To the Editor: Neurosarcoidosis is a rare neurologic disorder. Patients with neurosarcoidosis can develop psychiatric features including hallucinations, delusions, disorganized thoughts, and aggression.
1 To the best of our knowledge, tilted vision and delusional perception have not been reported as symptoms in neurosarcoidosis.
Case Report
The patient is a 66-year-old right-handed woman with a documented history of neurosarcoidosis who initially presented because of an episode of acute onset of aggression, tilted vision, and delusional perception. She had significant neurological symptoms including impairment in repetition, naming, word-finding, paraphasic errors, and short-term memory. The patient had been treated with prednisone and methotrexate, resulting in stabilization of pulmonary and cutaneous symptoms; however, she continued to experience neuropsychiatric symptoms of increased paranoia, aggression, and mood lability, as well as a recurrent visual hallucination of a woman walking between two colored points.
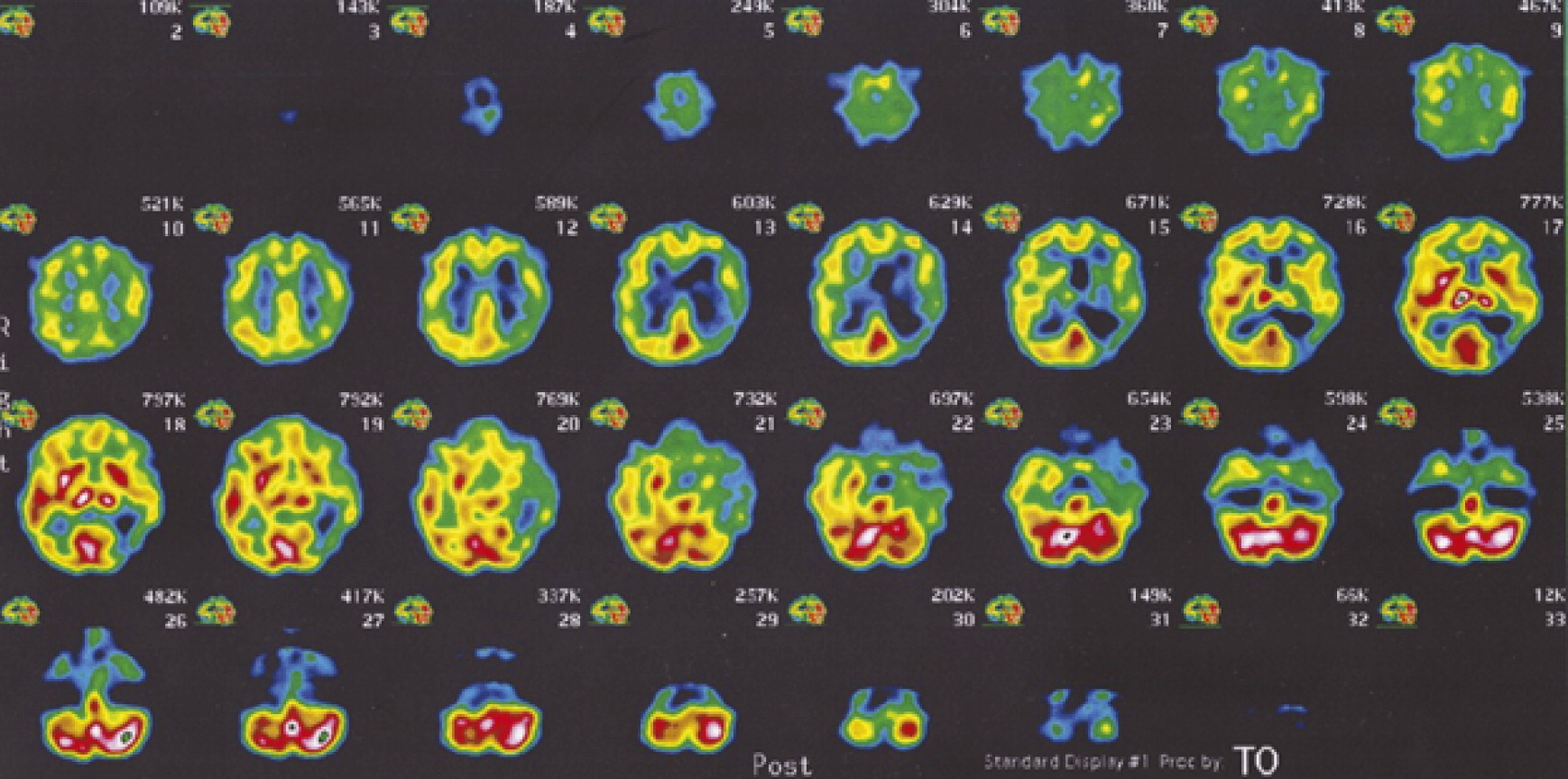
The patient was transferred to the psychiatric unit from the neurology service because of increasing aggression and delusions. She reported visual misidentifications where familiar patterns seemed to appear in everyday objects, as well as a clockwise tilt in her visual field of approximately 10–20 degrees. She described seeing familiar patterns created by household objects, such as bottles “transformed” into the shape of her husband’s belt buckle. The patient felt most disturbed by a delusion that her husband had arranged objects according to specific patterns, in particular placing bottles in the kitchen cabinet so that “the bottles were all on a slant” and “pushed back.” The patient believed that these perceived rearrangements were signs of either her husband being medically ill or strangers entering her house. Work-up was initiated, including imaging, laboratory testing, and cognitive examination. The rest of the MSE findings demonstrated decreased cognitive functioning, including difficulty with stating the digit span backward, copying a three-dimensional cube, and clock drawing. Prior neuropsychological testing had demonstrated difficulty with processing speed, complex attention, memory, and aspects of executive functions. MRI and single-photon emission computed tomography (SPECT) studies demonstrated extensive white matter changes, areas of calcification in the left parieto-occipital lobe, and decreased perfusion of the left parietal and temporal lobes (
Figure 1); laboratory tests of blood and CSF supported the diagnosis of neurosarcoidosis. The patient’s insight into her condition improved slightly with discussion of how her psychiatric symptoms, and neuroimaging were connected with the known diagnosis of neurosarcoidosis. She was started on a low dose of risperidone, with improvement and discharge to outpatient psychiatric care.
After hospitalization, she continued to have episodic mood lability, aggression, and confusion, complicated by an ischemic stroke. She had another psychiatric admission for increased aggression and delusional thinking toward her husband. She has responded well to ziprasidone, which was started during this hospitalization period, with no major side effects.
Discussion
The patient presented above reported a slight tilt to her vision, particularly noticeable with objects that she knew were supposed to be vertical (i.e., books, bottles, utensils). Tilted vision and visual metamorphosis can occur because of a variety of lesions, though these symptoms have predominately been reported in patients with parieto-occipital regions or in the vestibulo-cerebellar system.
2 Similar to our patient, most cases of tilted vision are transient. The primary visual cortex appears to be spared.
3Psychosis in neurosarcoidosis is well-documented, though relatively uncommon. In this case, our patient had both visual hallucinations and delusional perception that her perceived visual metamorphosis was an indication that her husband’s health was failing. Her report of visual hallucinations may be attributed to lesions of her temporal, parietal, and occipital lobes on MRI/SPECT; some studies indicate that both parietal lobes play a role in the psychotic symptoms of schizophrenia, including some consideration that hypoactivity in the left parietal lobe may correlate with difficulties ascertaining agency over actions or perceptions.
4 A similar problem with attribution of symptoms and agency may in part explain the delusional symptoms in this case.