Body Dysmorphic Disorder: Clinical Overview and Relationship to Obsessive-Compulsive Disorder
Abstract
Definition and Core Clinical Features of BDD
Diagnostic Criteria for BDD in DSM-5
Criterion A.
Criterion B.
| Lifetime | |
|---|---|
| Behavior or compulsion | rate (%) |
| Comparing disliked body parts with the same areas on others (e.g., in person, online, on television) | 88 |
| Checking disliked body areas in mirrors or other reflecting surfaces | 87 |
| Grooming (e.g., applying makeup; cutting, styling, shaving, or removing head hair, facial hair, or body hair) | 59 |
| Seeking reassurance about the perceived defects or questioning others about how they look (e.g., “Can’t you see this on my face?”) | 54 |
| Touching the disliked areas to check their appearance | 52 |
| Changing clothes (e.g., to camouflage disliked areas or find an outfit that distracts others from the “defects”) | 46 |
| Dieting (e.g., to make a “wide” face narrower) | 39 |
| Skin picking to improve perceived skin flaws | 38 |
| Tanning (e.g., to darken “pale” skin) | 25 |
| Excessive exercising | 21 |
| Excessive weightlifting | 18 |
Criteria C and D.
BDD Specifiers in DSM-5: Muscle Dysmorphia, Insight, and Panic Attacks
With muscle dysmorphia.
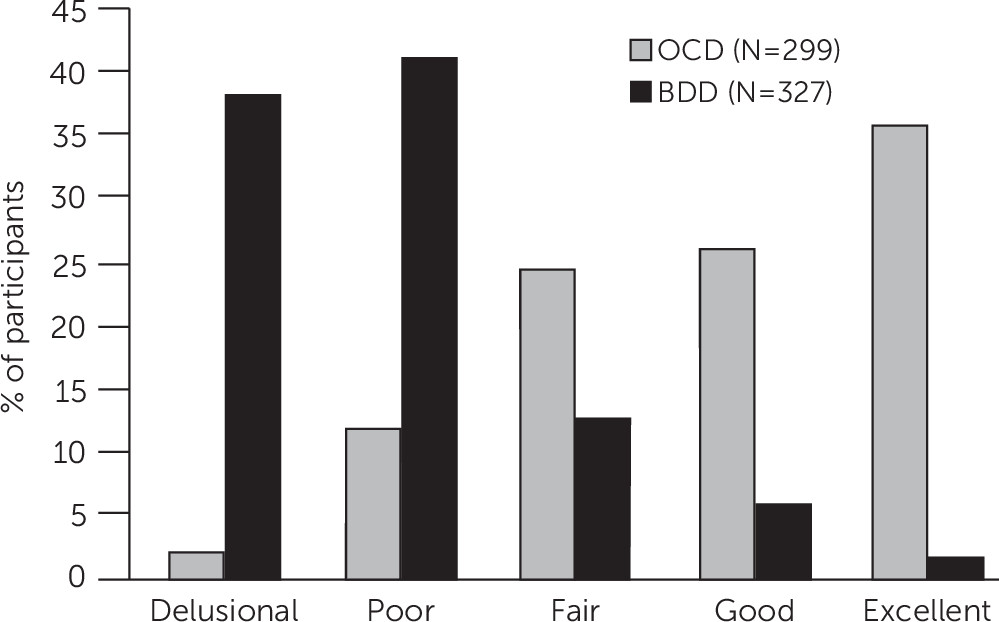
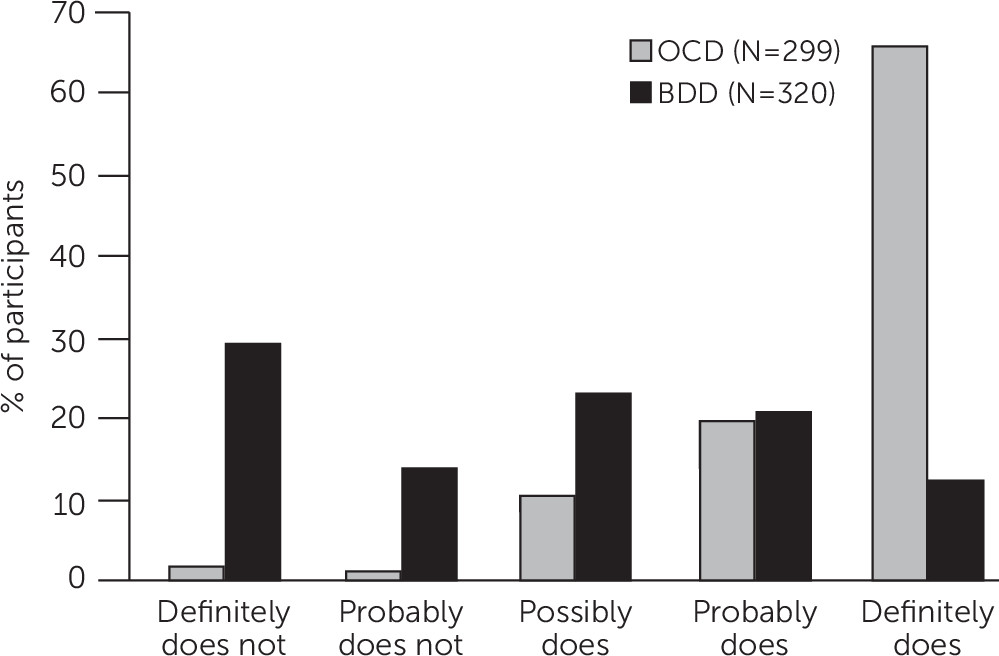
Insight.
With panic attacks.
Key Associated Features
Epidemiology
Age at Onset and Course of Illness
BDD Among Youths
Impairment in Psychosocial Functioning
Suicidality
Gender-Related Aspects of BDD
Major Depressive Disorder, Substance Use Disorders, and Other Comorbid Conditions
A Patient With BDD
Emerging Clues About BDD’s Etiology and Pathophysiology
Genetic Factors
Neurobiological Factors
Information-Processing Biases
Psychological and Social-Environmental Factors
Evolutionary Perspective
BDD’s Relationship to OCD and Other Disorders: Similarities and Differences
| Similarities | Differences |
|---|---|
| Unwanted, distressing obsessions and preoccupations | Different focus of obsessions, core beliefs, and compulsions (appearance focused in BDD) |
| Distressing repetitive behaviors (rituals, compulsions) that aim to reduce anxiety or distress | Some BDD repetitive behaviors (such as mirror checking) appear less likely to reduce anxiety and may increase anxiety and distress |
| Content of some obsessions and rituals, such as symmetry concerns, checking, and reassurance seeking | Poorer insight as well as more ideas and delusions of reference in BDD (and more paranoid personality disorder) |
| Similar BDD-YBOCS and Y-BOCS scores for individual scale items | More frequent comorbid major depressive disorder and substance use disorders in BDD |
| Most demographic features | More frequent suicidality in BDD |
| Often severe functional impairment and poor quality of life | Functional impairment may be more severe in BDD, particularly in education, employment, and other domains |
| High levels of perfectionism, high neuroticism, low extraversion | Possibly more childhood emotional and sexual abuse in BDD |
| Course of illness (often chronic) if not appropriately treated | Differences in translational studies (e.g., greater anger recognition bias and greater frequency of threatening interpretations of ambiguous social and appearance-related information in BDD) |
| Familiality | Poorer facial affect perception in BDD |
| Overlapping genetic vulnerability | Disorder-specific genetic effects and environmental influences |
| Abnormalities in frontostriatal systems, including hyperactivity on fMRI in orbitofrontal cortex and head of the caudate | More intensive strategies (e.g., motivational interviewing) may be needed to engage and retain patients with BDD in treatment |
| CBT as first-line psychosocial treatment (cognitive restructuring, ritual prevention, and exposure) | Differences in CBT: in BDD, more complex and often longer treatment, with greater focus on cognitive techniques and behavioral experiments; inclusion of perceptual retraining; if needed, use of habit reversal training for skin picking, hair plucking and pulling, and use of strategies to address desire for or use of cosmetic treatment; greater need to address depressive symptoms |
| SRIs as first-line pharmacotherapy (high doses often needed) |
How to Assess Patients for BDD
How to Differentiate BDD From Disorders With Which It Is Often Confused
OCD
Excoriation (Skin-Picking) Disorder
Trichotillomania (Hair-Pulling Disorder)
Major Depressive Disorder
Social Anxiety Disorder
Agoraphobia
Generalized Anxiety Disorder
Eating Disorders
Psychotic Disorders
Gender Dysphoria
Olfactory Reference Disorder (Olfactory Reference Syndrome)
Clearly Noticeable Physical Defects
Normal Appearance Concerns
Treatment of BDD
Treatment Challenges and How to Address Them
Surgical, Dermatologic, Dental, and Other Cosmetic Treatment
Pharmacotherapy
SRI efficacy.
SRI dosing.
SRI trial duration.
SRI augmentation and switching.
Non-SRI monotherapy.
CBT
CBT efficacy studies.
Components of CBT for BDD.
Session number and frequency.
Predictors of therapy response.
Combined Pharmacotherapy and CBT
Family Therapy
Approaches for Treatment-Refractory BDD
Conclusions and Future Directions
Footnote
References
Information & Authors
Information
Published In
History
Keywords
Authors
Competing Interests
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.