Although over 400 cases have been identified by Dalmau and his colleagues, there are few studies reported in the psychiatric literature on neuroimmune and behavioral management, especially in adolescents. In order to demonstrate the complexity of this disease and its clinical management, we have included the following description of an case in an adolescent.
Case Presentation
A previously-healthy 14-year-old African American girl reported a weeping blister below her nose, a sunburn-like facial rash, headache, and a temperature of 37.8°C (100°F). These findings quickly resolved without intervention. Two days later, she developed acute-onset auditory hallucinations and paranoia. She told her parents, “God said everything will be OK.” She was brought to the emergency department after becoming physically threatening. The patient’s past psychiatric and medical history were unremarkable.
After spending 2 days in an inpatient psychiatric unit, she was transferred to the pediatric intensive-care unit for further work-up. She demonstrated hyperactivity, irritability, increased speech, insomnia, and continued paranoia. Her CSF revealed a lymphocytic pleocytosis of 49 nucleated cells per mm3 with 98% lymphocytes and normal glucose and protein concentrations. The patient was started empirically on vancomycin, ceftriaxone, and acyclovir. The antibiotics were discontinued when her blood and CSF cultures returned negative. She was continued on acyclovir for 21 days to cover for presumed viral encephalitis of unknown etiology.
Her head CT, basic metabolic panel, and urine toxicology screen were unremarkable. She experienced one witnessed tonic–clonic seizure, after which she was placed on prophylactic levetiracetam. Her electroencephalogram (EEG) revealed frontal slowing, but no epileptiform activity.
A week later, the patient’s cognitive and neurological status deteriorated significantly. She became incontinent of bowel and bladder, and refused to take anything by mouth, necessitating nutritional support by nasogastric tube. Her mental status waxed and waned; at times she produced speech, with word-finding difficulty, and at others, she remained mute. For periodic agitation, lorazepam 1 mg iv prn provided some relief.
Given a broad differential, including endocrine, infectious, inflammatory, and autoimmune etiologies, an extensive medical work-up ensued, but was unrevealing. Her creatinine kinase was elevated, at 1,116 IU/L. Standard autoimmune antibodies were not detected in her CSF or serum. Her CSF was also negative for voltage-gated potassium-channel antibodies. A series of other tests for viral and parasitic etiologies were negative. She was started on a course of prednisolone 30 mg by nasogastric tube every 12 hours for presumed autoimmune encephalitis.
Six weeks after the initial onset of symptoms, her CSF was found to be positive for anti-NMDAR antibodies (Laboratory of Neuro-Oncology, University of Pennsylvania). Full-body MRI and PET scan were negative for malignancy. A 3-day course of intravenous immunoglobulin (IVIG) was administered, without significant improvement.
Two months after her initial symptoms, her CSF showed no WBCs, but remained positive for anti-NMDAR antibody. Serum ESR and CRP were found to be elevated, at 114 mm/sec and 39 mg/L respectively.
The patient’s mental status varied in terms of alertness. She demonstrated periods of dystonia, dyskinesia, spastic rigidity, cogwheel rigidity, bilateral upper-extremity hyperreflexia, as well as periods of decreased tone in all extremities. She made infrequent, unintelligable verbal communication with family members, but was able to recognize herself and her family in photographs. The patient remained incontinent of bowel and bladder function and required nutrition by nasogastric tube.
A psychiatric evaluation was obtained for recommendations on continued aggressive behavior and impulsivity. The patient showed limited improvement in aggression after a 1-week trial of oral risperidone 1 mg ng q8hr prn, and some improvement in agitation and insomnia with diphenhydramine 25 mg iv q6hr prn. Around this time, the neurology team recommended carbidopa-levodopa 10 mg/100 mg bid for muscle rigidity.
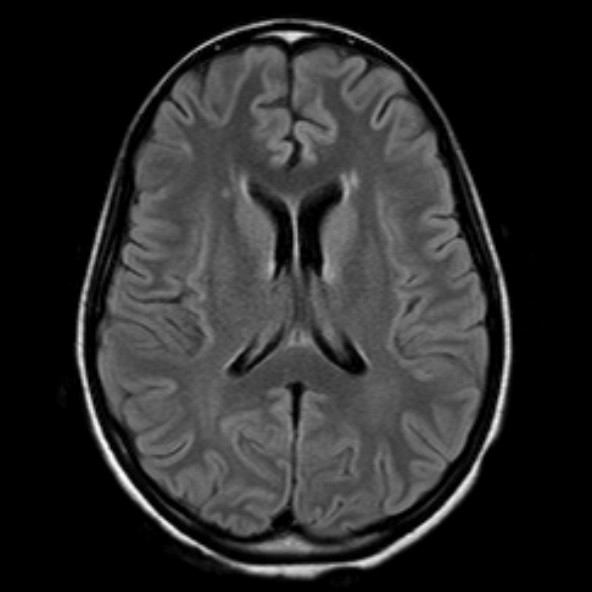
Seven weeks after symptom onset, a second brain MRI revealed minimal nonspecific periventricular white-matter changes (
Figure 1). A repeat EEG showed a background with moderately organized waves of 10 per second. The patient began to develop symptoms consistent with worsening catatonia: waxy flexibility, echolalia, muscle rigidity, negativism, stereotypy (lip and tongue biting; fidgeting with clothes), blank staring, and a grasp reflex. She received scheduled doses of lorazepam 2 mg iv every 6 hours, with temporary but dramatic improvement.
The following week, rituximab treatment was attempted, but the full course could not be completed because she developed autonomic instability and worsening catatonia within 24 hours. Emergent electroconvulsant therapy (ECT) was initiated on alternating days, normalizing blood pressure, pulse, and temperature, and improving her cognitive functioning. After seven ECT sessions, she became more aware of her surroundings, could name her location, play a simple card game, eat and toilet with assistance, and ambulate independently. Despite these advances, she remained impulsive and aggressive, and showed sleep-cycle inversion. She was started on valproic acid and trazadone to help stabilize her mood and improve nighttime sleep, while her lorazepam was tapered. The patient showed some improvement in aggression and sleep on this regimen.
To treat her autoimmune disorder, plasma exchange was performed in five sessions, without significant improvement in her cognitive functioning. One month later, rituximab was administered, followed by cyclophosphamide. She was eventually switched over to risperidone 2 mg bid and lorazepam 0.25 mg po bid to help with aggression and anxiety. The patient showed gradual improvement in cognitive functioning after her discharge to an inpatient rehabilitation program. Eight months after her initial symptoms, she began to engage in conversation with her parents, started running track, and could read and write at a fifth-grade level.