Consistent, high-quality suicide prevention care requires understanding that each episode of care is embedded within a broader context. A systems-level approach is needed to address the structural and cultural issues that create barriers to effective care and to provide solutions that fit real-world work pressures and environments. By shifting our perspective to see suicide as also an outcome of imperfect interactions with systems, we can identify problems and seek solutions that move us closer to the aspirational goal of zero suicides (
1,
2).
Care Example: Suicide Attempt After an Emergency Department (ED) Visit
The following example is a fictional composite developed from the authors’ experiences. Although this example is situated in an ED, the opportunities for improvement identified here can be found in many other health care contexts.
Danny, a 34-year-old male agricultural worker, sought care at an ED, reporting “feeling overwhelmed” by financial pressures and having thoughts of suicide. The nurse who assessed Danny determined that safety precautions during the visit were necessary. The ED physician evaluated Danny and then sought a consultation for a mental health evaluation. The long wait, bright lighting, loud noises, and his interpretation of staff behavior as callous left Danny feeling increasingly agitated. He asked several times for an update on when he would be seen, but the nurse provided little information, appeared irritated, and told him to wait patiently, because there were “a lot of sick people ahead of him.” This response increased Danny’s sense of isolation, burdensomeness, and hopelessness. Three hours later, an experienced licensed clinical social worker who was part of the consult liaison (C-L) team evaluated Danny. Danny’s fear of hospitalization, distrust of the staff, and exhaustion with the process led him to minimize his suicidal thoughts: he disclosed suicidal ideation and owning a firearm but did not report plans, preparatory behaviors, or intent to act. The consulting clinician discussed the situation with the ED physician, and together they determined that Danny did not meet the criteria for inpatient admission and should be discharged. The consulting clinician briefly confirmed this decision with the C-L psychiatrist on his team. The nurse completing the discharge provided Danny with a printed list of outpatient referral resources, contact information for a crisis line, and an information sheet about gun safety, but no safety plan, lethal means safety counseling, or appointment with a mental health provider—all best practices specified by the hospital’s protocols. Neither the C-L psychiatrist nor the ED physician checked to confirm that best practices had been followed. Two days later, Danny attempted suicide.
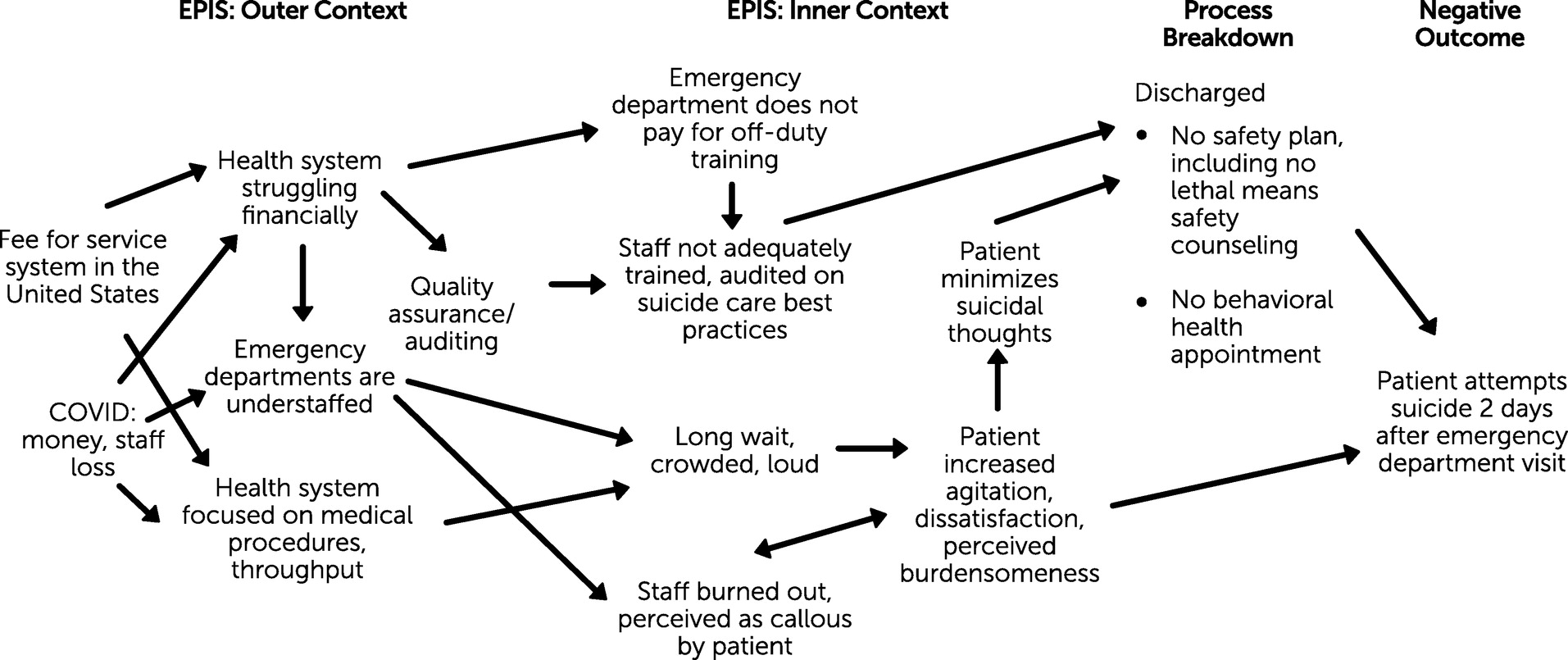
A Systems-Based Formulation Revealing Missed Opportunities
Traditional clinical “case” formulation focuses on individual psychopathology, stressors, and suicide risk. But if we widen the lens to consider the strengths and weaknesses of the systems with which an individual interacts, we can identify opportunities for improving suicide-related care. Borrowing from the field of implementation science, the following case presentation is informed by the constructs of outer and inner context, drawn from the EPIS (Exploration, Preparation, Implementation, and Sustainment) framework (
3). Inner context factors include organizational characteristics, quality and fidelity monitoring, department protocols, and staff characteristics (i.e., capacity, attitudes, degree of collaboration). Outer context factors include organizational leadership, service environment and policies, funding or contracting, and interorganizational environment and networks. These contexts broadly parallel proximal and distal factors in clinical formulations, allowing for the development of systems-based formulations of interactions between people receiving care and health care organizations. In this article, we treat the ED as the inner context—the “organization” referred to in the EPIS framework—whereas the outer context includes the broader health system to which the ED belongs, along with more distal external factors.
The hospital Danny visited had taken the important step of developing policy and procedures to require safety planning for people in the ED with identified suicide risk. Safety planning is an evidence-based practice (
4–
6) that involves collaboration with an individual at risk for suicide and their support persons. The goal is to identify person-specific distraction activities, coping strategies, and crisis support services the person can call on when warning signs occur, as well as to make the person’s environment safer through lethal means safety counseling. An obvious starting point for learning from Danny’s attempt is observing that this procedure was not followed. See
Figure 1 for an illustration of how we can identify further opportunities for improvement by widening the lens to examine inner and outer contexts.
Inner Context
The most proximal missed opportunity in Danny’s case was that staff did not engage Danny with safety planning. If we ask why, we find that the nurse who discharged Danny was insufficiently trained in this protocol. A combination of factors was at work. Because the ED does not pay for off-duty training, training is completed during already-busy shifts. Because training takes place around other activities and is provided through self-paced virtual modules, staff often click through the modules quickly. There is no opportunity for group discussion and development of norms around new practices. Furthermore, there is no performance auditing with feedback to ensure the learning outcomes have been met or that protocols are being implemented. Environmental factors, combined with staff attitudes reflecting work pressures, also contributed to Danny’s reluctance to disclose, with the extended wait leaving him feeling agitated, dissatisfied, and burdensome.
Outer Context
Distal factors also contributed to Danny’s suicide attempt. The health system is struggling financially, which is why paid, off-duty training is not provided. The manager responsible for training is overworked and unable to ensure that everyone is up to date with their training. There are no dedicated trainers or process improvement personnel, so the system cannot provide at-the-elbow training or auditing with feedback. A focus on profitable medical procedures and maximizing throughput affects which trainings and services are prioritized, leading to long wait times and a crowded ED. Some of these limitations originate in the fee-for-service model prevalent in the United States and the staffing and financial burdens caused by the COVID-19 pandemic, but similar concerns have been detected in countries with other health care financing models (
7).
It is impossible to say whether Danny’s suicide attempt would have been avoided if the implementation context had better supported the policy-mandated preventive measures. This systems-based formulation nevertheless identifies opportunities for improvement and reinforces awareness that suicide prevention is not the responsibility of any one role or individual. There is almost never a simple root cause for suicide or suicide attempts, nor a single care defect that is responsible. A systems-level approach is thus needed to respond to the range of factors identified.
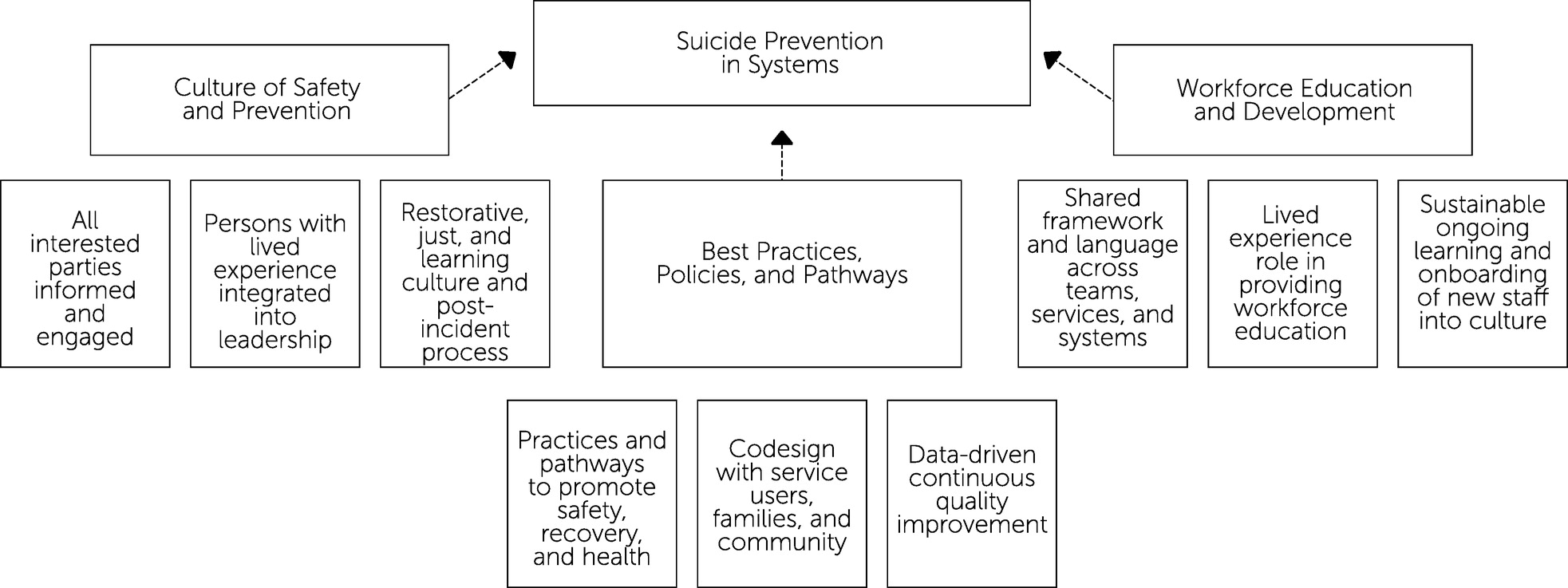
Suicide Prevention in Systems: Core Domains and Defining Characteristics
Figure 2 shows a systems approach to suicide prevention, with three mutually reinforcing core domains, each having three defining characteristics.
Figure 2 provides a conceptual map and a customizable outline for project planning. Implementation teams, including those that adopt the goal of Zero Suicide, can use the three defining characteristics to organize workstreams, a valuable project management tool (
8) for breaking down complex initiatives into manageable areas of activity. Organizing by workstreams fits with the goal of achieving suicide prevention in complex organizations, because progress in establishing a program of suicide prevention is often nonlinear, with different subgroups and teams working in different areas, either in tandem or in sequence. The domains and characteristics shown on
Figure 2 encompass and expand on key elements of the Zero Suicide framework, as articulated by Hogan and Grummet (
9), and as elaborated, adapted, and examined by others (
1,
2,
10–
14): leadership, training, screening and assessment, systematic suicide care protocol, evidence-based treatment, care transitions, and quality improvement.
Building Cultures of Safety and Prevention
The first core domain is the fostering of a culture of safety and prevention, a supportive organizational environment consonant with the life-affirming goals of suicide prevention. Creating such a culture involves engaging and communicating with leaders and other interested parties about suicide prevention and the organization’s progress toward this goal, ensuring that lived experience perspectives are integrated into leadership, and committing to a Restorative Just Culture that seeks healing and positive change after a suicide attempt or suicide.
All Interested Parties Engaged and Informed
Promoting change in complex organizations—especially in public sector organizations balancing multiple accountabilities, such as to government, politicians, media, and the public—requires strong leadership, effective communication (
15–
17), and fostering conversations that evolve from preparatory to action-oriented over time (
18). Continuous engagement from and between leaders and other interested parties is critical. From the beginning, formulations of the Zero Suicide approach emphasized the importance of executive leadership. Commitment, engagement, and embrace of change are needed from staff in all roles (
19) to embed an effective, enduring culture of safety and prevention. Consequently, ongoing communication across all levels of leadership is vital for maintaining focus on suicide prevention, keeping it top of mind throughout the system, and promoting broad buy-in. While senior leadership shares the message that suicide prevention is a priority and that change is happening, those leading the suicide prevention initiative can share accomplishments, explain how the program is evolving, and encourage interested parties to provide feedback. The goal of this communications strategy is to frame changes in practice in the context of the mission of the organization and the individuals within it, so suicide prevention becomes part of individuals’ professional identities and relationships (
18).
A strong internal communications plan might identify a particular practice innovation and convey its importance, the research behind it, and progress in its implementation. In Danny’s case, successful internal marketing of safety planning could have increased the likelihood that the clinicians treating him would have seen this step as indispensable, despite challenges, such as lack of time and staffing.
Lived Experience Integrated Into Leadership
Building and sustaining a culture committed to suicide prevention means putting humans at the center of the care system. People with lived experience of suicide are those who have attempted suicide or have struggled with suicidal thoughts, those who care for or support others who struggle with suicidal thoughts or behaviors, and friends or relatives of people who have died by suicide (
20). There is growing awareness that substantive engagement with people with lived experience is vital at all stages of planning and continuous quality improvement (CQI) activities to build a responsive and effective system (
21–
24). The field has now matured to a point at which frameworks and training (
25) are available to help those with lived experience to draw on that experience in contributing to advocacy, leadership, and education. Lived experience perspectives must be integrated into leadership to ensure they shape priorities and contribute to evaluation of the system’s elements. Advisors must be treated as full and fairly paid members of the team, not as third-party advocates lucky to be heard.
People with lived experience often report not feeling listened to in the ED and receiving no meaningful intervention or help in accessing behavioral health care in their community. Many would also likely emphasize that safety planning should be carried out in a caring and empathic manner, not merely as a box-checking exercise—reinforcing that the way safety planning is conducted is more important than simply filling in the boxes in an electronic health record template. Such insights from people with lived experience could have significantly improved Danny’s ED experience.
Review Process Based in a Restorative Just Culture
Restorative Just Culture (
26,
27) takes a forward-looking approach to adverse events that centers on identifying who has been harmed. The goal is to provide real justice and accountability to support learning and improvement rather than apportioning blame. After an incident, restorative practices ask who has been affected, what their needs are, and who is obligated to meet those needs, with the goal of repairing trust and relationships. Restorative Just Culture is not applicable only to suicide prevention, but suicide-related incidents provide one critical context for living out these principles. Turner et al. (
28) have argued that a critical incident review process rooted in such a culture should accompany efforts toward Zero Suicide. In a traditional root cause analysis (RCA), the goal is for dispassionate investigators to chart causal factors—typically a personal or institutional deficiency. A Restorative Just Culture review, by contrast, prioritizes engaging with bereaved families and staff who cared for the deceased in an accountable, but nonblaming, process organized around healing and addressing hurts, capturing all possible learnings, and enacting recommendations for the future. A recent evaluation (
29) has shown that such a process generates stronger engagement and recommendations from interested parties.
If Danny’s suicide attempt had led to his death, an RCA might have identified staff failure to deliver best-practice interventions as the proximal deficiency, leading to procedural and educational interventions to improve delivery. However, this approach neglects the broader human and systemic factors that contributed to the outcome. An analysis grounded in a Restorative Just Culture, by contrast, might have identified more distal systemic features contributing to the absence of a safety plan. For instance, even if all staff had been trained adequately, it might have been learned that planning was deprioritized by busy and highly pressured nurses who felt that other clinicians paid little attention to plans. Further review might have found that supervisors frequently perceived safety plans as less important than clearing patient backlogs. Unless Danny had died following his attempt, an RCA would have been unlikely to occur. A Restorative Just Culture approach, by contrast, may well have sought learning opportunities from Danny’s attempt, if information about it had come to light. Had such a learning system been in place prior to Danny’s visit to the ED, his outcome may have been changed through task shifting or by reprioritizing care components to create time for safety planning.
Applying Best Practices, Policies, and Pathways
The second core domain ensures that the culture of safety and prevention is expressed in practices, policies, and pathways that promote safety and focus on long-term recovery and health. These should be shaped by codesign processes that draw on lived experiences and are continuously measured, updated, and improved to ensure that problems are addressed and advances are integrated.
Practices and Pathways to Promote Safety, Recovery, and Health
Until recently, health care workers lacked evidence-based interventions, grounded in rigorous research, for suicide risk. Progress over the past two decades, however, has led to broad-based meta-analyses showing strong results for behavioral (
4,
30) and pharmacological treatments (
31), with other behavioral, medical, and technological interventions under investigation (
32). The effectiveness of system-level characteristics of suicide prevention pathways, policies, and practices has also undergone recent study, with promising results (
1,
12,
14). Thus, there is an urgent need to introduce these evolving best practices across systems and to connect them into treatment pathways.
Policies and practices should provide guidance to assist decision making, but without removing the ability to tailor choices to personal circumstances. Prescriptive requirements can limit person-centered care, leaving people feeling alienated and detached following a care experience. For example, primary care or school-based protocols may require an emergency evaluation any time suicidal ideation is reported. Although a specialist evaluation may be one of a set of options considered, such thoughts might be better handled with basic collaborative safety planning and close follow-up, with risks and benefits weighed in relation to the person’s situation, desires, resources, and needs, rather than by reducing intervention to a mechanical process.
The quality of the care Danny received in the ED prior to his evaluation mattered. Lengthy waits, dehumanizing safety precautions, boredom and discomfort, and feeling ignored or stigmatized by staff contributed to his feelings of burdensomeness, hopelessness, and isolation. Danny’s fear of hospitalization created a disincentive for frank disclosure. Because the clinician felt pressured by time constraints and overload, an adequate personal connection was not established. The clinician neither identified nor assessed Danny’s fear of hospitalization as a possible impediment to openness, and nor did the clinician explore intermediate-level treatment options, such as partial hospitalization or enhanced outpatient care. Protocols or pathways without sufficient attention to humane treatment and rapport building may provide only an illusion of adequate care, because individual evidence-based elements may not lead anywhere helpful without appropriate supporting measures.
Codesign with Diverse Service Users, Families, and Communities
Codesign or coproduction involves bringing together clinical professionals and those with lived experience of services as equal partners in the design and continuous improvement of health services to ensure that systems and processes are compatible with service users’ needs and wishes (
33–
37). Despite the challenges involved in flattening hierarchies between clinicians and people receiving care (
38,
39), there is increasing recognition that codesign is necessary if systems of care are to truly serve the humans at their center (
40,
41). Issues such as long wait times, not being listened to, and having one’s concerns minimized, were documented in the suicide prevention literature (
42) more than 15 years ago. Significant work has since focused on reducing wait times, improving workflows, and developing pathways to appropriate referrals, but problems persist (
43). Those who use health services, or who might have if these services had been organized differently, can help shape practices, policies, and pathways to fit the real needs of people at risk for suicide. Engaging service users and families or caregivers in codesign can bring new perspectives to policies, processes, and procedures. For instance, service users can provide first-person insight into what feels comfortable in developing a safety plan. Working with a codesign team of people with lived experience can lead clinicians to question assumptions about what is unavoidable and what is essential, and to think more creatively about how to deliver care.
Danny’s example highlights environmental and interpersonal stressors that codesign might mitigate. For those with suicidal thoughts, an ED can be a difficult environment, filled with stressors such as noise, other people in distress, and the threat of involuntary restraint. In response to these issues, lived experience advocates have worked with policy makers to develop specialized spaces—either within EDs or offsite—to provide care in environments that can help make the person with suicide risk feel calmer and more in control. The Crisis Respite Center model (
44) is a particularly promising alternative to standard ED care and is undergoing trials in several countries. Other community-led models are also gaining traction. If such alternatives had been accessible to Danny, additional opportunities for prevention may have become available.
Data-Driven Continuous Quality Improvement
The journey to reduce suicides requires a commitment to CQI (
1). CQI involves looking for patterns in care and data, not only around the worst outcomes, but also when protocols are enacted well and when protocols break down without a bad outcome. Although nobody needs persuading that quality monitoring is worthwhile, practical application is another matter. Ongoing processes for gathering feedback and measuring outcomes should be established, along with regularly scheduled reviews to reflect on the data gathered, identify ways to improve care, and develop plans for implementing change. A sustainable continuous improvement mindset requires that staff feel supported and heard by system leaders. A supportive work culture enables the flow of information that drives change and encourages honesty about what does and does not work in the system.
In our example, measurement of the number and quality of safety plans conducted in the department might have flagged the need for improved suicide prevention training and the prioritization of safety plans. Periodic review and communication of these data to leaders and staff might then have driven changes, leading to the opportunity for prevention being grasped for Danny. A Restorative Just Culture creates a space in which quality improvement measurement and activities can have maximal impact.
Workforce Education and Development
The provision of effective care and the strengthening of a culture of safety and prevention requires a common framework and language for talking about suicide and a sustainable approach to continuing education and onboarding of new staff that is built around lived experience.
Shared Framework and Language Across Teams, Services, and Systems
Organizational culture is supported by shared symbols, language, frameworks, and stories about what the organization stands for and hopes to become (
45,
46). One way to support a whole-of-organization approach toward suicide prevention is to unite people across roles and settings around a common language and framework. A visual map of practices and values (
47,
48) is an invaluable tool for bringing people together, literally “on the same page,” around suicide prevention. A visual framework can become a distinct “artifact” (
46) of the new culture, an accessible representation of the policies, practices, and pathways that the leadership wishes to promote. A common framework embeds shared values and informs workforce actions. Furthermore, unlike a densely worded policy document, a visual map of the framework can usefully be displayed on the wall for staff and those receiving care to see and consult, as nursing leaders did in one recent ED quality improvement project (
49). A common language ensures that people throughout the organization can communicate effectively and efficiently with one another, supporting warm transitions as the person seeking care and the care team decide on the right care pathway. A unified framework and language can also be shared transparently with those receiving care and their families and support persons, inviting them to navigate and partner with the system.
Although leaders had announced and developed documentation templates for the new safety planning protocol in the ED where Danny sought care, there was no common language or conceptual structure for how this practice should be embedded within and across systems. If the ED used the same planning process as outpatient behavioral health clinics, the safety plan could have been reviewed, reinforced, and adapted over time when the individual transitioned to lower levels of care, rather than being a “one off” intervention. In turn, ED staff could review and revise a safety plan for the patient, if one had been created for the patient in an outpatient setting.
Lived Experience Role in Providing Workforce Education
Just as lived experience voices at the leadership level are essential to ensuring systems meet the needs of the people they serve, so lived experience perspectives are also critical for training staff (
50–
52). Workforce education programs can be codesigned and co-delivered with individuals who have lived experience of suicide.
Training that integrated lived experience perspectives might have helped ED staff understand how to treat Danny in a way that resonated with his personal experience, reducing his feelings of being dehumanized and ignored. Safety precautions are important and necessary for some individuals, but they are often applied in a blanket manner, without allowances for individual differences or adjustment over time. Incorporating narrative-based elements from lived experience perspectives into training materials could provide staff members with the kind of insights and communicative templates they need to connect with each person as a unique individual and to build safety precautions tailored to that person. This practice could counteract the one-size-fits-all protocols common in highly medicalized systems.
Sustainable Ongoing Learning and Onboarding of New Staff Into Culture
Effective suicide prevention training needs to keep best practices, policies, and pathways top of mind for all staff. There is a broad consensus that a single “one-and-done” training course cannot deliver this outcome, but in a 24-hour-a-day operation, it is difficult to offer alternatives. It sometimes feels as if health care systems are forced to pick between engaging but hard-to-scale models, such as expert-led live group training, and online click-through modules that scale well but leave learners feeling unengaged. Recent work (
47,
53) suggests a hybrid middle ground may provide a viable alternative, combining live access to experts with online modules completed together by groups. A commitment to best practices and CQI requires new developments in suicide prevention to be integrated into staff skill sets. Consequently, workforce education initiatives should provide ongoing refreshers to keep staff engaged, as well as frequent updates to ensure that everyone has access to the latest knowledge. Onboarding new staff presents further challenges. New team members require flexible and effective initial training programs that introduce best practices, align them with the system’s values and culture, and connect them into workplace networks. Because financial and time constraints are the norm, training programs need to deliver these goals in busy contexts without incurring unsustainable costs.
The nurse who discharged Danny was newly hired and had received only cursory training on safety planning, delivered through self-paced, click-through online modules, with no periodic refresher or skills reinforcement from a supervisor. Training incorporating skills-based learning, longitudinal supervision, and performance auditing would have helped embed the importance of safety planning. Real systemic change, however, requires a fundamentally social approach that is contextualized in the workplace setting, links staff into networks, and contributes to peer group norms. With all these elements in place, there is a good chance that Danny would have been discharged not only with a safety plan, but with a
high-quality,
person-specific plan that conformed to the manner in which crisis and safety planning has been tested (
54,
55).
Conclusions
A systems approach to suicide prevention, examining both outer and inner contexts, seeks to create a coherent, competent system of care built around best practices and lived experience perspectives. By putting the individual human at the center of the system, the aim is to improve care for the whole population of people at risk. We cannot know whether a systems approach would have changed the outcome in Danny’s case; despite whatever systemic changes are enacted, personal and social factors will continue to contribute to suicide attempts and ideation. Nevertheless, although a systems approach will not change outcomes for every individual, changing the way that everyone within a system is treated can help maximize opportunities for altering outcomes in any particular situation.
This article focuses on a health system example, but many of the principles can be applied more widely, in contexts such as military settings, community services, workplaces, or schools. It has been established that shifts in the outer context, beyond health care systems, are necessary for reducing suicide rates more broadly. However, neither the inner nor the outer context can stand alone. Prevention efforts within and beyond health care systems must take place in tandem, and ideally in a mutually supportive way, so that those at risk and their loved ones are met with coherent, coordinated, and evidence-based care, in health care contexts and beyond.
Acknowledgments
The authors thank Paul Scade for his assistance in preparing this manuscript.