This exercise is designed to test your comprehension of material relevant to this issue of Focus as well as your ability to evaluate, diagnose, and manage clinical problems. Answer the questions below to the best of your ability with the information provided, making your decisions as if the individual were one of your patients.
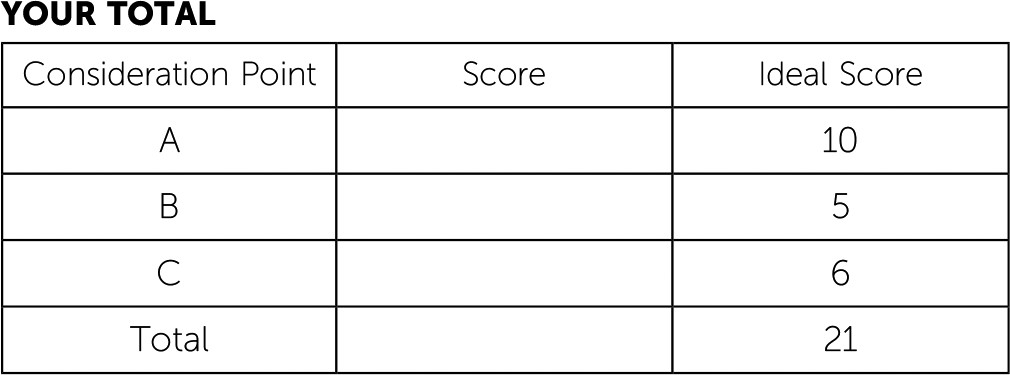
Questions are presented at “consideration points” that follow a section that gives information about the case. One or more choices may be correct for each question; make your choices on the basis of your clinical knowledge and the history provided. Read all of the options for each question before making any selections. You are given points on a graded scale for the best possible answer(s), and points are deducted for answers that would result in a poor outcome or delay your arriving at the right answer. Answers that have little or no impact receive zero points. At the end of the exercise, you will add up your points to obtain a total score.
This exercise describes the evaluation and treatment of a patient who has just received a diagnosis of bipolar disorder. Questions and answers examine the use of several agents in his treatment.
Case Vignette
You were covering emergency psychiatric services at the local hospital when the police brought in Mr. Sam Malone for involuntary evaluation and treatment. Mr. Malone was a 23-year-old man who came to the attention of the authorities when he was observed painting a mural on the exterior wall of a municipal building and roller skating wearing only underpants. He had not received authorization for the painting; when approached by police, he offered a rambling story about being guided by Zeus and ancient Grecian muses “to create art and to love one another.” The police said he was generally cooperative with being brought to the emergency department (ED) for care, although he maintained that the only thing wrong was that he was not being inspired that day.
You elicited further historical information from Mr. Malone in the ED. He reported that he had moved from his small hometown to the present city about two months prior, after seeing his twin sister act in a community theater performance of the musical
Xanadu (
1) and coming to believe that he needed to move to a larger city for inspiration. He reported that he had been interested in art since his teenage years and had studied art at a college in his hometown for a year before dropping out to paint and sculpt. He worked at a convenience store to support himself.
Mr. Malone reported that since moving to the city, he had felt “totally inspired by the energy.” He told you he had been living in low-cost single-room-occupancy hotels for the first month but now was living out of his car. He endorsed having little need for sleep yet feeling abundant energy, and he kept exclaiming “I’m alive!” to describe his excitement in life, almost with amazement. He endorsed smoking up to three joints of marijuana daily, which he felt had helped him to “stay mellow.”
Mr. Malone reported that he had talked with a counselor in high school “a couple of times” because he had felt “kinda moody after my folks died,” but he had never seen a psychiatrist, engaged in ongoing psychotherapy, or been prescribed psychotropic medications. He stated that both his parents had died six years previously in a car accident and that he and his sister had lived with an aunt and uncle until they finished high school. He gave you permission to call his sister for more history and to tell her that he was in the ED.
Case Vignette Continues
A call with Mr. Malone’s sister revealed that, indeed, he had always had an artistic bent that was underappreciated in his small hometown. She confirmed that the siblings saw their parents die in a motor vehicle accident, when their car was struck head on by a drunk driver. The twins were in the backseat, with their parents in the front, and their parents were declared dead at the scene.
Mr. Malone’s sister reported that their maternal aunt and her boyfriend had been “nice enough…when they weren’t high [on opiates]” and that they had provided a roof over the siblings’ heads and food but little emotional support or life guidance after their parents died. Both she and the patient had experienced nightmares for many months, but they had minimized their distress to others and had confided primarily in each other. The two had “that special twins-bond thing,” she noted. The sister was a year away from finishing her college degree as a communications major. She shared that her brother had been majoring in visual arts but “just didn’t click with college classes” and had dropped out.
She reported that her brother had been in good physical health, aside from smoking tobacco and occasional marijuana (“Maybe a joint twice a week”). She said she knew of no other substance use issues for her brother—no hallucinogens, alcohol, cocaine, psychostimulants, heroin, PCP, opiates, benzodiazepines, solvents, or other substances. She asked whether Mr. Malone was going to be admitted, and because he had given you permission to speak with her as his next of kin, you acknowledged that he was already on an involuntary hold for 72 hours.
You then returned to the patient’s room, where he was smiling and looking around intently. As you examined him, the patient was pleasant and cooperative, now wearing a hospital gown over his underwear. You noted prominent psychomotor agitation, with an excess of spontaneous movement. For example, he moved his legs in a pedaling motion when sitting still and shifted around on the gurney. Eye contact was intense. Speech was at a somewhat rapid rate but of normal volume and prosody. Affect was expansive and somewhat labile. Mr. Malone characterized his mood by saying, “I had been in that joyous flow state earlier, but this has all harshed my mellow.”
His thought process was rapid, with loosening of association, nonlinearity, and a preoccupation with specific ideas of reference and delusional beliefs. His thought content was free of suicidal or homicidal ideation but was focused on a belief that he had been inspired by ancient Greek muses who had come to life from a mural “just like in my sister’s show…that’s when I put it all together! I’m like Sonny Malone in the show, and my muse Clio is waiting for me to finish the mural so she can inspire me in the flesh.”
With respect to his cognitive state, Mr. Malone was awake, alert, and oriented to person and place, but he was off on the date by a few days. Memory registration was intact with three out of three stimuli, and recall after delay was correct for two out of three items. He was able to spell the word world forward and backward accurately. He had no difficulty repeating the phrase “No ifs, ands, or buts” but perseverated in repeating it frequently during the rest of the interview.
Mr. Malone’s insight was impaired in that he did not recognize the oddities of his beliefs and behaviors and that the ideas of reference related to the musical were unusual. His judgment was impaired, given that he had been roller skating in only his underwear and painting the mural “under the guidance of Zeus” without permission. You noted no tremors or involuntary movements.