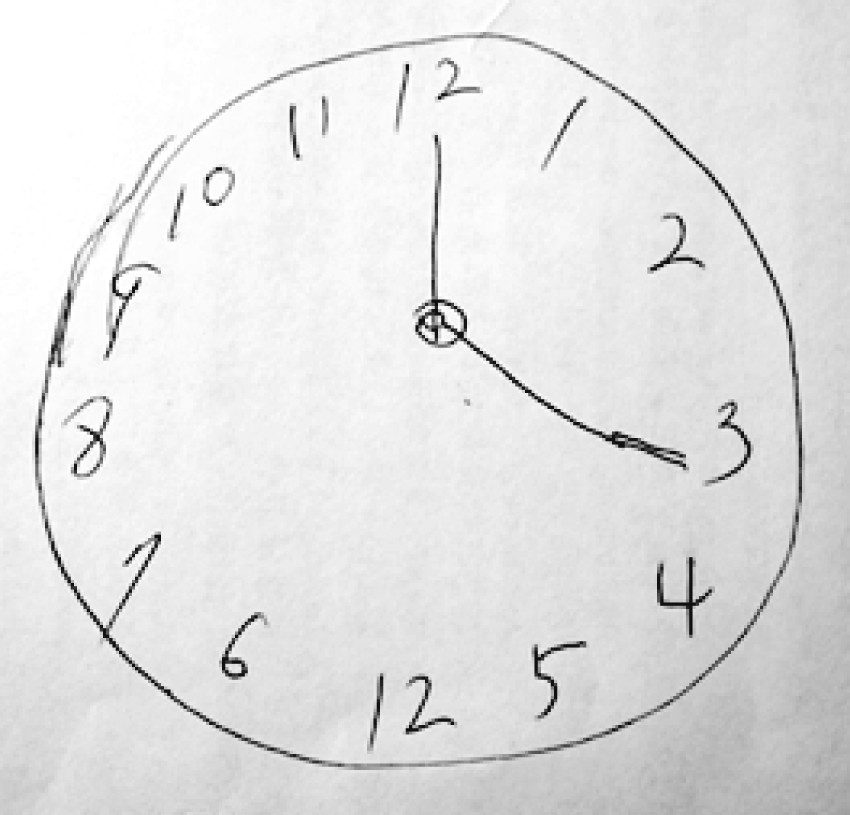
To the Editor: A 60-year-old woman without previous mental illness had presented symptoms of insomnia, somatic discomforts (including soreness of the teeth, epigastralgia, and soreness of the bilateral arms), decreased energy, poor appetite, diminished functionality, and a feeling of hopelessness, worthlessness, frequent weeping, and suicidal ideation for 1 year. She was treated with antidepressants under the diagnosis of major depression. Because of resistance to serial antidepressant treatments and persistent suicidal ideation, three successive courses of electroconvulsive therapy (ECT), with 27 fractions in total, were administered at a local mental institution. Although a dramatic response to the ECT was reported by her family, she soon relapsed into the same depressive state 1 week after the ECT. When she was referred to our hospital for further treatment, she was found to have psychomotor agitation and impaired cognition, including apraxia (e.g., she could not sew and cook as before) and obvious errors in the Clock-Drawing Test (
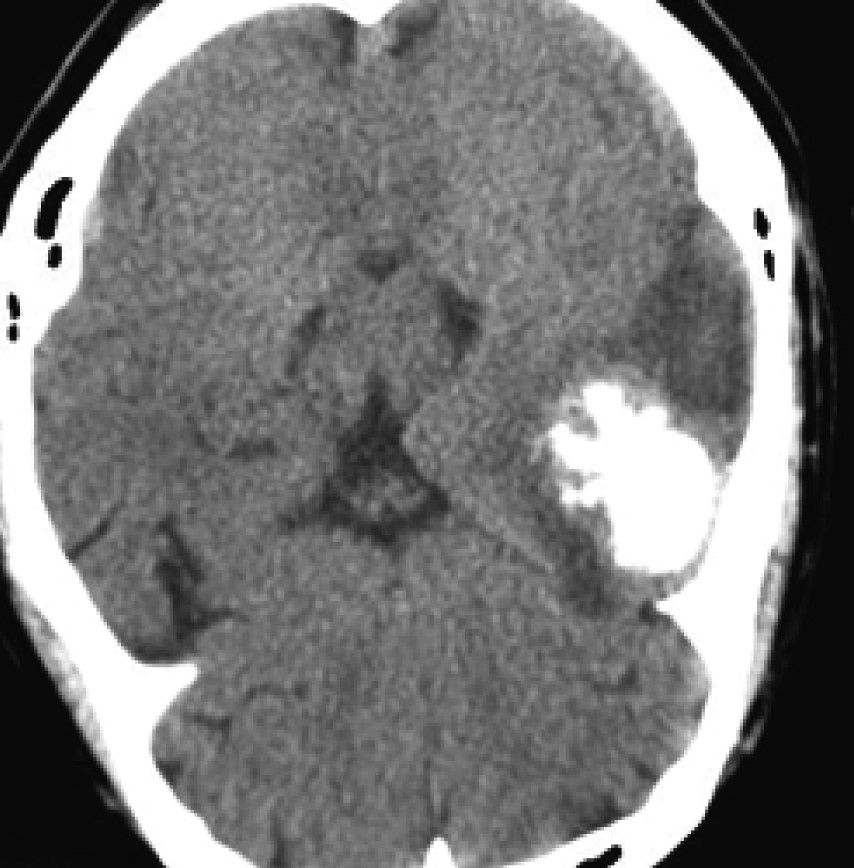
Figure 1). Under the impression of organic mental disorder or dementia, the patient was examined with cerebral computed tomography (CT), which revealed an intracranial mass in the left anterior temporal base. The mass was 40 mm in maximum diameter, with perifocal edema and a midline shift to the right hemisphere (
Figure 2). The intracranial mass was completely removed with neurosurgical intervention, and pathological examination confirmed the diagnosis of meningioma. However, most of the depressive symptoms, including somatic complaints, restlessness, feelings of worthlessness and hopelessness, and suicidal ideation, persisted for at least 9 months after the surgery, when only partial improvement in daily life activity, such as folding clothes, washing dishes, and talking about TV shows, was noted by her family.
Discussion
Mental symptoms caused by meningioma vary, and are usually related to the location and size of the mass and the time-course over which the tumor develops. Most meningiomas grow very slowly and are often asymptomatic. Depression is not uncommon in patients with intracranial neoplasm, and may possibly be misdiagnosed as mood disorder when no neurological deficit can be detected.
1 In this case, cognitive impairment with apraxia was the key symptom leading us to consider the possibility of organic mental disorder or dementia, so a neuroimaging study was arranged. Beyond our expectation, the patient remained depressed 9 months after removal of the meningioma. Correlation between the edema volume of the intracranial meningioma and the sequelae of coexisting psychiatric disorders has been reported.
2 The refractory depression in this case might have been related to a more severe peri-lesional edema that might have been aggravated by repetitive ECT, resulting in an irreversible injury. Thus, we suggest that caution be taken in the diagnosis of new-onset depression, especially in those cases with cognitive impairment and resistance to pharmacotherapy.