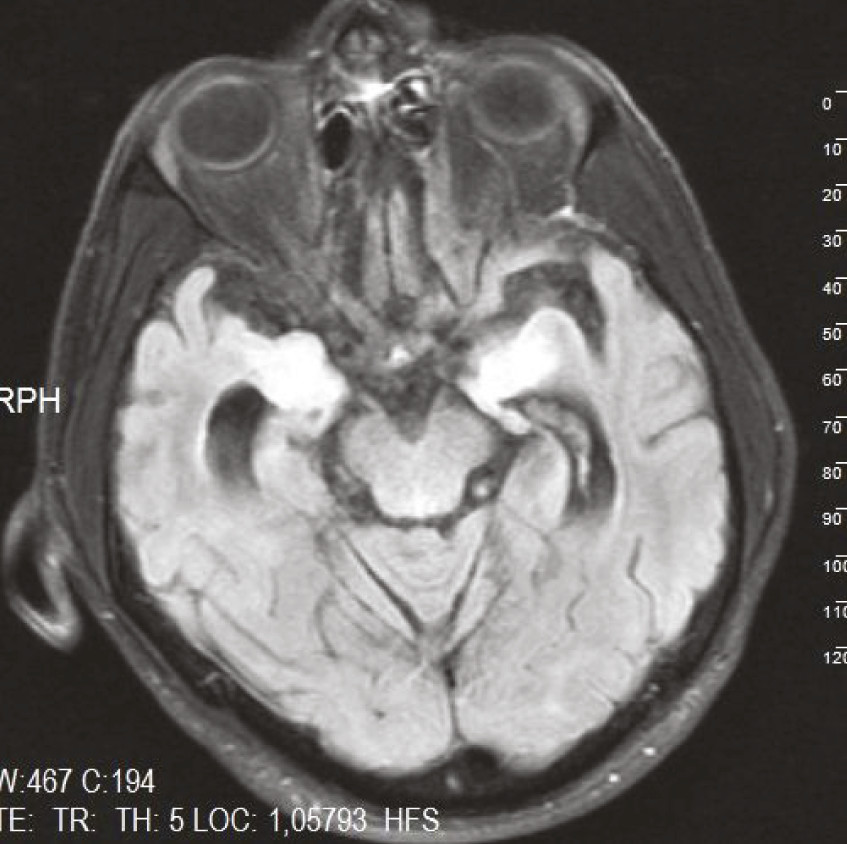
A 49-year-old man without a family history of psychiatric or neurologic illness was referred to our psychiatry clinic because of memory impairment, speech disturbance, aggressiveness, insomnia, suicidal behaviors, self-mutilation, apathy, hyperphagia, disorganized behaviors such as undressing and urinating in improper places within the last 2 years. Lately, he became dependent on caregivers and could not run his transporting business. A year ago, before his hospitalization, he was referred to an outpatient neurology clinic and diagnosed by cranial magnetic resonance imaging (MRI) with frontotemporal dementia (findings of hyperintense signal changes on both mesial temporal lobes [
Figure 1]). Because there was no improvement in his clinical status after paroxetine 20 mg/day and risperidone 1 mg/day treatment, and because of increased behavioral changes and a suicidal attempt, the patient was hospitalized. He was apathetic and uncooperative during the psychiatric examination. Memory loss and disorganized behaviors were apparent. A minimally increased muscle tone, increased deep-tendon reflexes, bilateral extensor plantar responses, and a slight ataxic gait were noticed at neurological examination. Mini-Mental State Exam (MMSE) score was 9. Risperidone was continued at a dose of 2 mg/day. Laboratory results were unremarkable, except that the venereal disease research laboratory test (VDRL) and treponema pallidum hemagglutination assay (TPHA) were positive, at 1/64 and 1/10,240 titers, respectively. Cerebrospinal fluid examination showed 20 lymphocyte/mm
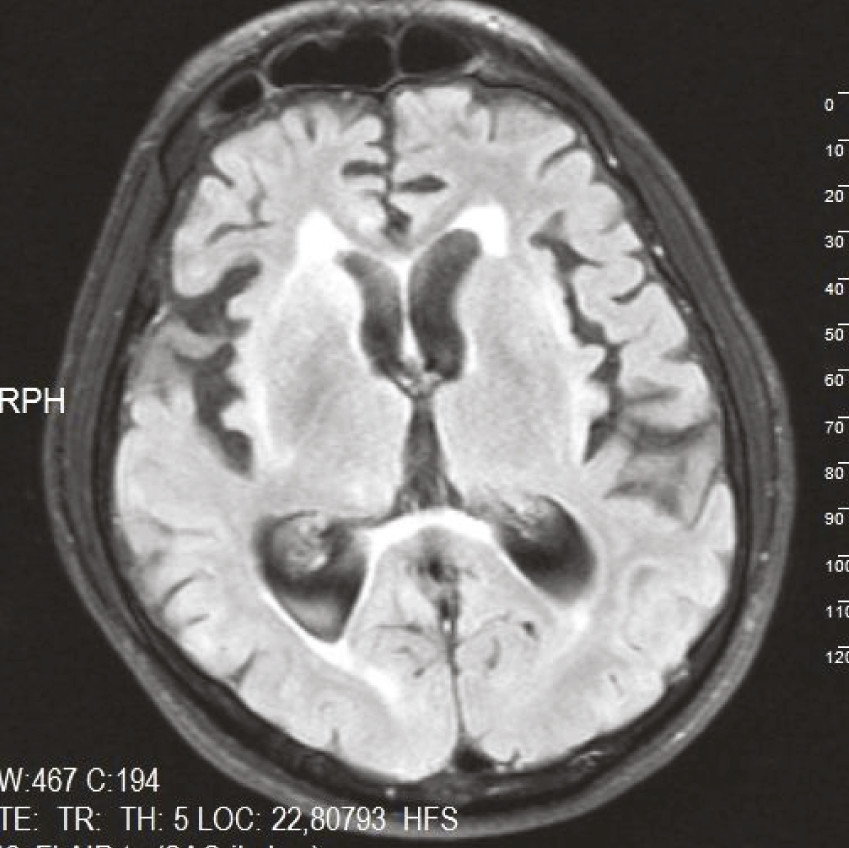
3, protein 52.4 mg/dl, glucose 56 mg/dl; TPHA test was positive, at 1/10,240 titers. Serological tests for human immunodeficiency virus, hepatitis B/C, and Brucella agglutination test were negative. A repeat cranial MRI showed cerebral atrophy, triventricular hydrocephalus, and periventricular lesion (
Figure 2). The patient was started on ceftriaxone (2 g/day intramuscular) for 14 days. His ataxic gait regressed after treatment, but neuropsychiatric symptoms remained unchanged. A recent psychiatric examination revealed emergence of psychotic symptoms, and so quetiapine 900 mg/day was initiated.
General paresis, or dementia paralytica, is seen in the late stage of neurosyphilis. Behavioral changes, psychiatric disorders, and dementia can occur in this stage, and, if untreated, death may occur within 3–5 years.
1 Neurosyphilis is a treatable disease if it is diagnosed early. In our patient, dementia and behavioral problems persisted even after antisyphilis treatment because of delayed diagnosis. Our case underlines the importance of early diagnosis and treatment of neurosyphilis.