To the Editor: Guillain-Barré syndrome (GBS) is a demyelinating polyneuropathy disorder, characterized by neurologic deficits mainly related to processes affecting nerve fibers, namely segmental demyelination and axonal degeneration. Acute motor axonal neuropathy (AMAN) is one of the subtypes of GBS with damage only to the motor nerve. It is usually caused by
Campylobacter jejuni, cytomegalovirus, or
Haemophilus influenzae infection, and rarely by cerebral trauma and injection of monosialotetrahexosylganglioside sodium.
1–3 Herein, we report a rare case of AMAN caused potentially by a combination of cerebral trauma,
Campylobacter jejuni infection, and injection of monosialotetrahexosylganglioside sodium.
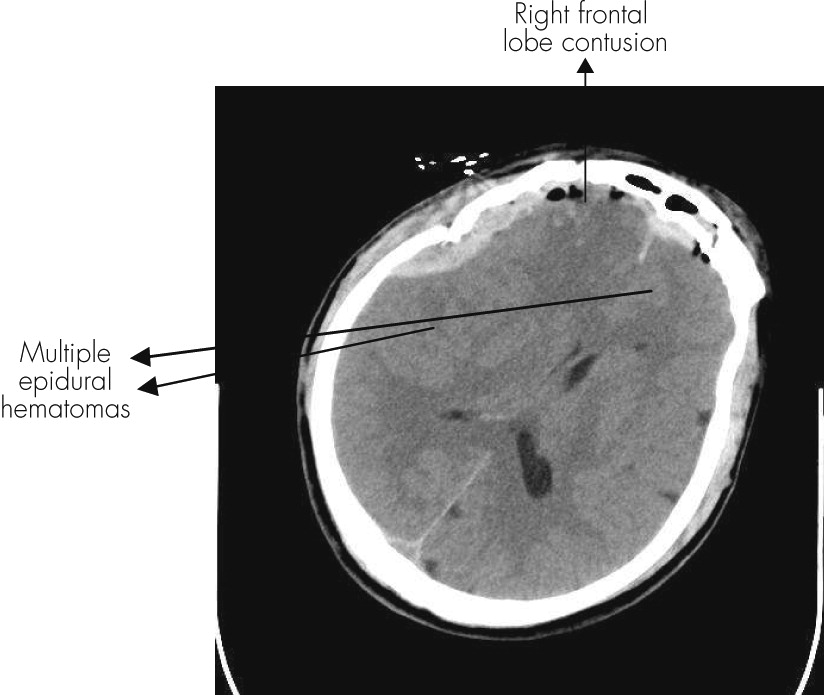
A 56-year-old man was hospitalized after suffering a fall injury (from 2 m) on May 25, 2011. CT examinations showed multiple epidural hematomas within cranium and brain, and contusion and laceration within the right frontal lobe (
Figure 1). There were no fractures and no dislocation in the cervical vertebra. The evacuation of epidural hematomas was performed, and the patient was awake after the operation. CT re-examination showed that the contusion and laceration within the right frontal lobe of the brain had no alteration. Sometimes the patient had metal symptoms without significant physical dysfunction and abnormal feelings. The patient was administered monosialotetrahexosylganglioside sodium (40 mg) together with 250 ml of NaCl injection per day. The patient suffered from diarrhea for 1 week and was treated with routine therapy. The mental status of the patient had significantly improved after treatment.
The weakness in the upper limbs occurred suddenly with grade 0 muscle strength and hyperalgesia. MRI scan of the cranium and the brain revealed contusion, and laceration within the right frontal lobe of the brain was same as that after the operation. MRI scan of the spinal cord showed no significant abnormality. After 1 day, grade 0 muscle strength of lower limbs appeared with hyperalgesia, and flaccid paralysis with all four limbs occurred. Pathological sign on both sides was not shown. The patient also suffered from hoarseness and bucking. Leukocyte and neutrophil granulocyte counts were high, and lymphocyte count was lower without hypokalemia. Protein level was increased without alteration in cell numbers as found by CSF analysis, showing that the albumin cytological dissociation existed. The result from Campylobacter jejuni culture was positive. Electromyography (EMG) examination measuring separately on median nerve, ulnar nerve, common peroneal nerve, and tibial nerve showed that motor nerve conduction velocity (MCV) was reduced and F-latency was extended. The sensory nerve conduction velocity (SCV) was normal. The diagnosis was GBS subtype AMAN. The proposed treatment was to administer 25 g γ-globulin per day. However, relatives of the patient refused the treatment because of family reasons. Dyspnea and weakness occurred; the patient died 1 day later.
In summary, cerebral trauma, Campylobacter jejuni infection, or monosialotetrahexosylganglioside sodium may be the cause of AMAN for this patient, making it a very rare case. Although inevitable causality between administration of monosialotetrahexosylganglioside sodium after cerebral trauma and GBS could not be obtained, this case suggests that at least we should be more careful when monosia otetrahexosylganglioside sodium is administrated after cerebral trauma.