To the Editor: Moyamoya disease is a progressive cerebral vasculopathy of unknown etiology, characterized by severe bilateral stenosis/occlusion of the main arteries of the circle of Willis, with a pattern of collateral vessels that look like a “puff of smoke” on angiography.
1 It is more common in Asian populations and more prevalent in women.
1 The diagnosis peaks in two age-groups: children approximately 5 years old, and adults in their mid-40s.
1 It may have variable clinical presentation: ischemic stroke, transient ischemic attack, intracranial hemorrhage, headache, seizures, involuntary movements, cognitive deficits, and psychiatric changes.
1 In adults, it usually presents with intracranial hemorrhage or ischemic symptoms.
2 Acute cerebral ischemia occurring after intracranial bleeding has rarely been reported and is not well understood.
2,3 We describe a case of hypoperfusion encephalopathy after intracerebral hemorrhage occurring as the first manifestation of moyamoya disease.
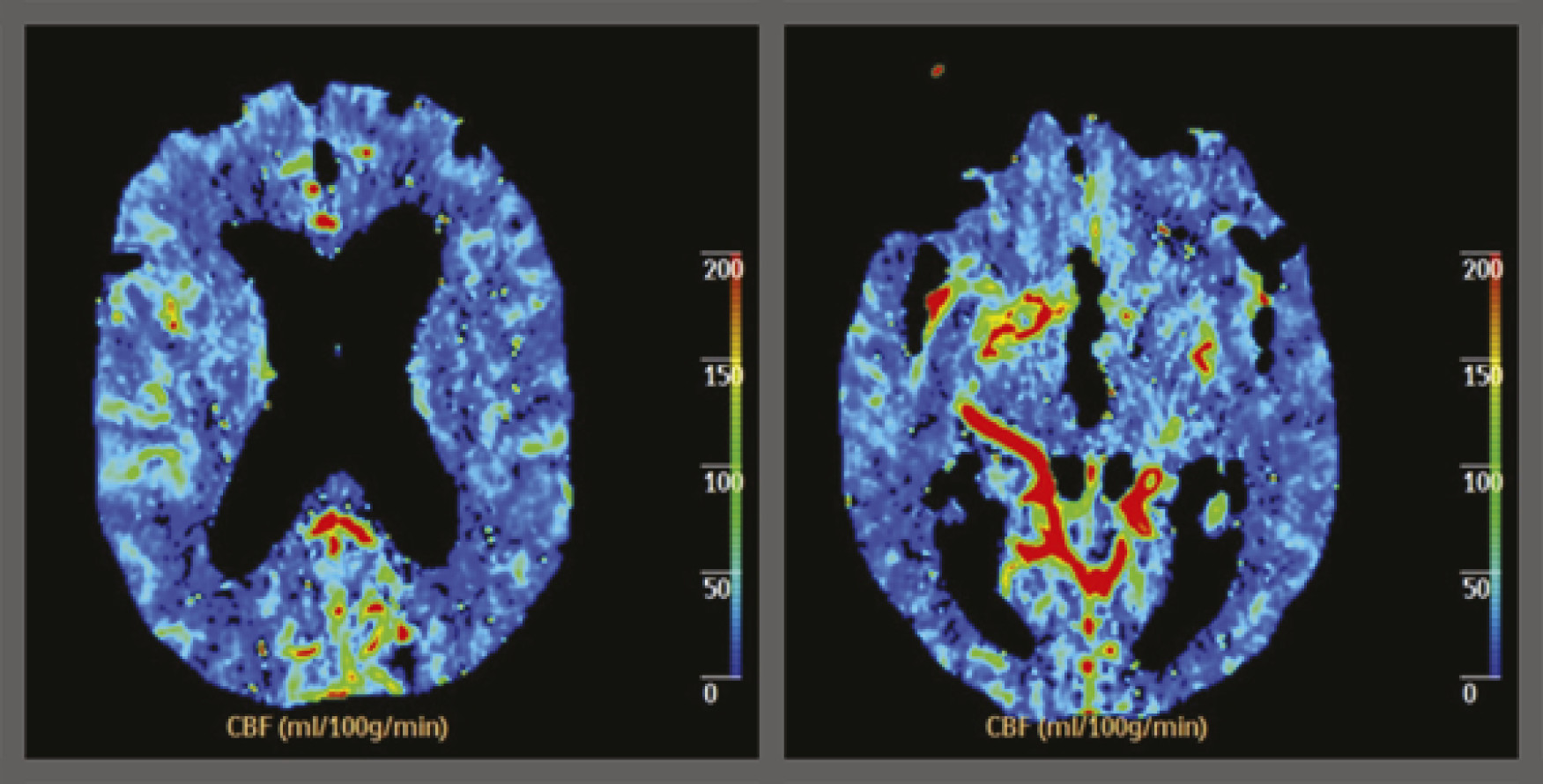
A 77-year-old male patient, with a long-standing history of uncontrolled hypertension, was admitted to our stroke unit upon being found unconscious. His blood pressure was 174/100 mmHg and Glasgow Coma Scale rated 3 (no eye opening, no verbal response, no motor response), with reactive pupils and right extensor plantar reflex. Computed tomographic (CT) scan showed left basal ganglia hemorrhage, extending into the ventricles and subarachnoid space. Antihypertensive and hyperosmotic therapy was started, and the initial evolution was favorable, with recovery of consciousness, confused verbal response, and right hemiparesis Grade 3 (MRC). By Day 14, multifocal myoclonus appeared, with decreased arousal and ensuing severe encephalopathy. Follow-up CT revealed hemorrhage reabsorption and no hydrocephaly. Laboratory studies were unrevealing. An electroencephalogram showed only slow background activity (5–6 Hz). Infections, metabolic, and toxic causes were also excluded. Brain diffusion-weighted imaging (DWI) MRI was negative for acute ischemic lesions. At this point, hypoperfusion encephalopathy was suspected and confirmed by perfusion CT (
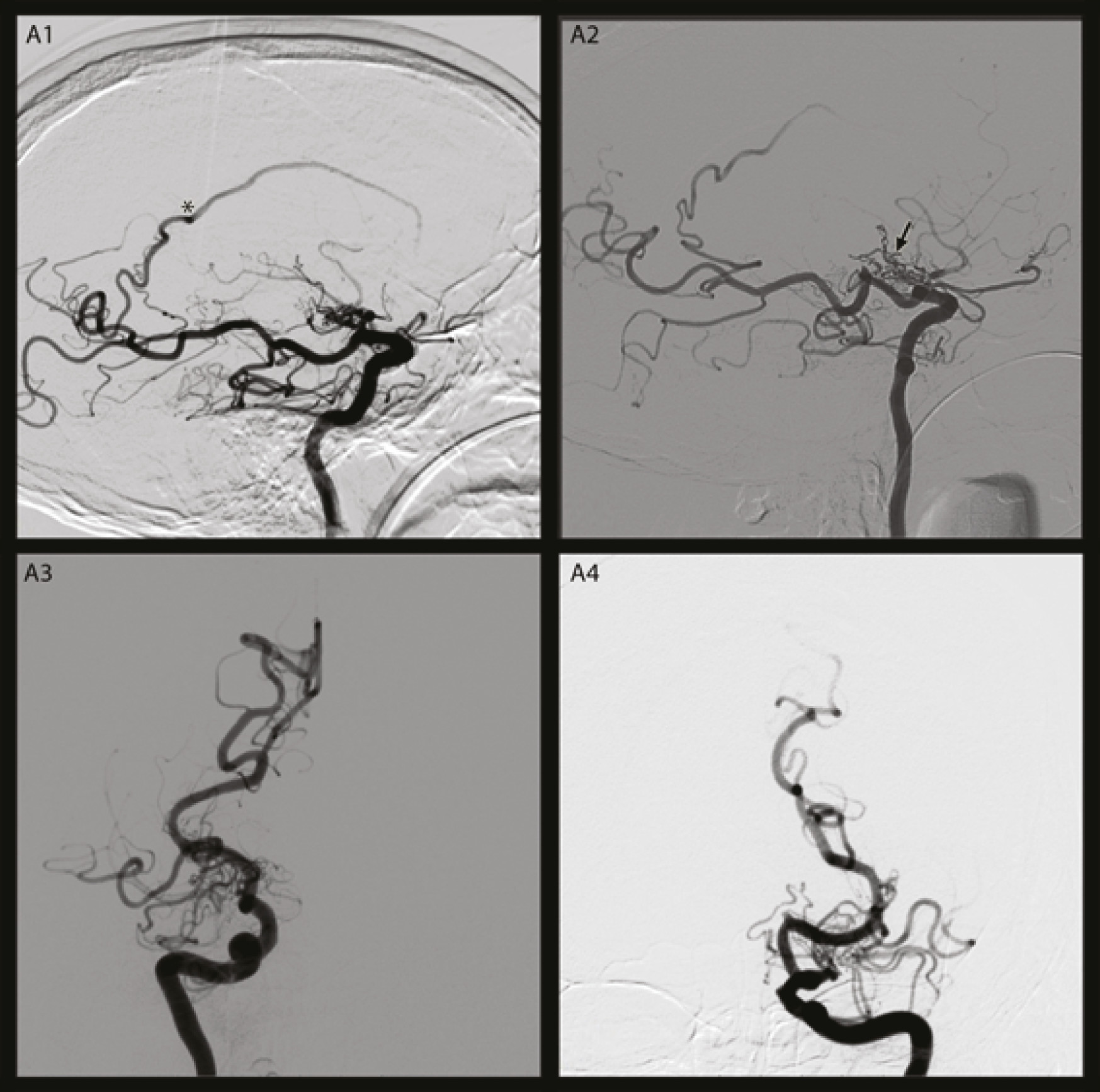
Figure 1). CT angiography disclosed stenosis of the distal intracranial internal carotid artery (ICA) bilaterally, extending to the proximal anterior (ACA) and middle cerebral (MCA) arteries. Moyamoya disease was diagnosed and was classified as Grade IV (Suzuki Grading System) by conventional angiography (
Figure 2). Because of his clinical condition, revascularization was not considered.
We report this case because of the rarity of moyamoya diagnosis in elderly persons and because of the atypical presentation. Our patient seemed to be permanently “fainted;” he had global hypoperfusion, but no real ischemic changes. The initial manifestation was interpreted as a hypertensive intracerebral hemorrhage. Later, when we detected hypoperfusion encephalopathy, Moyamoya was diagnosed. Vasospasm, in association with both subarachnoid and intraventricular hemorrhage, and hypotension and dehydration, resulting from the administration of hyperosmotic agents to control hemorrhage-related increased intracranial pressure, may have caused hemodynamic compromise, being possible contributing factors to the hypoperfusion encephalopathy in our patient. Other factors, such as hypocapnia and shrinkage of the moyamoya vessels, have also been proposed as mechanisms in acute cerebral ischemia occurring after intracranial bleeding.
2,3 The initial clinical presentation of hemorrhage and the presence of severe bilateral ICA stenosis affecting cerebral perfusion are predictors of very poor outcome in our patient.