The etiology of PSD is likely multifactorial, consistent with biopsychosocial models of mental illness,
3 but it remains unclear whether the lesion contributes directly to PSD by disrupting the brain’s mood regulation systems.
4 Idiopathic major depression is associated with dysfunction in the left dorsolateral prefrontal cortex (DLPFC),
5 as is late-life depression,
6,7 and depression associated with acute traumatic brain injury.
8 Correspondingly, a study of patients with bilateral DLPFC damage from various causes found increased rates of depression compared with patients with lesions elsewhere.
9 PSD has previously been associated with left frontal strokes,
10,11 particularly with increasing proximity to the left frontal pole.
12–14 However, these studies were primarily conducted during the first few months after stroke, during a period of acute adjustment to communication impairments and loss of dominant limb function in many left hemisphere stroke survivors. A meta-analysis examining lateralization of depression at different time points after stroke found that PSD was associated with left hemisphere strokes in the acute phase, but right hemisphere strokes in the chronic phase. This pattern is consistent with differential time courses of neuropsychological syndromes associated with the two hemispheres: resolution of catastrophic reaction and acute adjustment difficulties from aphasia in left hemisphere stroke, and a resolution of anosognosia with persistence of behavioral dysfunction in right hemisphere stroke.
4 This meta-analysis, and others,
15 have addressed the broad lateralization of depression symptoms to one hemisphere or the other, but have not examined specific localization within the hemispheres. However, some studies have found that within the left hemisphere, the association between anterior strokes and depression diminishes over time.
14,16,17 These studies were conducted before the era of modern lesion-symptom mapping
18 and used relatively coarse measures of localization (e.g., proximity to the frontal pole). These approaches may not be sensitive to lasting effects of specific damage to structures involved in mood regulation, including the left DLPFC, in the chronic phase after stroke.
Here, we use a new multivariate lesion-symptom mapping method
19 to localize depression symptoms within the left hemisphere with greater precision than these earlier studies. Based on the evidence in idiopathic major depression, we hypothesized that strokes of the left DLPFC should disrupt mood regulation systems, resulting in greater depression symptoms compared with other stroke locations, even in the chronic phase of recovery. Although most prior studies on localization of PSD have focused on earlier periods after stroke, testing in the chronic period is consistent with common lesion-symptom association approaches in cognitive neuropsychology, in which the necessity of a given brain structure for the function of interest is demonstrated through a persistent lesion-symptom association in the chronic phase, after adequate time for neuroplastic recovery.
20 Because our hypothesis was specifically lateralized to the left DLPFC, we restricted our investigation to survivors of left hemisphere stroke. These approaches are expected to provide a sensitive assessment to determine whether precise localization within the left hemisphere relates to depression symptoms in chronic stroke.
Results
As expected, participants overall reported relatively mild depression symptoms, with a median total SADQ score of 9/30 and maximum score of 19/30. There were no significant relationships with age, sex, stroke etiology, time since stroke, total stroke size, or antidepressant use, but there was a protective effect of education on depression symptoms (r=−0.40, p=0.01) (
Table 1).
Most of the participants had aphasia and many had cognitive deficits, which could impact depression ratings. We therefore examined relationships between SADQ scores and WAB-R scores, and the CLQT Attention and Executive domain scores. No significant relationships or trends were identified, and examination of scatter plots revealed no apparent nonlinear relationships.
There was an expected significant positive relationship between depression scores and self-reported physical disability (SAQOL physical score r=−0.35, p=0.03), but no relationship with self-reported functional communication disability (SAQOL communication score r=−0.12, p=0.45;
Table 1).
Next, the demographic, deficit, and disability measures in
Table 1 were entered into a stepwise linear regression with SADQ scores as the dependent variable. Only education survived in the model as predictive of depression symptoms (model, F(1,37)=6.83, p=0.013; standardized beta for education=−0.395, t(37)=−2.61, p=0.013).
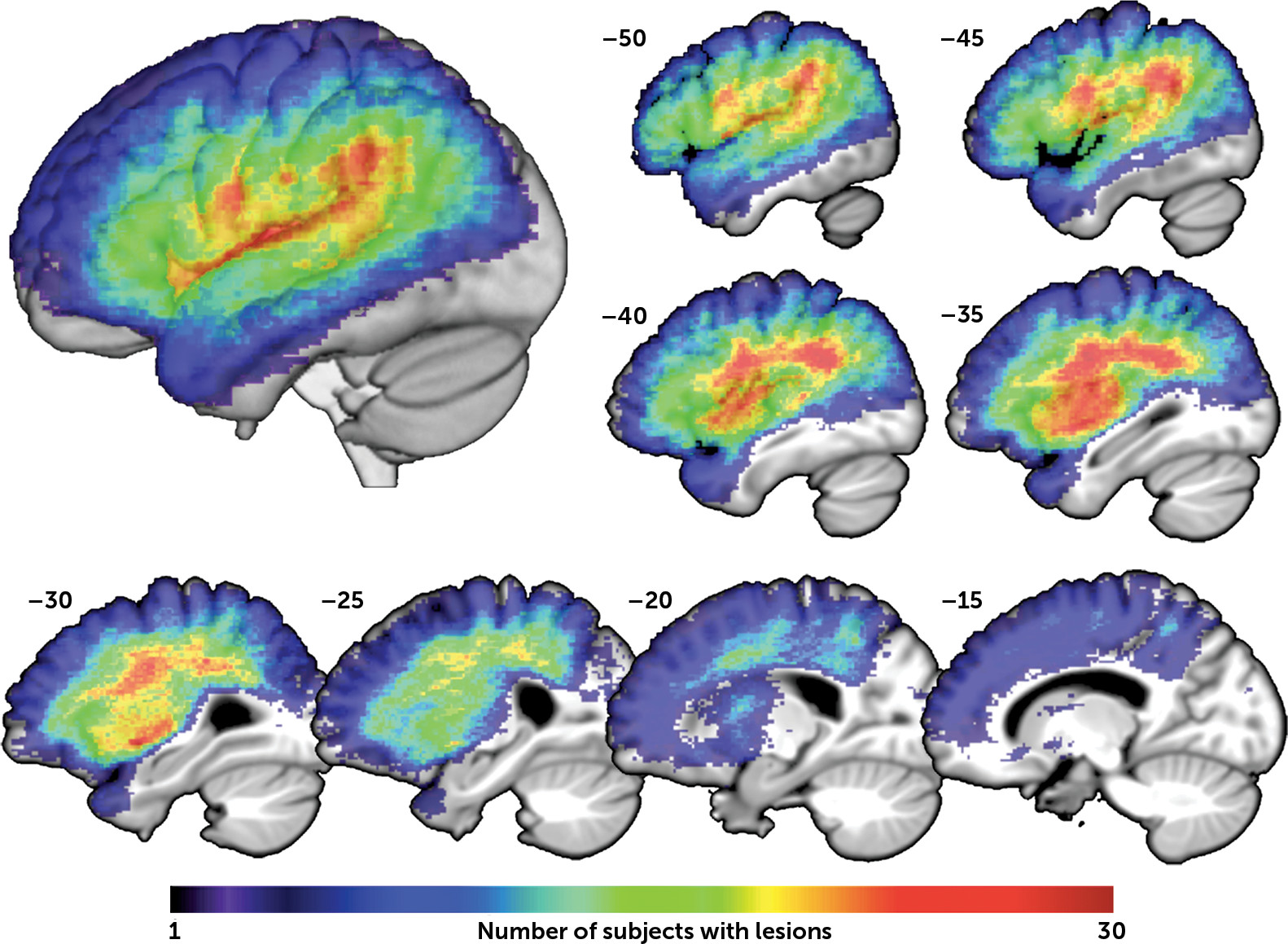
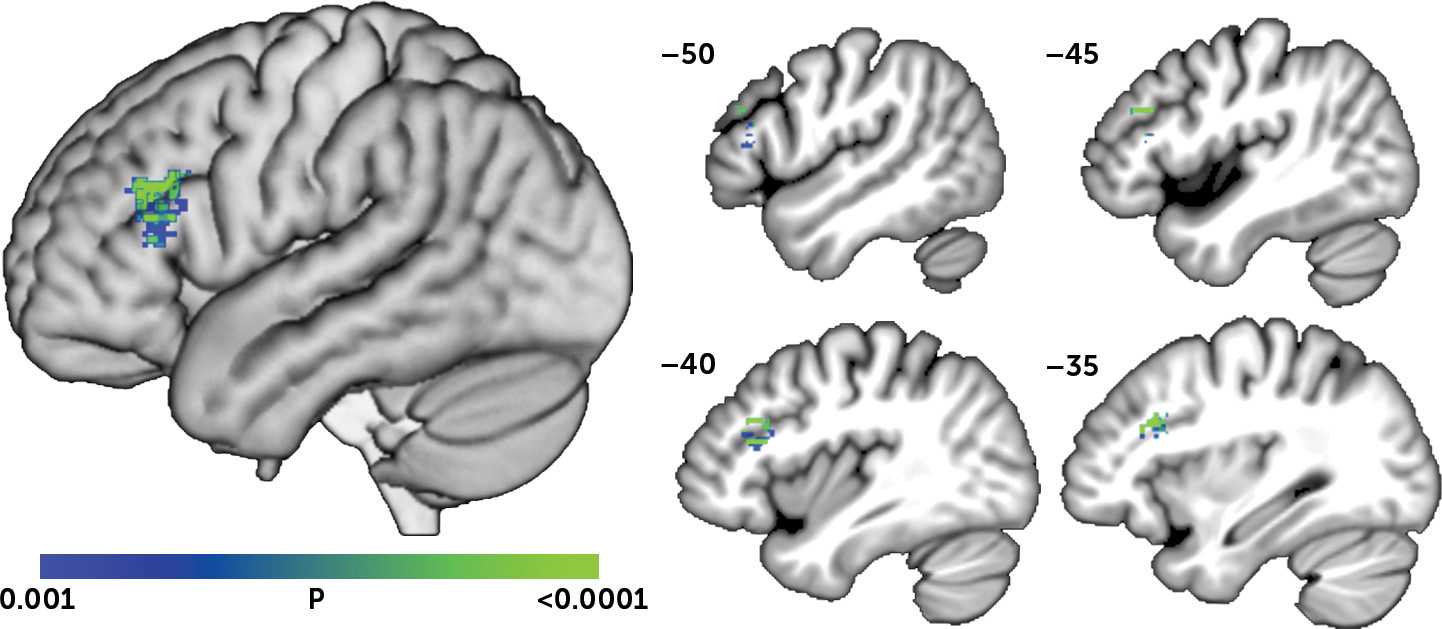
SVR-LSM was then used to determine if SADQ scores related to lesion location. To account for the relationship between education and depression symptoms, we performed the SVR-LSM analysis using the residual SADQ score after regressing out education. The SVR-LSM analysis identified a single significant cluster centered in the left DLPFC in which lesions were associated with greater depression symptoms (
Figure 2; volume=1,235 mm
3; peak MNI coordinates=−33, 21, 26; center=−42, 26, 20). There were no areas in which lesions related to lower SADQ scores.
Since patients with moderate-severe comprehension deficits would typically be excluded from a study like this one, we next tested the relationship between SADQ scores and DLPFC damage independently in patients with moderate-severe and mild-to-no comprehension deficits. Independent ANOVAs demonstrated that, controlling for education and total lesion volume, SADQ scores related to DLPFC damage (>1/2 of the voxels in the SVR-LSM cluster lesioned) in both groups (moderate-severe comprehension deficit group, F(1,8)=17.09, p=0.003; mild-to-no comprehension deficit group, F(1,23)=9.49, p=0.005).
Discussion
Using a new multivariate lesion-symptom mapping method, we found that lesions in the DLPFC were associated with increased depression symptoms in chronic left hemisphere stroke survivors. These results correspond with prior evidence that left frontal strokes are associated with PSD,
10–14,17 and with prior evidence that DLPFC damage from other causes relates to depression symptoms.
6,8,9 This study extends these findings by demonstrating a precise localization of the effect within the left DLPFC using an advanced imaging analysis method.
Dysfunction of the left DLPFC has previously been implicated in major depression by studies using a variety of experimental methods.
27 The left DLPFC is thought to control negative affect through contextual processing and reappraisal/suppression strategies, and is hypoactive in functional imaging studies of individuals with major depression,
5 particularly during emotional judgment tasks.
28 Moreover, excitation of the left DLPFC using high-frequency repetitive transcranial magnetic stimulation improves depression and is now cleared by the U.S. Food and Drug Administration for adjunctive treatment of major depression.
29,30 Considering the convergence between these findings on major depression and the results of the current study on poststroke depression symptoms, it seems that both may share a common pathophysiological mechanism, at least with regard to the contributions of left DLPFC dysfunction. This convergence also provides support for the use of lesion studies to understand the neuroanatomy of major depression, and lends credence to the notion that some brain stimulation treatments for major depression may also be useful for PSD.
31The question of whether lesion location contributes to PSD has been controversial, with prior studies often providing conflicting results or revealing no association at all.
32 This lack of consistency has likely arisen from variation in experimental parameters, including the measurement instruments, the populations examined, and the timing and setting of the testing.
3,4,33 In addition, most prior studies have used fairly coarse methods to localize and categorize lesions, with only two recent studies using modern lesion-symptom mapping approaches. One of these recent studies used graph theory analysis of diffusion tensor imaging data to demonstrate that damage within a broad “depression-related network” was associated with increased rates of PSD.
34 The other recent notable study used a univariate voxel-wise approach with T1-weighted images, and failed to find a relationship between lesion location and PSD in a cohort of 55 subacute stroke survivors with left, right, or bilateral strokes.
35 The authors attribute the negative results to methodological limitations, primarily an overly diverse group of participants who did not have sufficient overlap in lesion locations to provide adequate power for lesion-symptom mapping.
Aside from using a more sensitive multivariate lesion-symptom mapping method than this recent study,
19 we also restricted our analysis to left hemisphere stroke survivors only, providing more overlap of lesions in our group and higher power for lesion-symptom mapping. We also examined patients in the chronic phase of recovery, which may have provided sufficient time for normal grief and adjustment responses to resolve, yielding greater specificity for neurologically driven depression symptoms in our measurements. Because aphasia is a common complicating factor in prior studies of PSD, and aphasia occurs in most left hemisphere stroke survivors,
36 we also used a different measure of depression symptoms, the SADQ, which was designed for use in stroke survivors with aphasia (however, see the discussion of the limitations of this instrument, below). Moreover, we performed detailed aphasia and cognitive testing to rule out any impact of these deficits on depression symptom ratings prior to examining relationships between depression symptoms and lesion location. Finally, whereas most prior studies investigating localization of PSD have examined lesion location in relation to diagnosis of PSD, we instead examined lesion location in relation to the continuous score on the SADQ, i.e., symptoms of depression, not diagnosis of PSD. This approach acknowledges that depression symptoms after stroke occur on a continuum
37 and likely provided greater statistical power in the lesion-symptom mapping analysis, at the cost of reducing our ability to determine whether findings are clinically significant.
In addition to the contribution of left DLPFC damage to depression symptoms, we also confirmed prior evidence that physical disability relates to depression,
1 and identified a protective influence of education. This latter result has not been widely identified in other studies of PSD. However, lower education and correspondingly lower socioeconomic status is associated with higher rates of depression in the general population,
38 as well as lower likelihoods of seeking mental health services in older adults.
39 Level of education in our sample likely serves as a surrogate marker for socioeconomic status and consequently access to support services or social support networks, which help to mitigate PSD symptoms.
40Some limitations of this study are worth noting. First, the SADQ was selected as the measure of depression symptoms to facilitate the inclusion of participants with comprehension deficits. Most prior studies of PSD have excluded these individuals because there are no adequate measures to assess depression in this group. Indeed, the validity of the SADQ has never been clearly established. Furthermore, because the SADQ is administered to caregivers, it lacks questions about the patient’s subjective experience of sadness, which is critical to the diagnosis of depression. One might reasonably question whether the localization observed here truly relates to depression versus other symptoms measured by the SADQ. We are somewhat reassured by our results, however, which are consistent with those of many prior studies on PSD that excluded people with comprehension deficits and used better-validated depression measures. As such, we suggest that despite the significant limitations associated with using the SADQ, our results tentatively fill a gap in the literature by suggesting that the localization of PSD observed in other studies may generalize to stroke survivors with comprehension deficits.
Other limitations include the sample size, which may not have provided sensitivity to detect all possible lesion-symptom relationships. Our analysis is only sensitive to effects in a restricted part of the brain, as shown in
Figure 2. The context in which the study was conducted made some standard measures such as the National Institutes of Health Stroke Scale unavailable. Although we excluded individuals with a history of severe psychiatric illness, we did not assess premorbid depression symptoms. The lack of premorbid depression assessment is unlikely to have produced a false-positive lesion-symptom mapping result, but poststroke depression is strongly related to premorbid depression, and its occurrence in this context may relate differently to lesion location. Functional disability was mainly measured using self-report scales, which could be influenced by anosognosia. It should also be noted that overall scores on the SADQ were fairly low in our sample, consistent with prior evidence that chronic left hemisphere stroke in general is not associated with PSD.
4,15 Thus, while the current study demonstrates a direct neurological effect of left DLPFC damage on depression symptoms, the clinical importance of the effect to the occurrence or severity of PSD remains unclear.
In summary, we used a new multivariate lesion-symptom mapping method to examine localization of depression symptoms in chronic left hemisphere stroke survivors, and found that lesions of the left DLPFC are related to increased depression symptoms. These results provide evidence of convergent biological mechanisms for poststroke depression symptoms and major depression, and demonstrate a direct neurological contribution to depression symptoms after left hemisphere stroke.