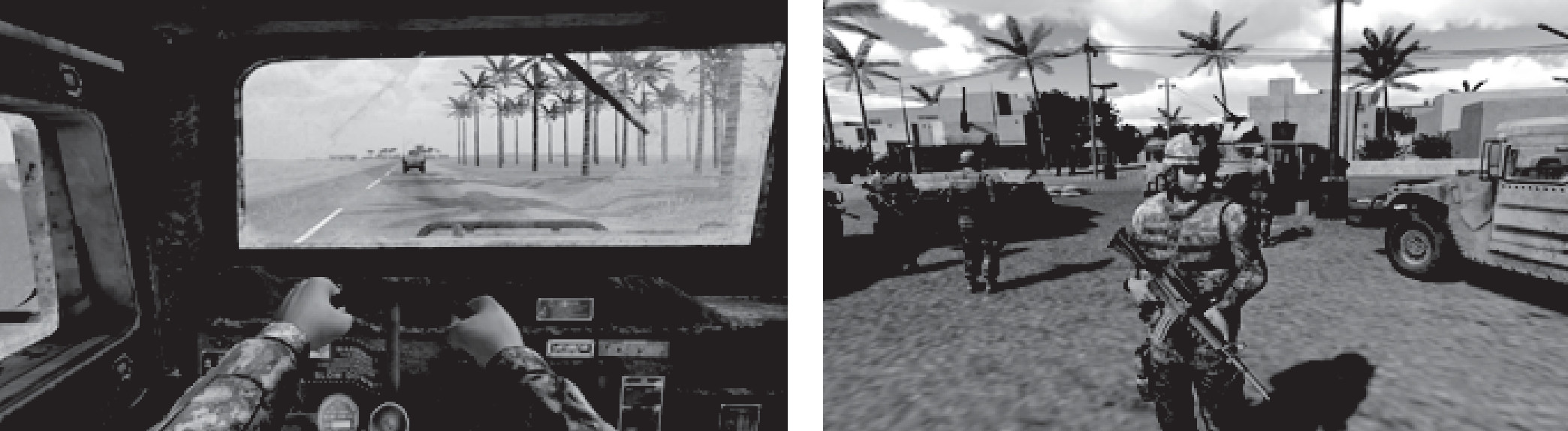
For these varied purposes, clinical VR scientists have constructed virtual airplanes; skyscrapers; spiders; battlefields; social settings; beaches; fantasy worlds; and the mundane (but highly relevant) functional environments of the schoolroom, office, home, street, and supermarket. In essence, clinicians can apply VR environments mimicking real or imagined worlds to engage users in simulations that support the aims and mechanics of a specific clinical assessment or therapeutic approach. As a result, there is a growing consensus that VR has now emerged as a promising tool in many domains of research (
72,
73) and clinical care (
29,
41,
61,
74,
75).
What makes clinical VR so distinctively innovative is that it represents more than a simple linear extension of existing computer technology for human use. Because of VR’s capacity to immerse a user in an interactive computer-generated simulation, new possibilities exist that can go beyond the simple automation of previous clinical assessment and intervention approaches. Nevertheless, in deciding whether VR is ready for clinical use, one needs to consider what features VR offers that may make it especially suited for addressing the requirements of clinical and research usage (cf.
29).
On a very general level, VR can be seen to foster core processes that are relevant across a variety of clinical domains. These processes can be briefly summarized as expose (e.g., exposure therapy for anxiety disorders, PTSD, or addiction treatment), distract (e.g., distract attention away from painful medical procedures to reduce pain perception or promote discomfort reduction), motivate (e.g., motivating patients in cognitive or physical rehabilitation to perform repetitive and sometimes boring tasks by embedding those tasks in gamelike contexts), measure (e.g., measuring performance on physical and cognitive assessment activities), and engage (e.g., generally seen as captivating attention or action, which is useful for engaging participation with clinical applications).
Most clinical VR applications leverage two or more of these core processes. To illustrate this in the context of VR applications relevant in psychiatry, we detail a use case directly relevant to psychiatry—exposure therapy for anxiety disorders and PTSD. For readers interested in other areas of clinical VR usage, the literature cited in the introduction should provide a current road map for exploring a wider range of clinical applications in more detail than possible in this more focused article.
Discussion and Conclusions
General simulation technology has a long history of adding value in aviation training; military planning; automotive, equipment, and architectural design; and robotic surgery practice (
113). When researchers leverage these same simulation technology assets, but in a form factor that can deliver VR experiences in a clinicians’ office, hospital, or research laboratory, a powerful and engaging set of virtual tools for psychiatric applications becomes available. The initial step for creating useful VR simulations for clinical purposes is to first look at known processes operating in physical reality that are based on existing theory and are thought to underlie evidence-based approaches to assessment and intervention. With that as a starting point, one can thoughtfully specify the simulation assets required to create VR applications that can amplify treatment effects, provide more reliable and valid diagnostic assessments, break down barriers to care, or simply reduce costs by automating processes.
For example, we know that the use of imaginal exposure therapy for anxiety disorders and PTSD is evidence based in the physical world. From that, one can see a direct case for using the virtual world to deliver ecologically relevant simulations, within which stimuli can be precisely controlled. This allows for the titration of progressively more provocative stimuli designed to pace exposure for the end goal of promoting extinction learning and subsequent fear and anxiety reduction.
Similarly, we know that the sheer amount of physical rehabilitation activity that a stroke survivor engages in is related to improved functional outcomes (all other factors being equal). From that, it is logical to hypothesize that if compelling game-based VR rehabilitation tasks are developed, it might be possible to motivate users to do more repetitions, which could lead to improved outcomes. These thumbnail examples illustrate how a combination of the VR assets cited earlier (expose, distract, motivate, measure, and engage) can inform the rationale for clinical use cases that add value over existing traditional methods.
The research support for the use of clinical VR applications is also promising, albeit not fully mature. There seems to be consensus in the literature that VR can produce equivalent or better outcomes for exposure-based approaches for anxiety disorders and PTSD treatment (
25–
27,
114). As well, in other areas of clinical VR application, consistent findings have been produced in support of VR as an effective distraction tool for reducing the perception of pain among patients undergoing acutely painful medical procedures (
23,
53). A growing body of research indicates that VR can increase participation in physical rehabilitation, with patients reporting more motivation to engage in rehabilitation tasks in a game-based VR context, as compared with traditional rehabilitation approaches (
115). Cognitive assessment methods using VR have enhanced performance measurement, producing promising results in construct validation studies and for distinguishing between clinical groups and healthy controls (
70,
116–
118). Finally, virtual humans with varying levels of artificial intelligence have been shown to engage users in credible interactions in support of clinical training (virtual patients), as always-available and tireless health-care guides, and recently in the role of clinical assessors (
22,
119–
126).
As we look to the future, we see clinical VR as one of the larger domains of general VR usage. In the recent Goldman Sachs (
74) market analysis looking at the future of VR in 2025, the gaming and entertainment sector of course garnered the largest market share. Although this is to be expected, given the public’s chronic demand for new and better ways to consume media, the little-noticed item in that market analysis is that health care came in second place for the VR market share. This is not a surprise to researchers and clinicians who have worked in this area over the years, especially as we see health-care costs becoming one of the largest line items in the U.S. government’s budget, after defense.
Interest in clinical VR by actual therapists also seems to be substantial and growing. Norcross et al. (
75) surveyed 70 psychotherapy experts regarding interventions they predicted to increase in the next decade. VR was ranked fourth out of 45 options, with other computer-supported methods (teletherapy, mobile apps, online cognitive-behavioral therapy self-help) occupying the other three of the top five positions.
Professional interest in the clinical uses of VR technology has clearly accelerated and will likely continue to be fueled by a societal zeitgeist in which this form of immersive and interactive technology inspires the public’s attention and imagination. Although it was previously hamstrung by costs, complexity, and clinician unfamiliarity with VR equipment, the technology has evolved dramatically in the consumer marketplace, with new low-cost, easily accessible, high-fidelity product offerings that are poised to drive wider scale adoption. This will result in a probable future scenario whereby VR headsets will become like toasters—although people might not use the headset every day, every household will have one. When such market penetration occurs, the general public will have more access to a range of VR experiences. This may serve to accelerate the uptake of clinical VR as users, more familiar with the technology, begin to imagine its value beyond the world of digital games and entertainment and come to expect it as a part of their health care.
The momentum generated by the growing public awareness of VR, coupled with advances in the science and technology, has created a unique opportunity for psychiatry. Our analysis of the history, theoretical basis, and research findings to date leads us to predict that the application of clinical VR will have a significant impact on future research and practice. Certainly there is still much work to be done to advance the science in this area, particularly with the need to dismantle studies to better specify active ingredients for promoting clinical improvements. Research also needs to better specify which patients will best derive value from a VR approach versus more traditional methods.
However, when one considers that psychology as a science has been around for about 125 years, with a focus on studying human behavior and interaction in the physical world, it only makes sense that we may need a few more years to evolve the science for how humans behave and interact in the virtual world. In view of the current enthusiasm for VR generally across society and specifically in the clinical community, coupled with emerging scientific support, we believe that it is a fairly safe bet that clinical VR applications will soon become standard tools in the toolbox of psychiatry researchers and practitioners and will only grow in relevance and popularity in the future. For access to a large library of online videos demonstrating many of the VR applications discussed here, go to
https://www.youtube.com/user/albertskiprizzo.