Consumption of foods, such as yogurt, that contain probiotics has been associated with several beneficial effects. Probiotics are living microorganisms and may alter the host’s microflora.
1,2 Furthermore, the Food and Agriculture Organization of the United Nations has defined probiotics as live microorganisms that when administered in adequate amounts confer a health benefit on the host.
3 Meta-analyses of randomized controlled trials (RCTs) have confirmed that probiotics are beneficial for the treatment of many gastrointestinal diseases, such as antibiotic-associated diarrhea or irritable bowel syndrome.
1,4–6The benefits of probiotics seem to apply to more than just gastrointestinal conditions. Meta-analyses of RCTs have shown that probiotics can also lower fasting glucose,
7 decrease systolic and diastolic blood pressure levels,
8 and reduce the risk of eczema in infants.
9Animal data suggest that exposing mice to probiotics reduces anxiety and depression-related behaviors.
10 The vagus nerve may be an important pathway of communication between the bacteria in the gut and the brain, as evidenced by the observation that the effect of probiotic exposure was not found in vagotomized mice. The communication between gastrointestinal tract and the nervous system through gut microbiota is referred to as the microbiome-gut-brain axis.
11 Modifications to the gut microbiota with probiotics may therefore affect mood in humans.
12,13 In fact, the term psychobiotics has been introduced to describe live organisms that, when ingested in adequate amounts, work on the brain/gut axis to produce health benefits for sufferers of depression.
14We sought to assess the association of probiotic intake, through food or supplements, with the prevalence of depression, in a large population-based cross-sectional study.
Methods
We designed and conducted a cross-sectional analysis using data from the National Health and Nutrition Examination Survey (NHANES). NHANES is a national research program that collects health information from a representative sample of the U.S. population through interviews, medical examinations, and lab tests.
15,16Inclusion Criteria
Participants 18 years of age or older who participated in NHANES during the years 2005–2006, 2007–2008, 2009–2010, and 2011–2012, who responded to two 24-hour dietary recall interviews and to the depression questionnaire, were included. Each participant was only interviewed once since the NHANES survey is designed to examine a unique sample of persons in each 2-year cycle.
Assessment of Probiotic Exposure
NHANES has a dietary interview component with detailed dietary and dietary supplement intake information. The dietary intake data are used to estimate the types and amounts of foods and beverages consumed during the 24-hour period prior to the interview and to estimate the intake of energy, nutrients, and other food components from those foods and beverages.
The dietary interview component, termed What We Eat in America, is conducted as a partnership between the U.S. Department of Agriculture and the U.S. Department of Health and Human Services. In NHANES, all dietary interviewers were required to complete an intensive one-week training course and to conduct supervised practice interviews before working independently in the field. Retraining sessions were conducted annually to reinforce the proper protocols and technique. NHANES only provides dietary information for subjects considered to have reliable information. Subjects have an in-person interview and a telephone dietary recall interview 3–10 days following the in-person dietary interview.
17The types of probiotic foods included were: yogurt, buttermilk, kefir milk, and kimchi. Probiotic foods that may undergo heat-processing, which destroys live cultures, and foods that do not consistently contain live probiotics, such as frozen yogurt and yogurt-covered foods, were not included in the analysis. A total of 152 different types of probiotic supplements were included. Tables S1 and S2 in the data supplement accompanying the online version of this article describe the different food items and probiotic supplements included.
A subject was exposed to probiotics if he or she consumed a probiotic food or a probiotic supplement on either of the two interview days or a probiotic at least one day in the preceding thirty days. The latter assessment was based on a question that only applied to supplements.
Assessment of Depression
Depression was measured in NHANES with the Patient Health Questionnaire (PHQ-9). The PHQ-9 is a 9-item depression screening instrument that asks participants to choose one of four responses about frequency of depressive symptoms during the previous 2 weeks.
18 Subjects were classified as having depressive symptoms if PHQ-9 scores were ≥10. Scores ≥10 represent moderate or more severe depressive symptoms.
19 In addition, a score ≥5 was used to classify subjects with mild to more severe depressive symptoms.
18 The purpose of having two definitions of depression was to assess whether the definition affected the findings.
Assessment of Potential Confounders
Exposure to probiotics could be a proxy for characteristics of the subjects that make them less likely to have depression. These factors are age, gender
20, race/ethnicity, overall health, lifestyle, and socioeconomic status.
21–25Participants’ overall health status was determined by their answer to the question: “Would you say your health in general is excellent, very good, good, fair or poor”? This single, general, self-rated health question is an excellent indicator of the burden of medical conditions on an individual and is also a good predictor of mortality.
26,27Smoking, alcohol use, and eating habits likely reflect potential differences in lifestyle. Participants were classified as never, former, and current smokers. Current smokers were those subjects reporting at least 100 cigarettes in their lifetime and currently smoking every day or some days. Former smokers were those subjects who reported smoking at least 100 cigarettes in their lifetime but do not currently smoke. For alcohol use, participants were classified as never, former, and current drinkers. Current drinkers were those subjects reporting at least 12 drinks in their lifetime and currently at least 1 drink in the past 12 months. Former drinkers were those subjects who reported drinking at least 12 drinks in their lifetime and no drinks in the past 12 months.
A meta-analysis of observational studies found that a high intake of fruits, vegetables, fish, and whole grains was associated with a lower risk of having depression.
28 These types of food represent a healthy diet, high in fiber.
29 To control for the effect of a healthy diet, first we included total grams of fiber in the participant’s diet using the NHANES dietary interview data file. Dietary fiber is also associated with gut health and may impact probiotic survival.
30 Second, we included daily caloric intake
31, which also could be an indicator of lifestyle. A validation study showed that NHANES provides self-reported macronutrients that are within 10% of actual intake.
32Race/ethnicity was classified as self-reported African American, white, Hispanic, and other. Socioeconomic status was assessed through income. Income was grouped into four categories: very low, working class income, middle income, and high income, based on the participant’s response to the annual household income question. Very low income was defined as annual income <$15,000, working class as annual income between $15,000 and $34,999, middle as annual income between $35,000 and $74,999, and high income as annual income $75,000 or higher.
Association of Probiotics With Depression
To assess the association of probiotics with depression, we built unadjusted and adjusted logistic regression models with a binary outcome for depression (yes/no). In the adjusted analysis, potential confounders included were age, gender, smoking and drinking status, general health status, income, and daily total dietary fiber and caloric intake. Age, total grams of fiber, and caloric intake were included as continuous variables. The other potential confounders were included as categorical variables.
Sensitivity Analysis
To assess whether the source of probiotics affected the study results, we conducted a sensitivity analysis excluding subjects who were exposed to probiotics through supplements.
Exploration of Dose Response
To assess whether a dose response was observed, we used the maximum grams of probiotic food consumed in the in-person interview or in the telephone dietary recall interview. To avoid making an assumption of linearity, we created three categories based on the distribution of the variable.
Incorporating Complex Survey Design in the Analysis
To correctly account for the complex survey design, the analyses included the primary sampling unit variable (sdmvpsu) for variance estimation, the pseudo-stratum variable (sdmvstra) as the stratification variable, and the dietary two-day sample weight (wtdr2d) as the weight variable. NHANES provides sample weights to be used in conjunction with the data to allow analysts to produce estimates that are representative of the U.S. population. When combining multiple cycles of data, as in this study, the 2-year weights must be adjusted. Using the estimation procedure guidelines provided by NHANES, we multiplied the weight variable by 1/4 because we included four survey periods. STATA version 12.1 was used to conduct the analyses.
33The authors are employees of Janssen Research & Development. The manuscript makes no reference to any commercial product.
Results
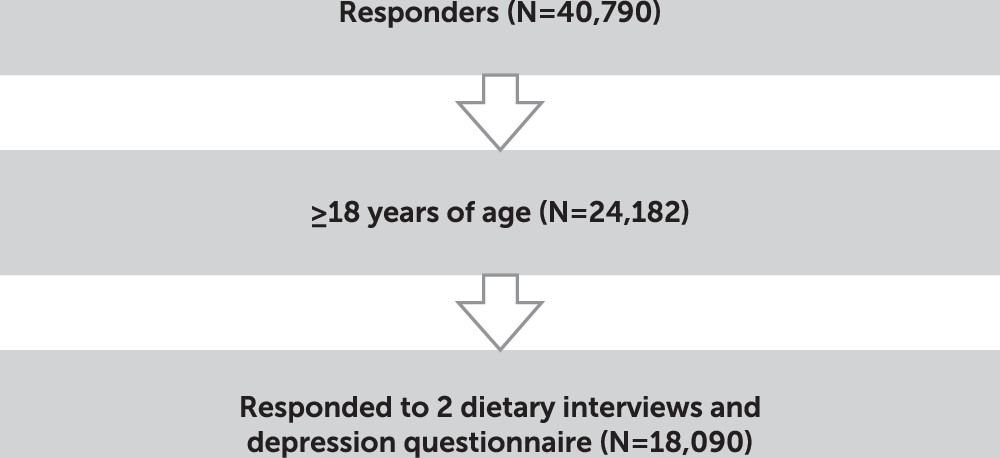
We included 18,019 subjects in the analysis, of whom 14.11% were exposed to probiotics. The participant flow diagram is shown in
Figure 1. Subjects in the probiotic group were more likely to be white, older, women, healthier, and to have higher family income. They also had a different lifestyle. Subjects exposed to probiotics were less likely to be smokers and had more fiber in their diet and fewer calories than subjects not exposed to probiotics (
Table 1).
Among subjects exposed to probiotics, 91.63% were exposed only through food, 6.53% only through supplements, and 1.85% reported exposure to probiotics through both food and dietary supplements. Among subjects who consumed yogurt or buttermilk, the mean intake was 112.87±76.46 grams over the 2 days.
Association of Probiotics With Depression
The overall prevalence of mild or more severe depression was 22.80% (PHQ-9 ≥5) and 7.59% for moderate or more severe depression (PHQ-9 ≥10). Subjects exposed to probiotics were less likely to have depression (unadjusted odds ratio [OR] for mild or more severe depression=0.69, 95% confidence interval [CI]=0.58–0.83; unadjusted OR for moderate or more severe depression=0.58, 95% CI=0.45–0.76).
After adjustment, the association between probiotic exposure and depression disappeared, irrespective of how depression was defined. For mild to more severe depression, the OR was 0.85 (95% CI=0.70–1.03), and for moderate or more severe depression, the OR was 0.82 (95% CI=0.61–1.1).
Excluding subjects who were exposed to probiotic through supplements did not affect the study results (see
Table 2).
After adjustment, women, current smokers, and subjects with very low income had higher odds of having depression. Participants with more grams of fiber in their diet had lower odds of depression. As health status decreased, the odds of depression increased. The strongest predictor of depression was poor health. Caloric intake and alcohol consumption were not associated with depression (see
Table 3).
Exploration of Dose Response
Probiotic consumption ranged from 0 to 1,071 grams on any one day. Dose response was examined by dividing probiotic intake categories based on the distribution of intake, where the lowest category (0 grams) included 86.81% of the population, the middle category (>0 and <170 grams) included 5.05% of the population, and the highest category (≥170 grams) included 8.14% of the population.
The unadjusted results show that both the middle and higher categories had lower odds of depression compared with subjects unexposed to probiotics. After adjustment for potential confounders, the association is attenuated and no longer significant. Greater levels of probiotic use were not associated with lower odds of depression (see
Table 4).
Discussion
We conducted a cross-sectional analysis on a large and representative U.S. population sample to assess the association of probiotic exposure with depression. We found probiotic exposure was associated with a lower prevalence of having depression, but when accounting for subject characteristics the association was attenuated and no longer significant. These findings suggest that it is not the probiotic exposure itself, but the attributes of subjects who consume probiotics, which lessen the odds of depression. In our study, subjects who consume probiotics are healthier, wealthier, exhibit characteristics of a healthier life style, have fewer risk factors for depression, and therefore are less likely to develop depression.
Major depressive disorder is being viewed as a psycho-neuroimmunological disorder that includes not only the traditional monoamine deficiency,
34 but also a persistent low grade inflammation.
35 Subjects with major depressive disorder have increased levels of a variety of inflammatory markers compared with those subjects who are not depressed.
35–38 The gut microbiota is now being viewed as a virtual endocrine organ that has bidirectional communication with the central nervous system through the microbiome-gut-brain axis.
39,40 Probiotics could directly, or through influence of other gut microbes, play a role in depression by inhibiting gut and systemic inflammation and activating the microbiome-gut-brain axis.
11,41,42 Probiotics directly protect the intestinal barrier; limit bacterial overgrowth in the small intestine; decrease systemic cytokines, oxidative stress, and inflammatory markers; and increase microbial production of GABA and other neurotransmitters.
Two very small randomized placebo control studies in healthy subjects
43,44 found that exposure to probiotics for a month decreased sad mood and symptoms of anxiety and depression. The results of this observational study are not consistent with those findings. This is a cross-sectional study: subjects were not followed over time, and NHANES dietary data identified food and supplement use over the 24 hour period preceding data collection and may not be reflective of usual intake. Although these data can provide insight, information on usual dietary practices collected over time would be expected to provide a stronger indication of associations between dietary factors and health outcomes.
The number of live microorganisms is relevant to assess the effect of probiotics on any health outcome. Although we excluded frozen yogurt because the number of viable bacteria could be very low and unreliable, we did not assess or control for the amount of bacteria. Although some yogurt manufacturers report culture levels at the time of manufacture, this is not a mandatory request and this number could vary dramatically from when the product is manufactured to when the product is consumed.
45 In addition, we did not asses the types of bacterial strain in the products consumed, even though the type of strain could be important.
46 These limitations could dilute the magnitude of the association between probiotics and depression.
The assessment of probiotics exposure was based on self-reported data. While NHANES uses a validated instrument for data collection (automated multiple pass method),
47 subjects underestimate habitual energy intake,
48 and therefore could underestimate the amount of probiotic food intake. This bias could lead to a failure to detect a dose-response association between probiotics and depression.
In this study we considered a subject as being exposed to probiotics if the subject consumed probiotics through food or through supplements. We recognize that the effects of probiotics may potentially differ when consumed as supplements versus through foods. However, excluding subjects exposed through probiotics through supplements did not change the results.
To measure depression we used the PHQ-9. Although in earlier studies, scores ≥10 had 88% sensitivity and specificity
19 for major depression, depression was not formally diagnosed by a mental health professional. Errors in depression classification could also lead to underestimation of the association between depression and probiotics.
We found that the higher the grams of fiber in the diet, the lower the odds of depression, and this finding persisted after adjustment. A meta-analysis of observational studies found that a diet based on high intake of fruit, vegetables, and whole grains, which translates into high fiber, was associated with lower risk of depression.
28 Dietary fiber is now considered more than a static collection of indigestible plant materials; it binds potential nutrients to prevent their absorption.
11,49 Fiber provides substrates for bacterial fermentation and therefore has the potential to change the composition of the gastrointestinal tract flora, promoting a shift toward different types of bacteria.
This large population-based study found that probiotic exposure is associated with a lower risk of depression only when the characteristics of the subjects exposed and unexposed to probiotics are not considered. Subjects exposed to probiotics are healthier and have fewer risk factors for developing depression than subjects who are not exposed to probiotics. In summary, this study found that use of probiotics is not associated with lower rates of depression.