To the Editor: Chromosome 22q11 and the gene/genes in this region that may be responsible for susceptibility to schizophrenia have been previously studied.
1 We present a novel finding in schizophrenia that is a maternally-inherited uniparental disomy (UPD) on chromosome 22 cent-q11.2 in a female patient with disorganized behavior and psychotic symptoms.
Case Report
An 8-year-old girl was referred because of mental retardation and behavioral problems. Written, informed consent was obtained from the parents for the publication of the patient's details.
She was born to consanguineous parents at 31–32 weeks' gestation. Her birth percentiles were in normal ranges. Her developmental milestones were slightly delayed. There was no history of psychiatric disorder in the relatives except that there were two members with idiopathic mental retardation. Her physical assessment at age 8 revealed elfin-like facial features, sparse medial eyebrows, arched eyebrows, hypertelorism, depressed nasal bridge, bulbous nasal tip, downturned corners of mouth, thick lower lip, and joint laxity. Imaging studies were normal.
Psychiatric evaluation at age 3 revealed language-development delay, restricted social relationships, echolalia, and lack of interest in peer-relationships and toys. Her psychometric evaluation with developmental tests showed a 1-year delay.
2 Echolalia, social-relationship restrictions, and not having imaginary play were noted as autistic-like features. At age 6, unrealistic fears, psychomotor agitation, disorganized behavior, auditory and visual hallucinations, incoherence, irrelevant and disorganized speech, and delusions were observed. She was diagnosed as “very-early-onset schizophrenia” according to the DSM-IV criteria.
3 Her Scale for the Assessment of Positive Symptoms (SAPS) and Scale for the Assessment of Negative Symptoms (SANS) scores were 75 and 72, respectively. Her psychiatric disorder severity score was 6, according to Clinic Global Impression Scale–Severity (CGIS–S).
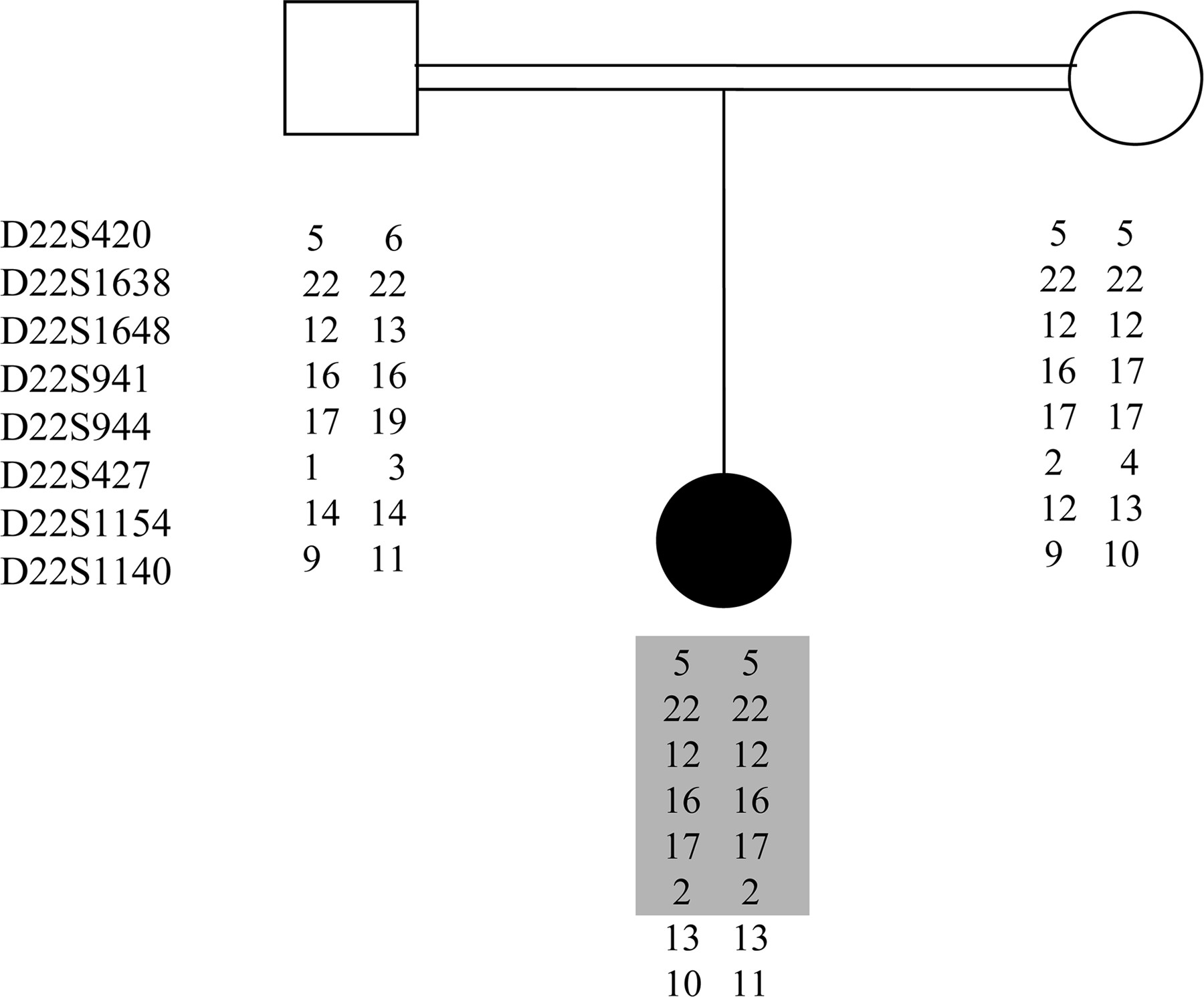
Her karyotype and FISH analysis were normal. Whole-genome analysis by Affymetrix Human SNP Assay 6.0 kit revealed inherited copy-number variations (CNVs) and loss-of-heterozygosity (LOH) on a number of regions, which could be due to the parental consanguinity. LOH on chromosome 22 cent-q11.2 spanned 6 Mb. CNV analysis showed no evidence of any deletion in this region. The same analysis for the parents was normal. Microsatellite marker analysis with 8 markers confirmed maternally-inherited UPD (
Figure 1). Catechol-
O-methyltransferase (COMT) gene at 22q11, which has been identified as a susceptibility locus for schizophrenia, revealed 100-fold down-regulation, as compared with a control group. Therefore, it could be speculated that COMT could be one of a number of other genes down-regulated in this UPD region that may have contributed to the clinical presentation.
In conclusion, this is the first report reinforcing the link between 22q11 and schizophrenia with two novel findings; first, down-regulation of COMT expression, which may be due to the maternally-inherited UPD; and second, phenotypic effects of the same abnormality.