To the Editor: Under critical circumstances, such as diffuse cerebral edema caused by major traumatic brain injury and ischemic and hemorrhagic stroke, a wide decompressive craniectomy (DC) saves life and might improve the long-term outcome. However, another nightmare begins in surviving patients because they must endure skull defects unless reconstructive surgery is performed. The gross external appearance of the skull after craniectomy negatively affects patients physically and mentally, especially young patients who are concerned about their appearance.
Advancements in the development of biomaterials have recently made various newly-designed implant options for the repair of skull defects after DC. Previously, we demonstrated craniofacial skeletal reconstructions with quantitative analysis of craniofacial symmetry as determined by the cranial index of symmetry (CIS) in re-formed polymethyl methacrylate (PMMA) and titanium cranioplasty. CIS scores of our patients were 95.86% (SD: 1.36; range: 94.2–98.5) and 97.98% (SD: 1.17; range: 96–99.8) in computer-assisted quantitative method for PMMA cranioplasty
1 and three-dimensional (3-D) titanium cranioplasty,
2 respectively. A CIS score >95% indicates symmetry. Although promising results indicate excellent cosmesis, and craniofacial symmetry of various new reconstructive implants, why isn’t CIS 100% in craniofacial reconstruction? Actually, the pivotal element of craniofacial symmetry is not solely restricted to implant reconstruction. Soft-tissue handling contributes to craniofacial symmetry as importantly as does implant reconstruction in cranioplasty for skull defects. However, little is known regarding the significance of soft tissue in calvarial reconstruction.
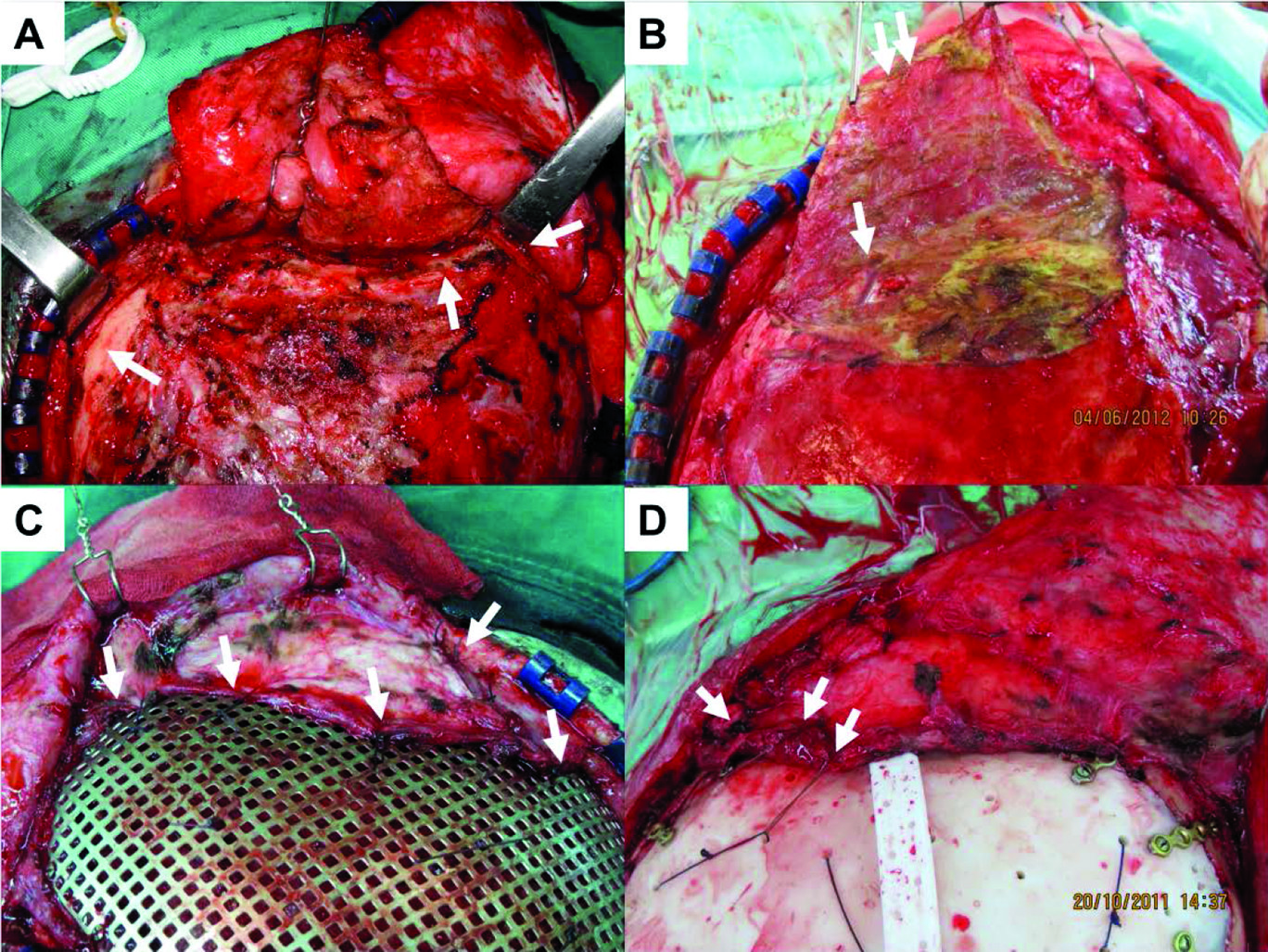
As far as the operative procedure is concerned, cranioplasty implants should be epidurally placed and can be anchored either to cover the skull defect or in apposition to the conjugation margin in respect 3-D titanium and PMMA cranioplasty. Therefore, the simultaneous modalities to manipulate soft tissue include thoroughly reflecting the temporalis muscle above the dura (epidural space), tissueless margins of the skull defect for enhancing implant reduction (arrows in
Figure 1 [A]), and preventing immoderate soft-tissue dissection adjacent to the implant’s edge.
The temporal branches of the facial nerve lie on the deep surface of the temporoparietal fascia. Thus, we suggest that the entire temporalis muscle above the dura be completely reflected (double arrow in
Figure 1 [B]) to prevent facial nerve injury. Furthermore, the more superficial soft-tissue bulk we could preserve, the less soft-tissue atrophy, and the better maintenance of the outer appearance. For temporalis muscle reflection, the difficulty lies in dissecting epidural muscle tissue without dural tearing. At least, intact arachnoid membrane (single arrow in
Figure 1 [B]) is necessary for the prevention of cerebrospinal fluid (CSF) leakage. More importantly, after the insertion of implants, the reflected temporalis muscle is tacked in place and reattached to the implants, using suspensory vicryl sutures to restore its original anatomy (arrows in
Figure 1 [C] and [D]).
To obtain good soft-tissue handling, proper surgical technique to manipulate soft tissue is mandatory in craniofacial reconstruction for skull defects. On one hand, we should completely reflect epidural soft-tissue bulk to preserve a potential soft-tissue pool for later degenerative atrophy. On the other hand, we should dissect only adequate soft tissue over the skull defect margin to prevent damage to muscular, vascular, and neurological structures.