To the Editor: Kleine-Levin syndrome is a rare disease characterized by recurrent episodes of hypersomnia, hyperphagia, and hypersexuality.
1–4 Cognitive deficits usually occur. This condition may be primary, also called idiopathic, or secondary to other neurological disturbances.
1–4 The authors describe the case of a 61-year-old Brazilian man presenting with Kleine-Levin syndrome after being submitted to a neuroendoscopic approach for tumor removal and discuss the main aspects of the pathophysiology. During colloid cyst and clot manipulation and removal, there may have been injury to structures near the foramina of Monro and third ventricle, which probably initiated Kleine-Levin syndrome. The symptoms were transient, and after 6 months, the patient is almost at the preoperative status. The course of symptoms encourage us to follow such patients, because there is often a pattern of reversibility. To our knowledge, this is the first case of documented Kleine-Levin syndrome following a neuroendoscopic approach for the treatment of a colloid cyst of the third ventricle.
Case
We describe the case of a 61-year-old Brazilian man presenting with intermittent moderate headache for 10 years with regular follow-up in an ambulatory setting due to a cystic lesion of third ventricle, suggestive of a colloid cyst. He was referred for previous arterial hypertension, dyslipidemias, and obstructive sleep apnea. The initial follow-up proposed conservative treatment once the patient was oligosymptomatic and responded to analgesic therapy.
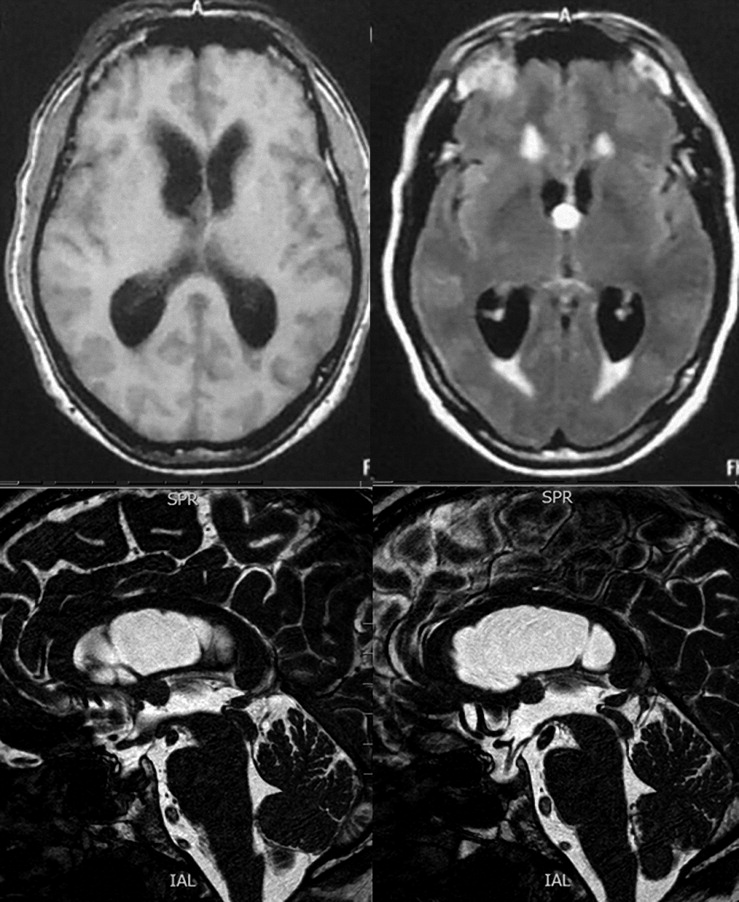
However, he sought medical attention because of subacute worsening of symptoms 2 months before surgery; he developed gait apraxia, memory disturbances, and urinary incontinence, together with worsening of headaches. New brain MR images revealed that the lesion was stable; however, a progressive hydrocephalus had developed (
Figure 1). Therefore, a surgical approach was proposed for lesion removal and treatment of hydrocephalus.
Surgery was performed with an endoscopic approach through a right frontal trepanation using a rigid neuroendoscope with a 0° lens. After reaching the lateral ventricle, a cheesy mass was visualized, obliterating the foramina of Monro. After gentle dissection and monopolar coagulation, the whole lesion was removed without evidence of a bleeding source. Nevertheless, in a matter of 2 hours in the immediate postoperative period, the patient presented with consciousness impairment.
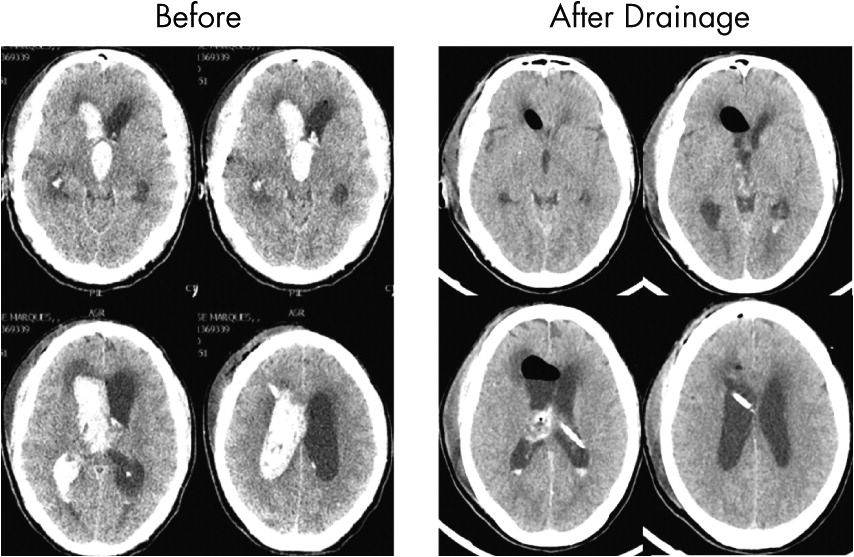
A skull CT scan was then performed, which showed the right hemoventricle. Thus, the patient was resent to surgery, which used the same approach to perform clot removal. After repetitive clot aspiration and cavity irrigation, hemostasis was achieved, and the patient remained sedated. A ventriculostomy catheter was also applied. Postoperative skull CT scans revealed satisfactory hematoma drainage, and the patient woke up with no neurological deficits (
Figure 2).
He was discharged, and in the early postoperative period developed hypersomnia, hyperphagia, and hypersexuality. A recent memory deficit was also present. The family reported that the patient was sleeping 18 hours/day. He also gained 15 kg in 3 months. Hypersexuality manifested as masturbation, obscene language, and excessive sexual advances toward his spouse. Although intense, the symptoms were not classified as socially inadequate by the family.
Polisomnographic recordings revealed an increase in the apnea/hypopnea index compared with studies performed previous to surgery (apnea/hypopnea index of 54/hour) and postoperatively (apnea/hypopnea index of 70/hour).
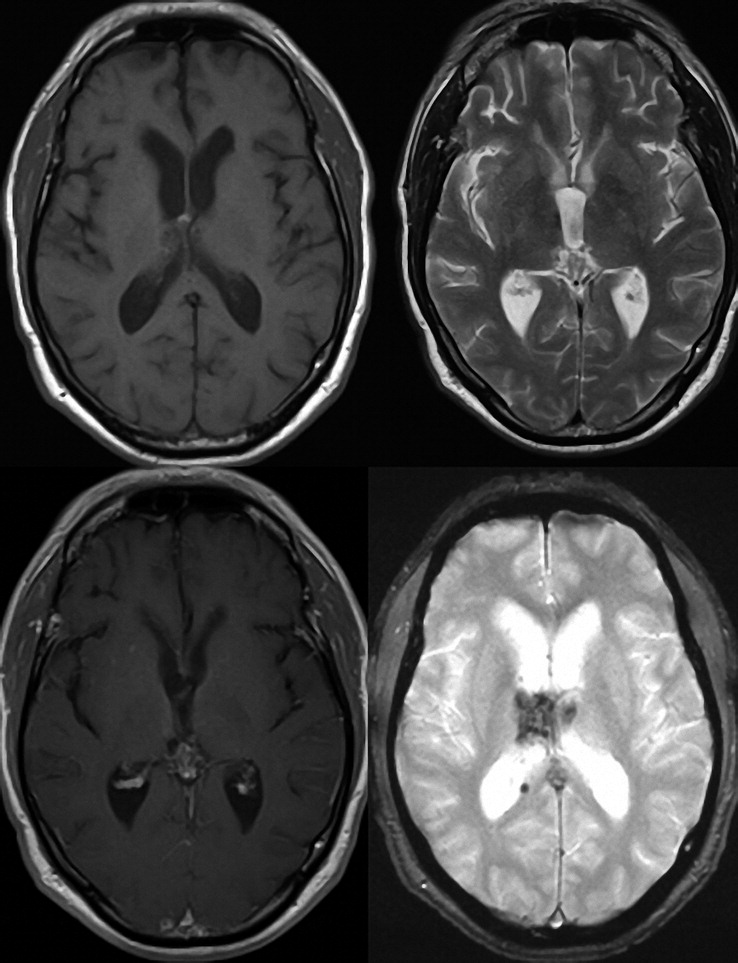
Four months after surgery, the patient remained with preserved neurological examination, and the symptoms of Kleine-Levin syndrome began to gradually vanish. He slowly regained his recent memory and returned to his previous dietary intake and sleep hours. His sexual behavior also normalized. Currently, 6 months after surgery, he has fully returned to his preoperative status and a new MR image showed only a scar in the topography of the right thalamus (
Figure 3).
Discussion
Kleine-Levin syndrome is a rare disease characterized by recurrent episodes of hypersomnia and, to various degrees, behavioral or cognitive disturbances, compulsive eating behavior, and hypersexuality.
1–4 Hypersomnia, a major clinical symptom of Kleine-Levin syndrome, is mandatory for diagnosis.
1–4 The usual sleep duration ranges from 12 to 24 hours/day. Polysomnographic recording results are generally not statistically different from those in independent samples.
3 Patients usually face cognitive disturbances such as confusion and concentration, attention, and memory deficits. Derealization, hallucination, delusion, mood disorders, and irritability may be present. Nearly half of patients can present with symptoms consistent with hypersexuality. These include masturbation, obscene language, fondling genitalia, and making unwanted sexual advances.
1–4Brain CT scans and MR imaging are often normal. Hormonal tests only occasionally reveal changes in the levels of pituitary hormones.
3The pathophysiology, although still unclear, involves hypoperfusion in diencephalic structures, especially the thalamus and hypothalamus.
3,4 Secondary Kleine-Levin syndrome is observed in association with stroke or posttraumatic brain hematoma, genetic or developmental diseases, multiple sclerosis, hydrocephalus, paraneoplasic syndromes, autoimmune encephalitis, or severe infectious encephalitis.
3In our case, we illustrate an atypical presentation of Kleine-Levin syndrome after repeated neuroendoscopic surgery. During colloid cyst and clot manipulation and removal, there may have been injury to structures near the foramina of Monro and third ventricle, which probably initiated Kleine-Levin syndrome. The course of symptoms encourages us to follow such patients, because there is often a pattern of reversibility.