Prevention of Post-Stroke Generalized Anxiety Disorder, Using Escitalopram or Problem-Solving Therapy
Abstract
Methods
Patients
Neurological and Neuroradiological Evaluations
Experimental Design and Treatment
Assessment Instruments and GAD Diagnosis
Adverse Events
Statistical Analysis
Results
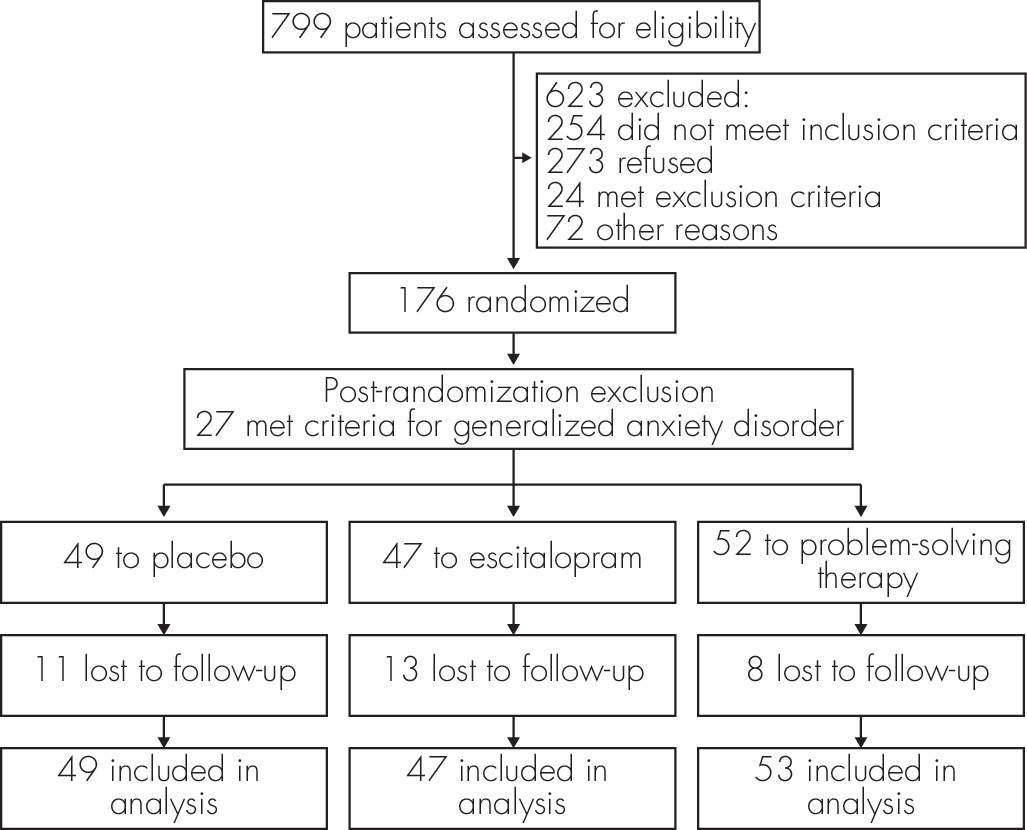
Participants and Baseline Measures
| Placebo (N=49) | Escitalopram (N=47) | PST (N=53) | |
|---|---|---|---|
| Age, mean (SD), yearsa | 64.8 (13.5) | 61.5 (13.7) | 68.3 (10.4) |
| Male, % | 67.3 | 63.8 | 54.7 |
| Married, % | 59.2 | 53.2 | 47.2 |
| Education, mean (SD), years | 13.4 (2.9) | 13.4 (3.1) | 14.1 (2.9) |
| Socioeconomic Class IV, Vb, % | 26.5 | 19.1 | 24.5 |
| Previous history of GAD, % | 6.1 | 6.4 | 5.7 |
| Baseline Hamilton Rating Scale for Anxiety score, mean (SD) | 6.8 (4.4) | 7.1 (5.6) | 8.3 (5.4) |
| Baseline Functional Independence Measure (FIM) score, mean (SD) | 114.9 (20.7) | 115.8 (16.6) | 114.5 (13.7) |
| Baseline Social Functioning Exam score, mean (SD) | 0.13 (0.12) | 0.12 (0.09) | 0.09 (0.09) |
| Stroke characteristics, % | |||
| Hemorrhagic stroke | 8.2 | 4.3 | 13.2 |
| Ischemic stroke | 91.8 | 95.7 | 86.8 |
| Large-artery atherosclerosis | 30.6 | 36.2 | 20.8 |
| Small-artery occlusion | 32.7 | 17.0 | 30.2 |
| Cardioembolism/Other | 28.6 | 42.6 | 35.8 |
| Left-side lesion | 51.0 | 48.9 | 41.5 |
| Medical comorbidity | |||
| Systolic blood pressure, mean (SD), mm Hg | 144.0 (24.4) | 139.3 (24.1) | 146.9 (20.6) |
| Low-density lipoprotein cholesterol, mean (SD), mg/dl | 122.5 (47.7) | 116.3 (37.0) | 109.9 (38.0) |
| Cumulative Illness Rating Scale total score, mean (SD) | 9.7 (4.6) | 10.2 (5.4) | 9.5 (4.8) |
| Diabetes mellitusc, % | 20.4 | 42.6 | 17.0 |
| Coronary artery disease, % | 22.4 | 25.5 | 24.5 |
| Cognitive heart failure, % | 6.1 | 14.9 | 13.2 |
| Atrial fibrillation, % | 14.3 | 14.9 | 22.6 |
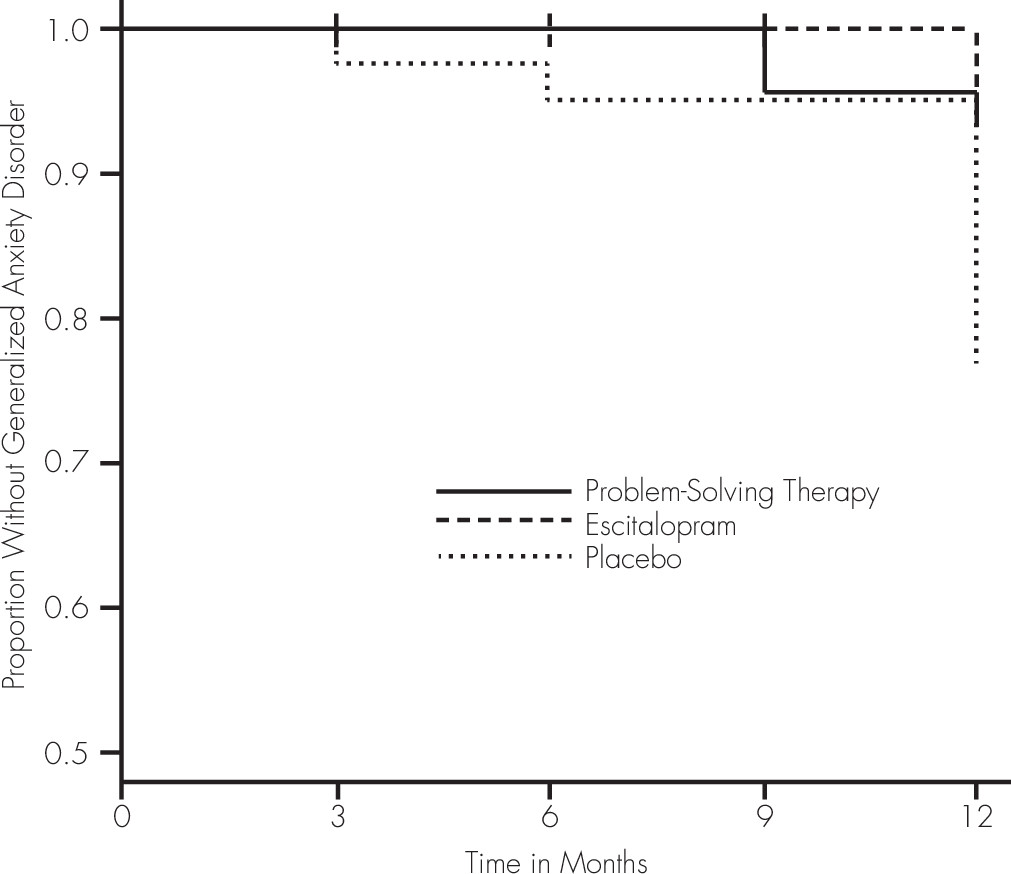
Effect of Preventive Intervention on GAD
| Adjusted Hazard Ratio (HR) | 95% Confidence Interval (CI) for Hazard Ratio (HR) | p | |
|---|---|---|---|
| Placebo versus escitalopram | 4.95 | 1.54–15.93 | 0.0073 |
| Placebo versus PST | 4.00 | 1.84–8.70 | 0.0005 |
| Escitalopram versus PST | 0.81 | 0.12–5.26 | NS |
| Age | 1.03 | 1.01–1.06 | 0.0097 |
| Previous history of GAD | 3.59 | 7.74–4.64 | 0.0005 |
| Female vs. male | 1.39 | 0.59–3.07 | NS |
| Baseline Functional Independence Measure score | 1.03 | 0.96–1.10 | NS |
Adverse Events and Adverse Effects
Discussion
Acknowledgments
Footnote
References
Information & Authors
Information
Published In
History
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).