Physical assaults (i.e., nonaccidental physical contact that intimidates or harms another person) are a persistent problem in hospital psychiatry, disrupting the milieu and causing physical injuries, psychological distress, missed workdays, and increased costs.
1–9 Estimates of the proportion of patients who commit physical assaults range from 5 to 15 percent of the inpatient population.
10,11 Risk factors that may be associated with increased risk of assaultive behavior include younger age, male gender, involuntary admission, history of substance use, history of violence, and certain diagnoses (e.g., schizophrenia).
4,10,12 A diverse array of antecedents can precipitate assaultive behaviors, with research suggesting staff–patient interactions (e.g., imposing restrictions on a patient’s behavior or disputes over medication) precede nearly 40 percent of assaults.
6 Assaults may not have a clear underlying narrative.
6 Importantly, the majority of prior studies examined assaults on inpatient psychiatry units,
1–4,6,10,11,13–23 with a smaller literature addressing medical emergency rooms
18,24,25 and community settings.
3,26–28 Data describing assaults in the psychiatric emergency room are scarce, raising questions about the degree to which lessons learned from inpatient settings are applicable in the psychiatric emergency room.
Differences exist between inpatient units and psychiatric emergency rooms. The psychiatric emergency room is often a small space, where patients are in close proximity, patients are admitted and discharged 24 hours per day, intoxication and withdrawal symptoms may be especially acute, therapeutic programing may be limited, and patients are typically uncertain about their likely disposition. None of these factors is unique to the psychiatric emergency room, but the combination and relative intensities of these factors can make the psychiatric emergency room a unique clinical space. Moreover, psychiatric emergency rooms can vary in their size, location, staffing, and primary population served, raising additional questions about the generalizability of inpatient data to psychiatric emergency room settings.
Of the few studies examining assaults in the psychiatric emergency room, even fewer have described events in detail and assessed risk factors. Dawson
et al.29 compared violent and nonviolent patients on 72-hour psychiatric holds in a medical emergency room, but the sample size was small (
n=22 violent patients), the definition of violence included verbal altercations, and the analysis did not include multivariate models or adjustments for multiple comparisons. Lynch and Noel
30 tested a Risk of Violence Assessment scale in a psychiatric emergency room, attempting to predict future violence in both the psychiatric emergency room and inpatient unit, but their sample was also small (
n=32 violent patients) and was limited to a Veterans Affairs hospital with a 95 percent male population. McNiel
et al.31 used violence in the two weeks prior to presentation, as well as violence in the psychiatric emergency room, as a predictor of hospitalization rather than an outcome variable, and included fear-inducing behavior (e.g., verbal attacks, threats, attacks on objects) in the definition of violence. Similarly, Way
et al.32 studied assaultive behavior in the psychiatric emergency room as a predictor of psychiatric hospitalization rather than an outcome. Terrell
et al.,
33 examining a related question, reported the frequency of seclusion and restraint in a psychiatric emergency room, but statistical tests were limited to a t test for age.
33Methods
Setting
Data were collected at one adult psychiatric emergency room and two adult inpatient psychiatric units at a large, integrated, multi-campus, urban hospital system. The psychiatric emergency room is a locked, 24-bed unit, which operates 24 hours per day and is adjacent to a medical emergency room. The clinical team consists of psychiatrists, nurses, nurse practitioners, social workers, and occupational therapists who evaluate more than 500 patients per month. Regulations allow patients to be kept up to 24 hours for an evaluation or up to 72 hours in an extended observation room. The two inpatient units have 24 and 30 beds. Both have an average length of stay of approximately two weeks, and both are embedded in general medical hospitals. One unit has additional staffing for electroconvulsive therapy, and the other has additional staffing for substance use disorders.
Incidents
Whereas the underlying data source material called each event an assault, this article refers to events as incidents or incident reports to avoid overstating what is known about the events. In particular, the assault label implies culpability and can overlook significant ambiguities about what constitutes intentional versus accidental physical contact, who is perceived as the aggressor and who is engaging in self-defense, and whether the underlying motives are discernable.
Incident reports collected by the department of psychiatry were the primary source for identifying incidents in the psychiatric emergency room. This method is similar to previous studies on inpatient psychiatric units.
1,2,18,21,22,34 Hospital staff are trained to complete incident reports for all assaults via an online form, regardless of severity. Any staff member can enter an incident report, and reports can be entered anonymously. Reports include a brief description of what happened, when and where it happened, and who was involved. Incident reports were included in this study if the incident occurred in the psychiatric emergency room between January 2014 and December 2018 and had the classifications General Event Type: Safety/Security, and Specific Event Type: Assault.
The electronic medical record was reviewed for each patient identified in these incident reports to obtain additional narrative descriptions for each incident. Data collected from these narratives were event time (i.e., weekday, hour), location, who was involved in the incident, means of assault (e.g., punch), and interventions following the incident. Incident severity was assessed using the physical aggression subscale on the Modified Overt Aggression Scale (MOAS).
35 Initially, two authors (R.E.L. and S.A.R.) assigned MOAS scores to each incident, but after comparing MOAS scores for the first 31 incidents, there was near-perfect agreement (Cohen’s kappa 0.8524, standard error 0.101, 95% CI 0.6548–1), so one author (R.E.L.) assigned MOAS scores for all remaining incidents. This method was also utilized for incident reports originating from the two inpatient psychiatric units during the same time period.
Incident narratives, derived from incident reports and patients’ electronic medical records, were analyzed qualitatively to identify antecedent events and themes that precipitated the incident. A grounded theory approach was used, where themes were allowed to emerge from each narrative. Two authors (R.E.L. and S.A.R.), both psychiatrists with experience in qualitative research, first reviewed the incident narratives. R.E.L. generated a preliminary codebook, which was reviewed by S.A.R., who provided critical review and offered suggestions for clarity and parsimony. R.E.L. and S.A.R. coded each narrative independently and discussed the results. Discrepancies were discussed until consensus was reached. Revisions to the codebook were allowed throughout the coding process, which resulted in some minor modifications, clarifications, and consolidations, but no major changes were made; 90 percent of themes were present in the first 20 narratives, and 100 percent were present in the first 96 narratives, suggesting that theme saturation was achieved. In organizing the resulting list of antecedent events and themes, we generally tried to preserve the focus and specificity of the themes used in the codebook rather than aggregating themes into broad categories, so that the categories would not become vague, overly abstract, or too common to be useful to clinical staff.
Demographic and Clinical Factors
Demographic and clinical characteristics were collected from the electronic medical record for all patients who were mentioned in an incident report. If a patient’s first incident report originated from the psychiatric emergency room, the patient was described as a “psychiatric emergency room patient with an incident report.” If the first incident report originated on an inpatient unit, the patient was described as an “inpatient with an incident report.” Individuals were included only once even if they were involved in more than one incident; five psychiatric emergency room patients had two or more incident reports while in the psychiatric emergency room, two psychiatric emergency room patients had one incident report in the psychiatric emergency room and one incident report on the inpatient unit, and 20 inpatients had two or more incident reports on the inpatient units.
Demographic and clinical characteristics were selected based on previous literature studying agitation, aggression, and assault. Demographic characteristics were gender,
1,15,16 age,
1,2,15,16 homelessness,
14 unemployment,
10,14 and legal history.
2,15 Historical clinical characteristics were number of prior hospitalizations, prior hospitalization in a state facility, and history of violence.
1,2,15,16 Current clinical characteristics were enrollment in assertive community treatment, assisted outpatient treatment,
36 and presenting with thoughts to harm self or others.
1,2,15 Recent substance use was defined as any self-reported use within two weeks of presentation or positive urine toxicology.
1,14–16 Diagnostic categories were schizophrenia, schizoaffective, or bipolar disorder
2,14–16; unipolar depression (sometimes associated with decreased assault risk)
2,14,16; posttraumatic stress disorder; dementia
16; intellectual disability (associated with violence in a forensic setting)
37; traumatic brain injury
15,16; borderline personality disorder or traits
2,10,14; antisocial personality disorder or traits
2,10,14,15; and unspecified personality disorder or traits.
2,10,14Although some previous studies treated substance use as a binary category,
1,3,4,10,11,15,16 we examined substances individually. Schizophrenia, schizoaffective disorder, and bipolar disorder were combined because their presentations in a psychiatric emergency room can be indistinguishable. Patients with these diagnoses were separated into those with manic symptoms and those without manic symptoms because McNiel
et al.13 reported significant bivariate association between diagnosis (i.e., schizophrenia, mania, other) and “physical attacks” in the two weeks prior to involuntary civil commitment (with higher rates for schizophrenia and mania) and in the first 72 hours of commitment (with higher rates for mania).
The control group consisted of individuals seen in the psychiatric emergency room who did not appear in any incident reports. The control group was described as psychiatric emergency room patients with no incident reports. The control group was created by reviewing an administrative list of all patients seen in the psychiatric emergency room, organized by time of arrival. The individual arriving immediately before and immediately after the psychiatric emergency room patient with an incident report was chosen for the control group; if the selected individual was already in the data set, the next person on the list was selected. The reason for matching by time of arrival was to help control for milieu factors (e.g., staffing, waiting time, noise level, census). When reviewing the electronic medical record for each person in the control group, three electronic medical records contained reports of assaultive behavior while in the psychiatric emergency room, but there was no corresponding official incident report. These three individuals were added to the group of psychiatric emergency room patients with incident reports, and additional individuals were selected as controls using the criteria described above.
Data Analysis
Quantitative data were analyzed using Excel 2013 and Stata 15.1 (StataCorp LLC, College Station, Texas). The first analysis used incidents as the unit of analysis, with simple counts and chi-square tests to compare incidents in the psychiatric emergency room with incidents on inpatient psychiatric units. The second analysis was an assessment of demographic and clinical characteristics, which necessitated using individual patient records as the unit of analysis; we acknowledge that in most cases assaultive behavior is better conceptualized as a temporary feature of the illness rather than a permanent feature of the individual. This analysis was a three-way comparison of psychiatric emergency room patients with incident reports versus inpatients with incident reports versus psychiatric emergency room patients with no incident reports. This analysis used chi-square tests for categorical variables and analysis of variance for continuous variables. Post hoc analysis without adjustment was used to detect between-group differences and included t tests for continuous variables and chi-square tests for categorical variables. Variables with statistically significant associations were entered into a conditional logistic regression model comparing demographic and clinical characteristics of psychiatric emergency room patients with incident reports versus psychiatric emergency room patients with no incident reports, which accounted for case–control matching by time of arrival. Statistical significance was defined as P < .05.
This study was approved by the Institutional Review Board at the New York State Psychiatric Institute. Additional details of the methodology can be found in the supplemental materials available in the online version of the article (under Figures & Data).
Discussion
In this qualitative and quantitative analysis of assault incident reports from the psychiatric emergency room and inpatient psychiatry units, there were similarities across sites in the types of incidents that occurred, as well as in their severity. Our results echo previous literature on risk factors for inpatient assault, including younger age, history of violence, and presenting with thoughts of harming others.
1,2,15,16 Previous studies have also reported reduced risk of assaultive behavior among depressed patients
2,14,16 and have pointed toward some relationship between psychotic disorders and assault risk.
3,4,17 These similarities suggest much of the literature generated on inpatient psychiatry units is applicable to a psychiatric emergency room setting.
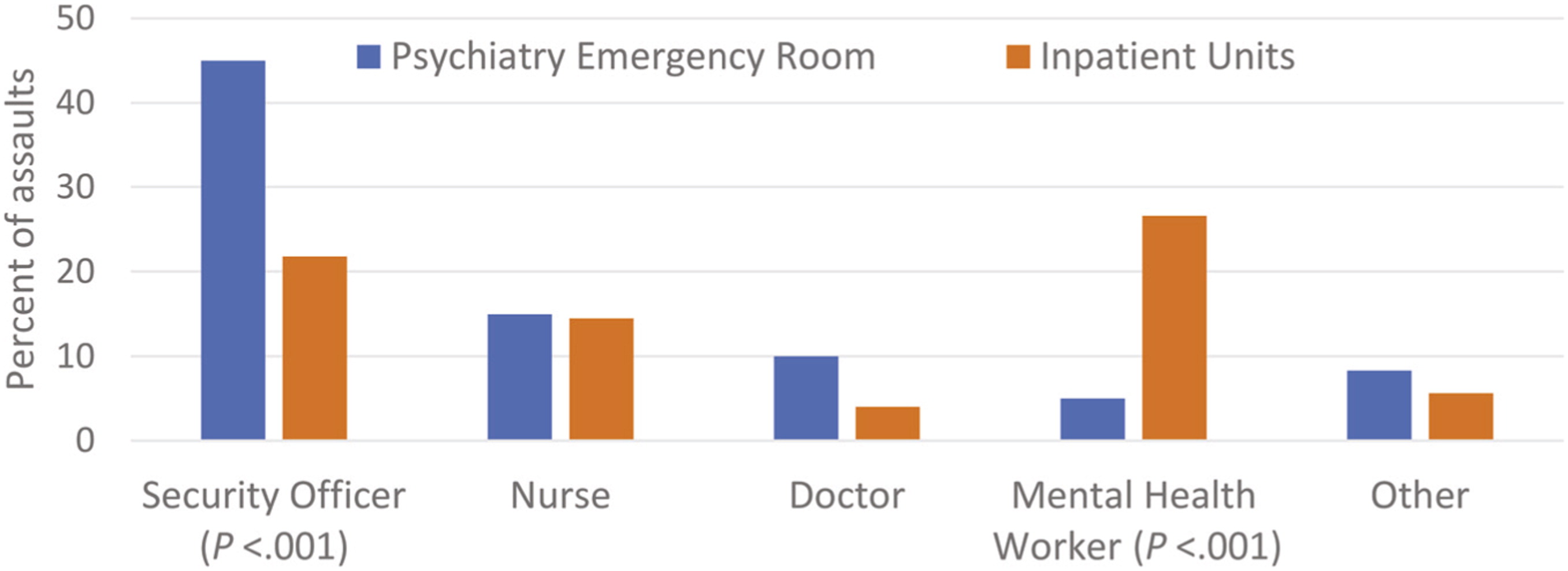
Our results also suggest some differences between the two settings regarding which staff members are at highest risk, the use of manual holds, associations with time of day, and the possible role of antisocial personality disorder. Awareness of these differences could inform staff training and preparation, especially for mental health workers and security officers.
Although identifying risk factors associated with assaultive behavior is valuable, it is also true that assaultive behavior is notoriously difficult to predict. If patients are confused, intoxicated, impulsive, intellectually disabled, or motivated by an internal logic known only to the patient, staff might have difficulty knowing what the patient is thinking, feeling, or trying to do, and so might have difficulty anticipating and preempting assaultive behaviors. This challenge could partially explain why these situations result in assaults rather than successful de-escalations. Other studies have noted that in-hospital assaults can be difficult to predict. Grassi
et al.
10 reported that the cause of violence was not immediately apparent in 44.4 percent of 116 cases. Hillbrand
et al.2 reviewed charts for three days before each of 104 incidents of assault by forensic inpatients and found no prodromal signs in 20 incidents. Papadopoulos
et al.,
6 reported in their meta-analysis that there was no clear cause for 33 percent of incidents; they are correct to highlight the important role that staff play in identifying cues and intervening to prevent violence from occurring. Tam
et al. are likely also correct to warn that “[t]he myth that all violence can be spotted early and dealt with should be dispelled” (Ref. 13, p 87).
Previous studies have reported heightened rates of in-hospital violence among patients with manic symptoms.
13 This may represent selection bias, in that patients with this condition who are exhibiting dangerous behavior might be especially likely to receive treatment in a psychiatric emergency room or inpatient unit. It is also possible that patients who exhibit aggressive behavior might be especially likely to receive a diagnosis of mania. These results are also consistent with the possibility, even when clinical staff identify risk factors and implement appropriate interventions for each patient, that these interventions might produce less immediate effect for patients with manic symptoms.
Although most individuals with schizophrenia are not violent, debate does exist over whether schizophrenia is associated with increased risk of violence in the hospital. Many previous studies have reported this association,
3,4,17 but some recent studies have noted no such association.
2,21,22,30 Importantly, many of these studies used “schizophrenia” as a collective term that included multiple diagnoses, and the publications did not always specify what was included. For instance, Dack
et al. grouped patients into three categories: “schizophrenic (including schizoaffective, etc.), affective (depression, mania, etc.) and other (personality disorder, organic brain syndrome, etc.)” (Ref. 4, p 263). Lehman
et al.
3 used “schizophrenia and other psychoses,” Biancosino
et al.17 reported on “schizophrenia and related disorders,” and Sanghani
et al.21 separated assaultive patients into a “schizophrenia spectrum” and a “nonschizophrenia spectrum.” Differing definitions likely contribute to heterogeneous results; erroneously identifying schizophrenia as increasing assault risk could increase stigma, promote overly restrictive treatment plans, or divert clinical resources from patients who are actually at increased risk. The finding that patients with schizophrenia, schizoaffective disorder, or bipolar disorder were at heightened risk for assaultive behavior only when manic symptoms were also present, if replicated, might advance discussion by identifying clinical circumstances when these patients might be at increased risk and by emphasizing a treatable symptom.
Multiple studies have reported inpatient nursing staff to be at increased risk of being assaulted, especially nursing assistants, mental health workers, and technicians.
20,38 Few studies have addressed risk to security personnel. One analysis of Veterans Health Administration facilities reported slightly higher annual injury rates among security personnel (73.7 injuries per 1,000 employees) than among nursing assistants (71.8 injuries per 1,000 employees).
3 A different study at a forensic hospital reported much higher annual injury rates among psychiatric technicians (25.5 per 100 staff) than among facility police officers (5.6 per 100 staff).
2 In our study, the fact that security officers were at higher risk in the psychiatric emergency room and mental health workers were at higher risk on inpatient units probably reflects different staffing models. The psychiatric emergency room always has four security officers present and a few mental health workers (i.e., this number varies according to how many patients require 1:1 observation), whereas the inpatient units have multiple mental health workers and typically 0–1 security officers. The person at greatest risk of being assaulted might be whoever is closest to the high-risk patient. This possibility would be consistent with data from the MacArthur Violence Risk Assessment Study, in which discharged patients were followed in the community. Those results indicated that the most common victim of community violence was a close affiliate, such as a spouse, girlfriend, boyfriend, or other friend.
27Several clinical variables were significantly associated with assault risk in bivariate models but not in the logistic regression model. One interpretation is that each bivariate association represents a clinically useful marker of risk, but the variables are too closely related to make independent contributions to the final model due to collinearity (e.g., homelessness, history of violence, substance use, and prior arrest might be measuring similar underlying social factors).
The association between assault risk and recent cannabinoid use invites further study. Associations between marijuana use and violence have been reported occasionally, including among individuals with first-episode psychosis
39 and persons who use marijuana after a psychiatric hospitalization,
40 but research on this potential relationship is limited.
This study has limitations. Underreporting of incidents is a recognized problem.
25 Incident reports and medical records are not comprehensive accounts of events. It is not known if any of these individuals was assaultive outside these three clinical areas, outside the hospital, or outside of this five-year window. While two different inpatient units supplied data, psychiatric emergency room data were limited to one location. Some analyses were limited by low cell counts. Additional factors describing the milieu and staffing factors are likely relevant to specific events but were not obtainable. These findings may not be generalizable to other settings where patients are treated in general emergency rooms without a dedicated space or an interdisciplinary team serving patients with psychiatric emergencies. These findings also do not distinguish between individuals who have one incident versus many incidents.
Another limitation involves the process by which patients in this study were assigned diagnoses. Whereas many diagnoses are defined by time durations lasting weeks or months, patients in the psychiatric emergency room may receive a diagnosis after the psychiatric team has observed the patient only briefly. Many patients had prior visits as well as inpatient and outpatient notes that informed the diagnosis, but other diagnoses were based on one-time assessments. Future studies would benefit greatly if more specific diagnoses could be incorporated, especially if larger sample sizes allowed diagnostic subgroups to be parsed and assessed. For example, a future study with a large sample size could separately assess schizophrenia with agitation, schizoaffective manic episode, and bipolar mania with psychotic features to measure the safety risks associated with each of these symptom states.
The definition of assault used in this study limits direct comparison to other studies that use alternative definitions or primary outcomes. As mentioned in the introduction, other studies of emergency room settings have included verbal altercations
29 and fear-inducing behavior
31 in their definitions of violence, which likely expands the sample available for analysis but reduces the specificity of the outcome. Unfortunately, the emergency room literature does not include a study comparable with the present analysis, using physical assault as the outcome variable, which is both a limitation of the field and an opportunity for future research. This limitation has been mitigated by assigning MOAS scores to each incident, which helps standardize descriptions of what occurred.
In conclusion, in this study of assault incident reports, incidents in the psychiatric emergency room and on the inpatient units had similar precipitants, means, and clinical interventions, which suggests that much of the broader literature from inpatient psychiatry can be generalized to a psychiatric emergency room setting. Disorganization, manic symptoms, and intellectual disability were potential risk factors that might inform clinicians’ efforts to intervene and use de-escalation techniques before violence occurs. Manic symptoms in particular were strongly associated with assault risk, which presents a treatment opportunity that might decrease risk. Although perfect prediction of assaultive behavior is unlikely to be achieved, there is reason to hope that ongoing education about risk factors and de-escalation techniques can help psychiatric emergency rooms and inpatient units deliver high-quality patient care in an environment that is safe for patients and staff.