To the Editor: Although basal ganglia (BG) physiology is classically joined to motor function, increasing evidence has outlined its involvement also in cognitive and behavioral domains.
1 Personality changes as well as clearly psychiatric traits can be recognized in BG syndromes like Parkinson’s disease, and BG alterations have been described in psychiatric disorders. In schizophrenia, changes in subcortical brain regions have been extensively observed.
2 Herein, we describe a patient with schizophrenia who experienced a sustained remission after an occasional “selective” bilateral pallidal lesion induced by carbon monoxide (CO) intoxication.
“Mrs. R” was a 50-year-old woman affected by a paranoid form of schizophrenia, with several hospitalizations for episodes of paranoia, complex auditory hallucinations, and delusional religious beliefs. During her life, she has been managed with several antipsychotic drugs, and the last therapy was based on haloperidol decanoate injections (200 mg every 4 weeks), with residual symptoms consisting of minor delusions and few episodes of auditory hallucinations.
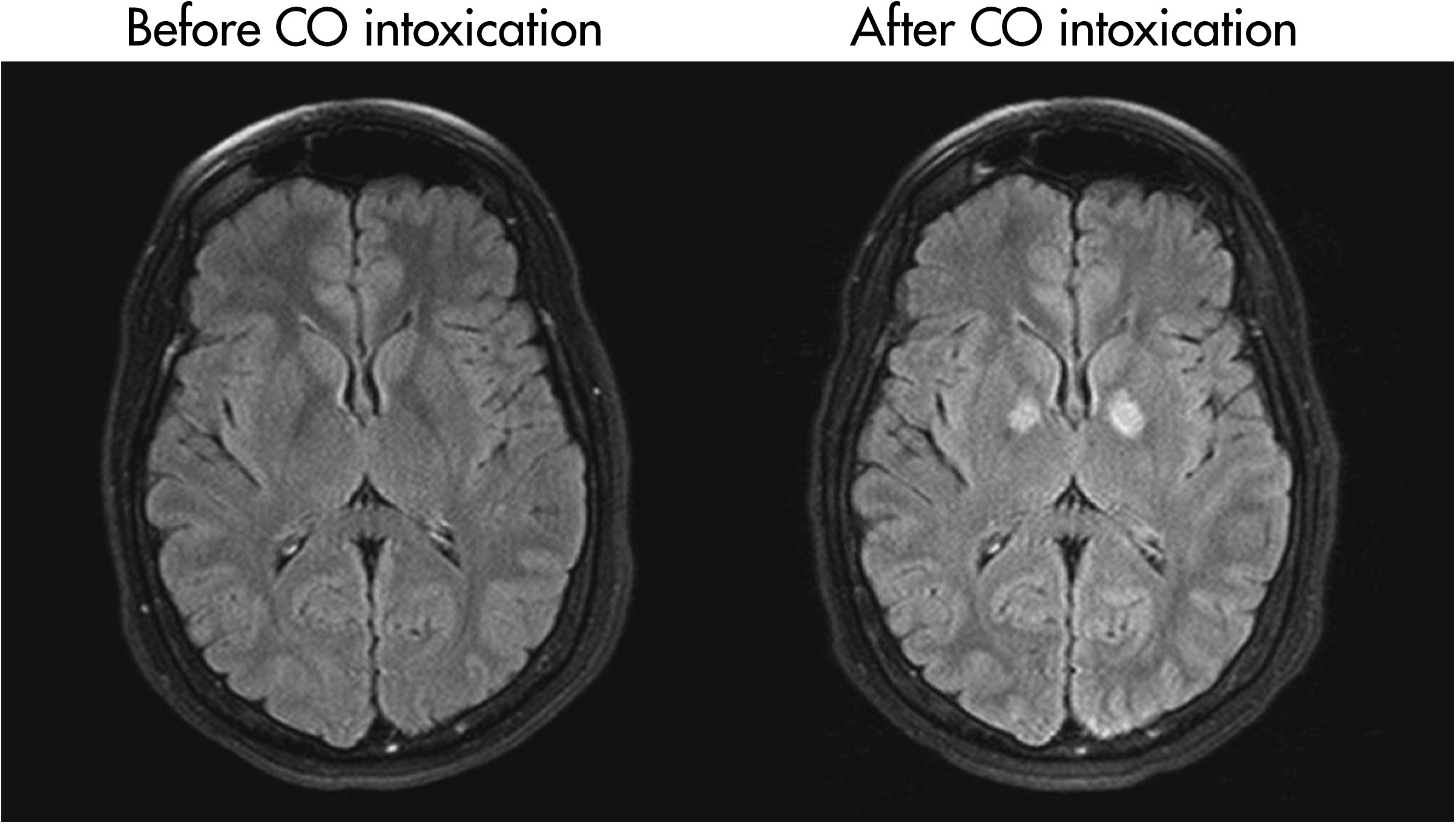
In December 2008, she was intoxicated with CO that caused an anoxic lesion of both pallidum structures, as shown in the MRI brain scan (
Figure 1). During hospitalization, she was unexpectedly relating better, without paranoid or any delusion, and therefore no antipsychotic treatments were prescribed. Surprisingly, after the hospital discharge and in the following 2 years of visit appointments, she was completely stable, with full sustained psychiatric remission.
This unexpected clinical observation shines a further light on the intimate involvement of BG in schizophrenia. Although we cannot definitely demonstrate a causal relationship between the CO-mediated pallidal lesion and psychotic compensation, the temporal association is highly convincing. In one of the most fascinating patho-physiological theories, in schizophrenia, the pallidum is placed in overdrive by the hippocampus unbalancing the two distinct firing patterns of dopaminergic neurons of the ventral tegmental area.
3 Particularly, the
tonic component (responsible for the “background” dopamine) release is impaired, causing a lower threshold of the system sensitivity to short-term
phasic increase of dopamine levels in response to behaviorally-relevant stimuli.
3Thus, the present case could support this patho-physiological theory of schizophrenia, leading to a picture in the future of a neuro-surgical approach for this disorder as extensively proposed in other psychiatric conditions.
4