To the Editor: Complex visual hallucinations consist of people, deformed faces, animals, and complex scenes, which are often associated with various clinical diseases such as delirium tremens, Parkinson's disease, dementia with Lewy bodies, Charles Bonnet syndrome, and schizophrenia.
1,2 Delusional parasitosis can be defined as a delusional syndrome that primarily affects middle-aged and elderly individuals (mainly women) and consists of the belief that parasites plague the skin.
3 Of historical note, Berrios
3,4 rediscovered the term
délire de zoopathie interne initially described by Dupré and Levy as a wider condition of delusion of parasitosis, which included the belief that one’s body was inhabited by all types of animals. The 29 cases reported by Dupré and Levy involved rats, birds, snakes, and other animals, but no insects were mentioned.
3,4 It seems likely that animals such as rats and birds appeared smaller than usual in the delusion of parasitosis, suggesting the coexistence of micropsia. Micropsia is one of the metamorphopsias and is defined as a symptom of objects appearing smaller than usual. Micropsia has been attributed to a dysfunction of object constancy within the temporal lobe, but lesions of the lateral occipitotemporal cortex may also cause micropsia, which may relate to a deficit of object processing rather than constancy.
5 To our knowledge, there are only two case reports showing complex visual hallucinations and coexistent delusional parasitosis.
6,7 We report a third case and discuss the mechanism of coexistence from the viewpoint of micropsia.
Case Report
A 74-year-old woman began to see insects and animals in her food and became very reluctant to eat a meal. She also started seeing insects under her skin and had the tactile sensation of their crawling, burrowing, and biting; this made her believe that because she ate a meal containing the insects’ eggs, they had hatched in her body and moved beneath her skin. The patient frequently struck a desk with her arms to crush the insects under her skin, which eventually caused subcutaneous hemorrhages. She had a history of a left-sided meningioma, which had been surgically removed 17 years before, and a right putamen hemorrhage, which was surgically treated 5 years earlier.
The patient initially saw her family physician, and dementia with Lewy bodies was suspected as a possible diagnosis because she also showed mild cognitive dysfunction and complex visual hallucinations. Although she did not have a fluctuation in cognitive impairment or parkinsonism, donepezil 5 mg daily was started. In addition, perospirone 16 mg daily, aripiprazole 12 mg daily, and carbamazepine 200 mg daily (6 μg/mL) were gradually combined with donepezil, but her visual hallucinations and delusion of parasitosis persisted.
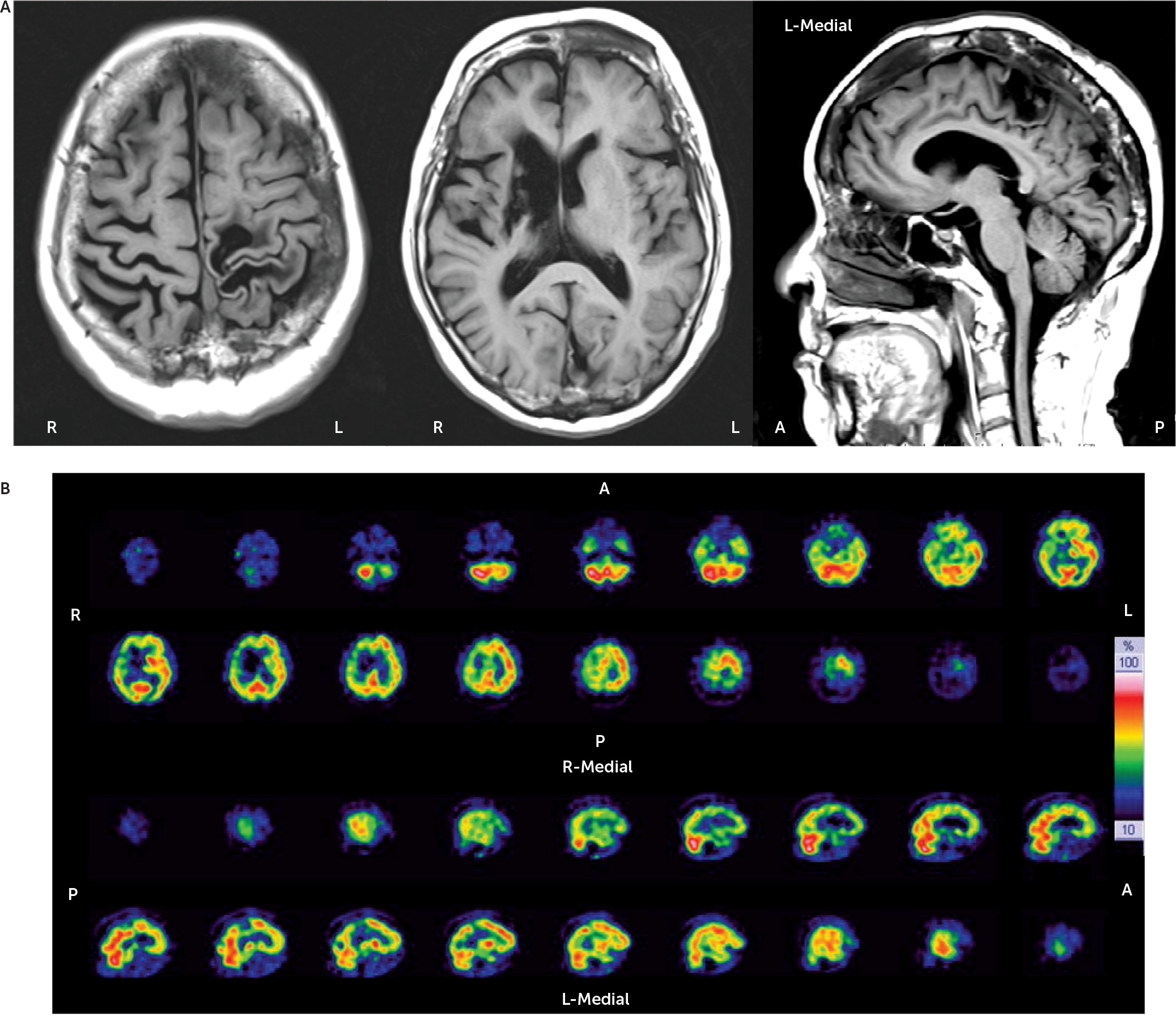
Finally, the patient was admitted to a psychiatric ward at our university hospital. She had no previous history of psychiatric illness, alcohol abuse, or illegal drug use. After admission, she complained of seeing blue and white insects, very small brown monkeys, and cats in her meal. The patient also saw maggots, centipedes, very tiny horses, dogs, cats, turtles, and insects with human faces beneath the skin of her arms. She often saw many scarabs on the wall and a cat beside her bed, all of which were nonexistent. She underwent brain imaging, and the results are shown in
Figure 1.
Olanzapine 2.5 mg daily was initiated and was gradually increased to 7.5 mg daily, which led to an improvement in the patient’s visual hallucinations. She began to be able to eat her meals. Because of the absence of side effects such as parkinsonism, olanzapine was further increased to 12.5 mg daily. She herself noticed that the number of insects and other animals clearly decreased in her meals and thereafter beneath her skin. Although visual hallucinations and delusion of parasitosis partially persisted, the patient developed insight to them and performed normal daily activities calmly. She was discharged home after hospitalization for 1 month.
Discussion
This patient experienced a variety of complex hallucinations, ranging from insects such as maggots to animals such as horses. In reality, horses are much larger than maggots; however, in the case of this patient, the horses she saw beneath the skin of her arms were scaled down to almost the same size as maggots. These hallucinations represent a type of micropsia of horses. It should be noted that this kind of micropsia was limited to the objects of visual hallucinations but not to those of the real world, suggesting the close distance between the neural substrates of visual hallucinations and micropsia.
Recent studies suggest that complex visual hallucinations can be found in association with any dysfunction of the eye to visual pathways and occipital visual cortices, especially Brodmann areas (BAs) 17, 18, 19, and 37.
8 Furthermore, BA19 is part of the occipitotemporal pathway that mediates the perception of size in relationship to distance, corresponding to micropsia.
9 In our patient, the left occipital lobe was largely damaged and the resulting impairment likely induced complex visual hallucinations; the impairment of BA19 and/or the occipitotemporal pathway was also assumed, probably leading to micropsia.
In addition, the right putamen was injured by infarction and hemorrhage. Among patients with stroke, delusions of parasitosis have typically been reported after lesions of the right temporoparietal cortex, thalamus, and putamen.
10 The putamen strongly influences visuotactile perception and contains bimodal visual and tactile receptive cells that project to the parietal (ventral intraparietal) cortex, primary somatosensory cortex, and premotor cortex. In our case, impairment of the right putamen and the adjacent area probably brought about the delusion of parasitosis.
In view of this patient’s psychopathology, it is interesting to consider the essentiality of micropsia in which large animals derived from visual hallucinations are made smaller and merge into the objects of delusion of parasitosis. Although both visual hallucinations and delusions of parasitosis can coexist independently, micropsia may facilitate the integrity of two different psychopathological symptoms in some patients. For other patients, the coexistence of visual hallucinations and delusions of parasitosis may be accompanied by micropsia, coincidentally.